In the advanced stage of chronic obstructive pulmonary disease (COPD), bilateral lung trans plantation has been shown to improve mortal ity rates1. In countries with limited availability of organ donations, single lung transplantation (SLT) has been found to be a valid alternative to enhance survival rates2. According to data re ported by the Instituto Nacional Central Único Co ordinador de Ablación e Implante (INCUCAI), dur ing the last twenty years (from 2003 to 2023) in Argentina, a total of 613 lung transplants were performed, with 292 of them being SLT (47.6%) and 321 bilateral lung transplants (52.4%)3.
However, the postoperative management of SLT poses an additional challenge due to the dis tinct compliance of each lung, leading to compli cations such as hyperinflation of the native lung and heterogeneous distribution of ventilation4,5. During the weaning process from invasive me chanical ventilation (iMV), the use of high-flow oxygen therapy (HFOT) offers several advantag es, including improved oxygenation, increased end-expiratory lung volume, and reduced work of breathing6. HFOT has also demonstrated low er intubation rates in patients with hypoxemic respiratory failure and comparable efficacy to non-invasive ventilation in preventing post-ex tubation respiratory failure7. However, the spe cific benefits of HFOT in SLT patients have not been clearly established.
To assess the impact of HFOT on each lung individually in these patients, electrical imped ance tomography (EIT) proves to be a valuable tool by providing regional assessments of lung aeration8,9. EIT is a non-invasive medical imag ing technique used to generate real-time images, providing valuable insights into the distribution of electrical thoracic impedance and allowing inference of lung ventilation and aeration.
We present a case report of a 65-year-old male patient who underwent SLT and was in the weaning period from iMV. In this case, we mea sured the physiological effect of HFOT using EIT.
Clinical case
We present the case of a 65-year-old male patient who was admitted to the intensive care unit for left SLT. The patient had a history of COPD and had been on the transplant waiting list for two years, with a BODE index of 8. Pulmonary function tests showed air entrapment and increased expiratory resistances. Postoperatively, the patient required prolonged iMV, and a tracheostomy was performed. During the weaning process, the attending team discussed whether the use of HFOT could prolong spontaneous ventilation periods in order to reduce the iMV time. To assess lung aeration in real time we used EIT.
The measurements were conducted with the patient in a semi-seated position, with the head elevated at 30°. A 16-electrode EIT belt (FluxMED, MBMed, Buenos Aires, Argentina) was positioned between the 4th and 5th inter costal space. The impedance units, referred to as Arbitrary Units (AU), represented volume. HFOT was administered using the Airvo2 system (Fisher & Paykel Healthcare, New Zealand) at a flow rate of 50 L/min and a temperature range of 34-37 °C. The fraction of inspired oxygen (FiO2) level was titrated to maintain peripheral oxygen satura tion (SpO2) above 92%. Vital signs were also monitored. Informed consent from the patient was obtained.
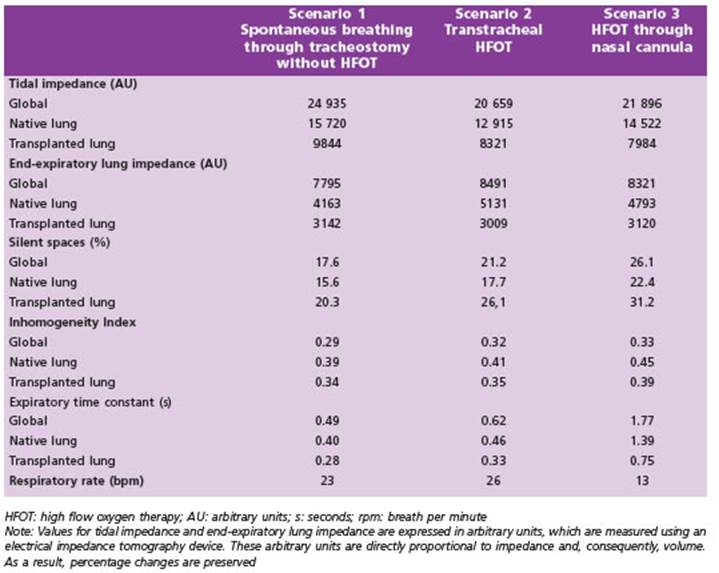
We conducted evaluations of lung impedance in three different spontaneous breathing scenarios: through a tracheostomy tube without HFOT (scenario 1), applying transtracheal HFOT (scenario 2), and using HFOT through nasal cannula (scenario 3). The results of the EIT mea surements are summarized in Table 1.
In scenario 1, we observed an inhomogeneous distri bution of ventilation among lungs. Tidal impedance (TZ), which reflects the variations in lung aeration and venti lation during a tidal breath, demonstrated that the gas distribution was higher in the native lung. TZ in the na tive lung represented 61.5% of the global TZ. Also, the global inhomogeneity (GI) index was 0.29. The GI index is a parameter used to represent the spatial extent and dispersion in the distribution of tidal breath in each lung in comparison with global ventilation. It ranges from 0, which represents a perfect homogeneous distribution of ventilation, to 1, indicating a completely inhomogeneous distribution of ventilation. Finally, end expiratory lung impedance (EELI) was almost symmetrical. EELI is use ful to assess changes in end-expiratory lung volume, for example after changing the positive end-expiratory pres sure or after recruitment maneuvers for the reopening of dorsal atelectasis as well as for the detection of de-recruitment of individual lung areas.
When comparing scenario 2 (applying transtracheal HFOT) vs. scenario 1 (breathing through a tracheostomy without HFOT), we observed a decrease native lung TZ and transplanted lung TZ (-17.8 and -15.5%, respectively), an increase in native lung EELI (+23.3%), without relevant changes in the transplanted lung EELI. The application of transtracheal HFOT exacerbated the inhomogeneity of air distribution (GI index +9.48%), extending regional expiratory time constant of the native lung (+15%) and in creasing in silents spaces (17,6% in scenario 1 and 21,2% in scenario 2). Expiratory time constants represent the time required for the respiratory system to reach 63% of its equilibrium value and is an indication of the time re quired for the lungs to empty during exhalation. There fore, a shorter time constant suggests a faster emptying process, while a longer time constant indicates a slower emptying process. Additionally, silent spaces refer to lung regions that exhibit an impedance change of less than 10%, indicating poor ventilation. Through silent spaces analysis, valuable information can be obtained regarding lung areas that experience limited airflow during tidal breathing, leading to hypoventilation. If these regions are situated at the lower portions of the lungs (dependent areas), there is a possibility that they may be collapsed, or be filled with fluid. Conversely, when these areas are located in the upper regions of the lungs, it is more prob able that they are already distended, potentially even overdistended.
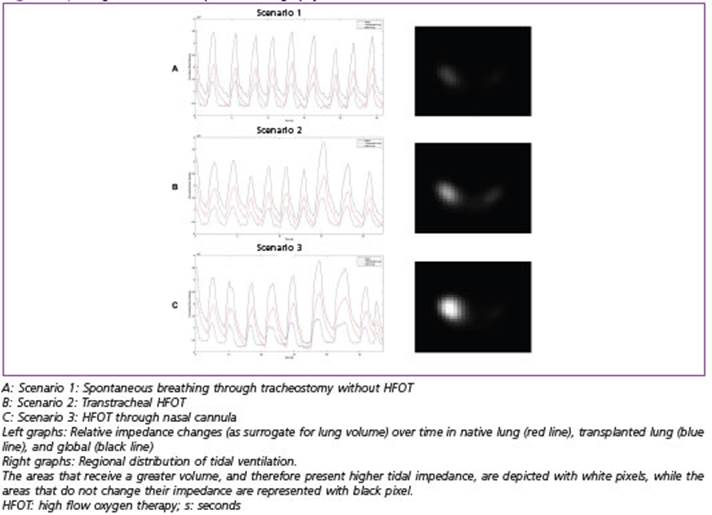
In scenario 3, the application of HFOT through nasal cannula produced a global and regional decrease in TZ in comparison with spontaneous breathing through a tracheostomy without HFOT (-12.2% for global TZ, -7.6% in native lung, and -18.9% in transplanted lung). Also an increase in global EELI, with greater expression in the na tive lung was observed (+6.75% in global EELI and +15.1% in native lung EELI), without major changes in the trans planted lung EELI. The GI index increased 11.5% as well as expiratory time constants. Finally, silent spaces increased when applying HFOT through the nasal cannula (21,2% in scenario 2 and 26,1% in scenario 3). In addition, applying HFOT had a relevant impact on decreasing the respira tory rate. Figure 1 shows the changes in EIT in different scenarios (these changes are also illustrated in Supple mentary material: Video).
After conducting EIT measurements, we concluded that the application of HFOT resulted in increased air trapping and overdistention of the native lung, without yielding any benefits for the transplanted lung. As a re sult, we decided to proceed with the conventional iMV weaning strategy, which involved periodic intervals of spontaneous ventilation through tracheostomy without HFOT. The patient successfully completed the weaning process after 23 days of iMV and was subsequently dis charged from the intensive care unit 42 days after being admitted to the hospital.
Discussion
Monitoring of pulmonary ventilation by EIT showed that the application of HFOT during the weaning period of iMV in this patient increased air trapping in the native lung with no benefit in the transplanted lung.
In scenario 1, during spontaneous breathing through a tracheostomy, the analysis of region al expiratory airflow in the native lung showed elevated expiratory time constants, which re sulted in a heterogeneous air distribution due to gas trapping. However, the EELI remained sym metrical. This can be explained because the EELI represents a situation in which the expiratory flow is zero, so the pressure in both lungs are in a state of equilibrium. When HFOT was ap plied either through a tracheostomy (scenario 2) or nasally (scenario 3), the global distribution of ventilation became more heterogeneous, due to global and regional increase in EELI with greater expression in the native lung. After HFOT appli cation in scenario 3, TZ decreased globally and regionally. Respiratory rate dropped abruptly, but gas trapping worsened, particularly in the native lung, evident by increased EELI, expira tory time constants, and silent spaces10. In the transplanted lung, TZ drop indicated hypoven tilation with increased regional silent spaces, while EELI and expiratory time constants re mained unchanged.
Measurements provided by EIT aimed to as sess regional pulmonary aeration, and avoid hyperinflation in a thoracic-pulmonary system composed of lungs with different elastic and resistive properties due to a combination of a proportional increase in tidal volume (because of low lung elastance) and the phenomenon of expiratory flow limitation due to high airway re sistance11. In extreme cases, air trapping in the native lung can produce a limitation of the ex pansion of the transplanted lung, called medias tinal shift, with the consequent decrease in the functional residual capacity, which can predis pose to hypoxemia and increased iMV time12-14.
Physiological effects reported were observed in only one patient, so we cannot extrapolate the results to all patients with SLT. Prospective studies with a large cohort of patients will be re quired to confirm this finding.