KEY POINTS
Current knowledge
• Coronavirus disease 2019 (COVID-19) pandemic poses a major challenge for healthcare systems. In South America, local information about the incidence and clini cal characteristics of critically ill patients diagnosed with COVID-19 is still limited.
Article´s contribution to knowledge
• The most frequent comorbidity was arterial hypertension, affecting 52.4% of 168 patients, followed by obesity in 41.6% (70).
• A 67.9% required invasive mechanical ventilation.
• The length of stay in the ICU was 13 days (6-24) and the mortality in the ICU was 25%.
In December 2019, a new coronavirus was identified by the Chinese Center for Disease Control and Prevention. On March 11th of 2020, the World Health Organization (WHO) declared the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outbreak as a pandemic due to the constantly increasing number of cases outside China1. Up to date, SARS-CoV-2 affected more than 32 million people over the world and caused 1 million deaths.
On March 3rd, 2020, 64 days after the first case was reported in China, a case in Argentina was confirmed. Since then, the number of cases gently ascended2; up to September 30th, 2020, a total of 736 609 had tested posi tive for the new SARS-CoV-2, with 139 419 active cases, and 3792 (2.7%) admitted to intensive care unit (ICU)3.
Nevertheless, local information about the incidence and clinical characteristics of critically ill patients diagnosed with COVID-19 is still limited4. In this context, knowledge of critically ill patients’ baseline characteristics and outcomes is crucial for health and government officials engaged in planning efforts to address local outbreaks. This case series describes clinical characteristics, image findings and respiratory mechanics of COVID-19 patients admit ted to ICU in a high complexity hospital in Buenos Aires.
Materials and methods
For this retrospective single-center study, ICU patients were recruited between March 15th, 2020 and September 15th, 2020. Data were obtained from medical records of adult patients (18 years of age or older) with laboratory-confirmed COVID-19 hospitalized in the ICU in a high complexity hospital in Buenos Aires. Those with adequacy of the therapeutic effort at ICU admission were excluded.
According to WHO guidance5, laboratory confirmation for SARS-CoV-2 was obtained as a positive result of real-time reverse transcriptase-polymerase chain reaction (RT-PCR) assay of nasopharyngeal swabs. Only laboratory-confirmed cases were included in the analysis, and the Hospital Ethics Committee approved the study in March 2019. Epidemiologi cal, demographic, clinical, laboratory, respiratory support, and outcome data were obtained. Radiologic assessment of chest x-rays and all laboratory testing was performed according to the treating physician criteria. The presence of a radiologic ab normality was determined and the Radiographic Assessment of Lung Edema (RALE) score6 was calculated and reviewed by medical imaging specialists. Laboratory assessment con sisted of a complete blood count, a blood chemical analysis, coagulation testing, assessment of liver and renal function, and measure of electrolytes, C-reactive protein (CRP), pro calcitonin, pro b-type natriuretic peptide (pro-BNP), lactate dehydrogenase, high-sensitivity cardiac troponin (hs-cTnT), d-dimer, ferritin and interleukin-6 (IL-6).
The number of patients who died or been discharged, and those that stayed in ICU until September 30th of 2020 was recorded. Additionally, ICU length of stay was determined.
No statistical sample size calculation was performed in advance and the sample size was equal to the number of patients treated during the study period. Continuous variables were expressed as medians and interquartile ranges or simple ranges, as appropriate. Categorical variables were summa rized as counts and percentages.
No imputation was made for missing data. Mann-Whitney rank-sum test was used to compare nonparametric continu ous variables. χ2 or Fisher exact test was used for categorical variables as appropriate. All statistical tests were 2-tailed, and statistical significance was defined as p < .05. The analysis has not been adjusted for multiple comparisons, and given the possibility of a type I error, the findings should be inter preted as exploratory and descriptive. All the analyses were performed using R Software, version 3.6.2 (R Foundation for Statistical Computing).
Results
Between March 15th and September 15th of 2020, a total of 259 patients with suspected COVID-19 were referred to the ICU. A total of 87 with negative test results for SARS-CoV-2 were not included in the study. Additionally, four with laboratory-confirmed COVID-19 but without the adequacy of therapeutic effort at ICU admission were excluded. Thus, data from 168 critically ill patients with laboratory-confirmed COVID-19 was analyzed.
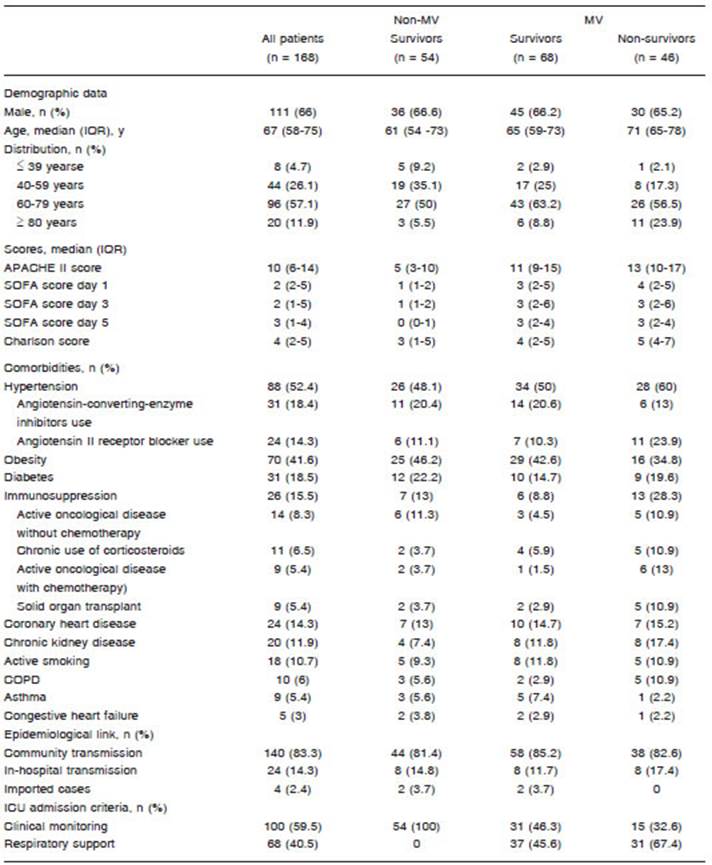
Overall, 66% (111) patients were male, with a median age of 67 (58-75). Eighty percent (134) presented at least one comorbidity. Hypertension was the most common comorbidity, affecting 52.4% (88), followed by obesity in 41.6% (70). The 6.5% (11) admitted were health-care workers. Table 1 shows the demographic and clinical characteristics of the patients.
The median (IQR) time between symptoms onset and hospital admission was 4 days (2-7). Fever was referred by 91.1% (153) followed by shortness of breath (52.4% [88]). The main ICU admission criteria were clinical monitoring (59.5% [100]), and 40.5% (68) needed MV at ICU arrival. The median time up to ICU admission was seven days (4-9) since symptoms onset.
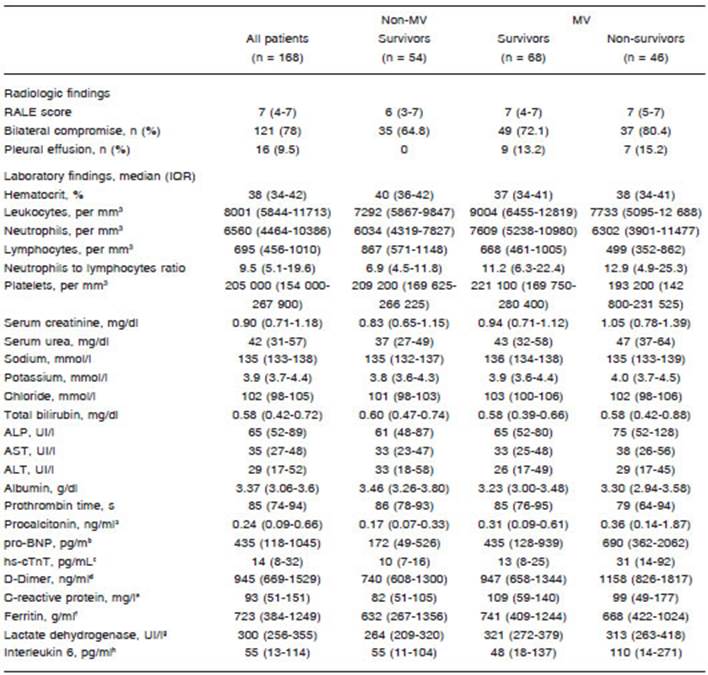
All patients had chest x-rays at ICU admission, 98.2% (165) revealed abnormal results. The most common pat tern on chest x-rays was patchy bilateral shadowing in 72% (121) with a median (IQR) RALE score of 7 (4-7). The presence of pleural effusion was infrequent (9.5% [16] of chest x-rays).
On ICU admission, lymphocytopenia was present in 73.2% (123), thrombocytopenia in 19.6% (33), and leu kopenia in 6.5% (11).
Among mechanical ventilation (MV) survivors and MV non-survivors, no difference was found in total leukocyte count (median [IQR], 7292 mm3 [5867-9847] in MV sur vivors vs. 9004 mm3 [6455-12 819] in MV non-survivors; p = 0.1313) nor absolute neutrophil count (median [IQR], 6034 mm3 [4319-7827] in MV survivors vs. 7609 mm3 [5238-10 980] in MV non-survivors; p = 0.3366).
Regarding lymphocytes, absolute cell count was sig nificantly higher among non-MV patients than MV patients (median [IQR], 867 mm3 [571-1148] vs. 668 mm3 [461- 1005]; p = 0.0042), and also, a significantly higher count was registered in MV survivors than MV non-survivors (499 mm3 in non-MV [352-862]; p = 0.0294).
Neutrophil to lymphocyte ratio (NLR) was higher among non-MV patients than MV survivors in ventilated vs. non-ventilated (median [IQR], 6.9 [4.5-11.8] vs. 11.3 [5.5-24.2]; p = 0.0059) but non difference was found between MV survivors vs. MV non-survivors (median [IQR], 11,2 [6,3- 22,4] vs. 12,9 [4,9-25,3]; p = 0.9913).
The majority of patients had elevated levels of inflam matory biomarkers like CRP, ferritin and IL-6. ProBNP was higher among ventilated vs. non-ventilated (median [IQR], 520 pg/ml [199-1189] vs. 172 [49-526]; p = 0.0004). Also, among overall, non-surviving patients had more prominent laboratory abnormalities including proBNP and d-dimer than survivors (median [IQR], 690 pg/ml [362-2062] vs. 435 pg/ml [128-939]; p = 0.0106 and 1158 ng/ml [826-1817] vs. ng/ml 818 [618-1305]; p = 0.0097). Table 2 shows the radiologic and laboratory findings at ICU admission. Figure 1 shows laboratory results among non-MV, patients, MV survivors and MV non-survivors.
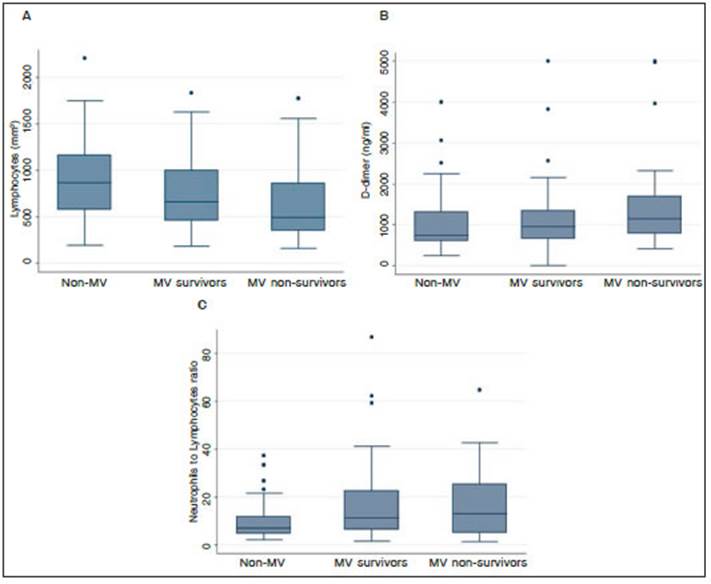
Fig. 1 Laboratory results among non-mechanically ventilated (non-MV) patients, MV survivors and MV non-survivors of. A: lymphocytes (per mm3). B: D-dimer (ng/ml). C: neutrophils to lymphocytes ratio
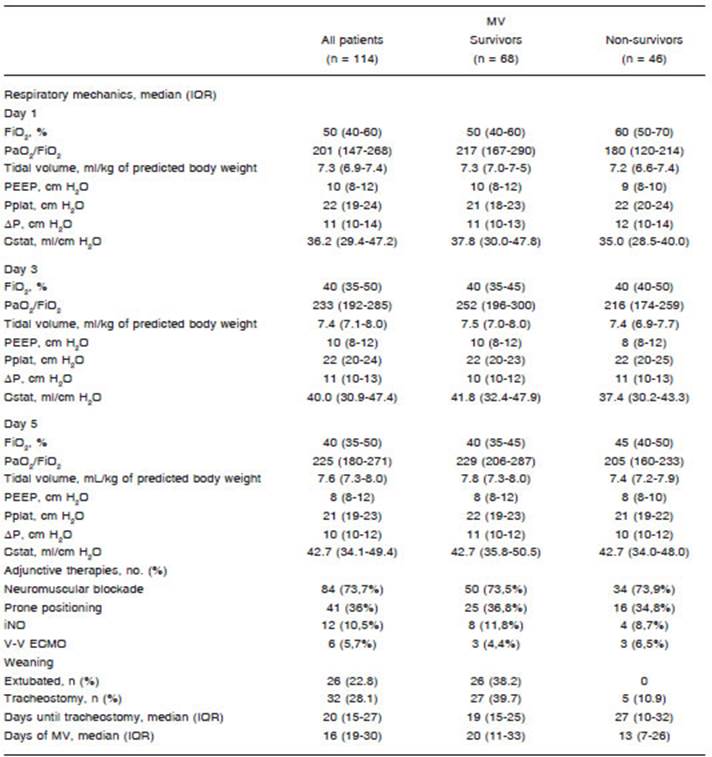
A total of 114 patients (67.9%) required endotracheal intubation and invasive MV. No one was treated with noninvasive ventilation. On the first day of MV, the median positive end-expiratory pressure (PEEP) was 10 (8-11) cm H2O. PEEP levels as high as 16 cm H2O were ap plied. Among a total of 114 patients, 75 (65.7%) required a fraction of inspired oxygen (FIO2) of at least 50%, and 11 (9.4%) required 100% FIO2. The median PaO2/FIO2 ratio was 200 (IQR, 147-268). Also, lower PaO2/FIO2 ratios on the first day of MV were registered among non-survivors vs. survivors (median [IQR], 180 [120-214] vs. 216 [167-290]; p = 0.0309). All MV patients fulfilled Berlin criteria for Acute respiratory distress syndrome (ARDS)7.
Regarding respiratory mechanics, the median plateau pressure (Pplat) on the first day of MV was 22 (19-24) cm H2O, the median driving pressure (ΔP) was 11 (10-14) cm H2O and the median respiratory system compliance (Crs) was 36 (30-47) ml/cm H2O.
A majority of the mechanically ventilated patients (84 [73.7%]) required neuromuscular blockade due to se vere hypoxemia to avoid patient-ventilator asynchronies. Also, prone position ventilation was applied to 41 (36%), and 36.1% of them (15) required more than one prone positioning session. Twelve patients (10.5%) received inhaled nitric oxide (iNO) and 6 (5.7%) were connected to veno-venous extracorporeal membrane oxygenation (V-V ECMO) because of refractory hypoxemia.
The time elapsed of MV was 16 days (19-30) among overall ventilated patients and 8 days (6-14) among those who were successfully extubated (26 [22.8%]). Thirty-two patients (28.1%) underwent percutaneous tracheostomy due to prolonged weaning. The median time of MV until tracheostomy was 20 days (15-27); 10 patients (8.7%) remained under MV at data cut off. Table 3 shows respira tory mechanics, oxygenation parameters and adjunctive therapies applied.
Most of the patients received dexamethasone (on RECOVERY-trial dose8) and empirical intravenous antibi otic therapy (143 [85.1%] and 133 [79.2%], respectively). Ninety patients (53.6%) were included in a 2:1 blinded-protocol of convalescent plasma against placebo. Other treatments like ritonavir/lopinavir (23 [13.7%]) and tocili zumab (3 [1.8%]) were less frequently applied.
A common ICU related complication was delirium that was identified in 121 patients (72%) overall. Delirium was less present among non-ventilated (23 [42.5%]) in comparison with ventilated that survived (61 [89.7%]) and those who died (37 [80.4%]). Other complications registered were catheter-related sepsis (23 [13.7%]), pressure ulcers (17 [20.1%]), urosepsis (10 [6%]) and ventilator-associated pneumonia (11 [6.5%])
Among overall patients, the median duration of hospi talization was 21 days (14-32) and the median length of stay in ICU was 13 days (6-24). ICU length of stay among survivors was 5 days (3-8) for non-ventilated patients and 23 days (16-31) for those who required invasive MV. Overall ICU mortality of this series was 25% (42). Table 4 shows treatments, ICU related complications, and clinical outcomes at data cutoff.
Discussion
The population in this study mainly consisted of men (66%) with a median age of 67 (58-75) years, which is substantially high compared to the median age of all the positive Argentinian cases of COVID-19 (38 years old)9. The previous suggests that gender and age are risk fac tors for admission to the ICU, as previously reported10. Moreover, in this cohort, most of the patients (79.7%) had at least one comorbidity, with a large proportion with hypertension (52.4%) and obesity (41,6%).
In this case series, most patients were admitted to the ICU because of acute hypoxemic respiratory failure that required clinical monitoring. A substantial proportion of patients needed respiratory support and endotracheal intubation at ICU arrival. Endotracheal intubation and invasive MV were needed in 67.9%, whereas only 32.1% could be managed with oxygen delivery by a non-rebreather mask. Setting primary focus on health-care personnel security, no patient received non-invasive MV (eg. continuous positive airway pressure, non-invasive positive pressure ventilation, or high flow nasal can nula) due to the risk of aerosol dispersion11. There is still controversy regarding the efficacy of non-invasive MV devices to avoid endotracheal intubation12 but the need for invasive MV in this patient population under study was similar to other ICUs where non-invasive MV was applied: 65% (São Paulo, Brazil)13, 71% (Washington State, USA)14, 71% (Wuhan, China)15, 80.8% (Detroit, USA)16, 88% (Lombardy region, Italy)17, 96.7% (Mexico City, Mexico)18.
Among ventilated patients, 44.7% (51) presented paO2/FiO2 lower than 200 on the first day of MV, although pulmonary mechanics were almost normal (median Pplat 22 cm H2O [19-24] and median ΔP 11 cm H2O [10-14]). Nevertheless, 79.8% (91) had low Crs(<50 ml/cm H2O) with a median Crs of 36 ml/cm H2O (30-47) despite of lung-protective ventilation (tidal volume ≤ 8 ml/kg pre dicted body-weight). These findings are in accordance with information that reported that COVID-19 ARDS re spiratory features are similar to non-COVID-19 ARDS19. Additionally, the values of Crs, Pplat, and ΔP were very similar to previously published cohorts of non-COVID-19 ARDS patients20.
Due to refractory hypoxemia, six patients (5.7%) were connected to V-V ECMO. Despite the middle-income country circumstances and the low volume of the ECMO program patients, outcomes are comparable to interna tional series. ECMO survival and survival to discharge was 66% and 50%, respectively21-23.
Since patients required MV for an extended period time due to prolonged weaning, there were more than under went percutaneous tracheostomy compared to those who were successfully extubated (32 [28.1%] and 26 [22.8%], respectively). At the beginning of the pandemic, several scientific societies warned about a possible increase in the request for tracheostomies related to SARS-CoV-2 infection24-26,29. The need for tracheostomies in critically ill COVID-19 patients ranges from 36% to 53%, according to the data found in the literature27-29.
Prioritizing the protection of health personnel, tra cheostomy was considered possible only in those who were expected to obtain a substantial benefit. Ideally, it was performed 21 days after intubation with a negative RT-PCR test30. Following that criteria and up to data cut off, none of the surgeons or intensivists who performed tracheostomies developed symptoms or tested positive for COVID-19. Nevertheless, a longer time of MV prior to tracheostomy was observed in relation to a previous series from the same center in a non-pandemic scenario (median 20 days [15-27] and 9 days [6-12], respectively)31.
ICU mortality rate was slightly lower than a recent systematic review and meta‐analysis of observational studies that informed a 41.6% (34.0-49.7) ICU mortality rate across international studies. This could be explained because, optimistically, countries in the later phase of the pandemic may be coping better with COVID-1932.
Although this study is considered limited due to the relatively small number of patients from a single center and could not be broadly applicable to other patients with a critical illness, it provides initial experience regarding characteristics of COVID-19 in those with critical illness in Argentina.