Metastatic lesions affecting the breast are excep tional, accounting for 0.2 to 1.3% of all the malignant tumors that affect this organ1. The most frequently reported histological types in case series of metastatic cancers are melanomas, hematolymphoid neoplasias, lung, prostate, ovarian, kidney, stomach and neuroendocrine tumors1-3.
The prevalence of hematolymphoid neoplasias infil trating the mammary tissue ranges between 0.04%4 and 1.6%2 with an annual incidence of 0.07% mainly account ted for by secondary lymphomas5. Ninety six percent of the cases appear in women aged between 60 and 70 at the time of the diagnosis and 80% of these are diffuse large B cells lymphomas, followed by follicular lymphoma and marginal zone lymphoma4,6,7. We present a patient with secondary involvement of both breasts by follicular lymphoma, this clinical condition being very unusual in scientific literature reports2,6.
Clinical case
A 60 year-old woman came to the clinic reporting bilateral, fast-growing mammary nodules that caused mild breast tenderness. She had a pathologic history of follicular lym phoma diagnosed 12 months before, which presented as a 6.5 × 5 cm mass, right perirenal location, associated to right retroperitoneal and inguinal lymph nodes, without bone marrow infiltration.
In the paraclinical testing hemoglobin level was 12.5 mg/ dL and lactate dehydrogenase (LDH) level was 205 u/L. It was initially staged as IIE of the Lugano classification and low risk according to the Follicular Lymphoma International Prognostic Index (FLIPI). The chemotherapy protocol was started with rituximab plus cyclophosphamide, doxorubicin, vincristine and prednisolone (CHOP), then maintenance with rituximab 375 mg/m2 every 8 weeks with partial response.
In the current physical exam, a nodular lesion was palpated in the lower inner quadrant of the right breast, firm consis tency, slightly tender to the touch, with no evidence of skin changes or nipple retraction. Two masses were found in the left breast, located in the upper outer quadrant and the lower outer quadrant with morphological features similar to those described in the contralateral breast.
A bilateral mammogram was obtained, which reported the presence of a nodule in the right breast, with smooth edges and clear boundaries, while in the left breast radi opaque and circumscribed nodules were noted; both lesions were categorized IVB according to the Breast Imaging Reporting and Data System (BIRADS), and interpreted as suspicious findings (Fig. 1). In the ultrasound a 4.5 cm mi cro lobulated, heterogeneous mass was defined in the right breast and two similar nodules in the left breast measuring 1.2 cm in diameter, average. No axillary lymphadenopathies were identified.
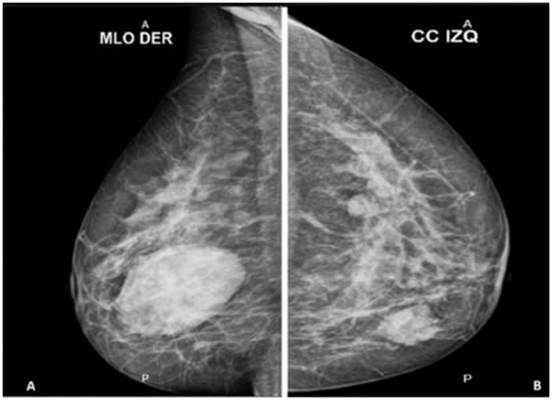
Fig. 1 A: Right breast mammogram evidencing in the lower inner quadrant a nodule with smooth edges and clear boundaries, BIRADS IV B, B: In the left breast, radiopaque, circumscribed nodules are identified at 5 cm. between 12 and 4 o’clock, BIRADS IV B
An ultrasound-guided trucut needle biopsy was performed and pathology reported infiltration of the mammary stroma by monotonous and diffuse small lymphoid cell population with no angioinvasion. The axillary lymph nodes’ biopsy reported tumoral involvement. Immunohistochemistry markers were run and showed tumor cells positive for CD45, CD20, CD10, BCL2, BCL6, and negative for CKAE1/AE3 and CD56. The rate of cellular proliferation expressed as a Ki-67 proliferative index (PI) is 8% (Fig. 2). The diagnosis was defined as bilateral breast and axillary lymph nodes involvement by follicular non- Hodgkin B cell lymphoma histological grade LF1 and stage IV in the Lugano classification. Second line treatment ensued with rituximab-bendamustin protocol, 4 cycles, resulting in significant tumor cytoreduction and currently in the consolidation phase with rituximab 375 mg/m2 every 12 weeks, without bone mar row infiltration or new masses in positron emission tomography scan, or clinical characteristics evidencing its transformation to diffuse large B cells lymphoma (DLBCL).

Fig. 2 A-B: H&E 10x-40x Mammary tissue infiltrated by small, monotonous and diffuse lymphoid population surrounded by desmoplastic stroma. C: 10x immunohistochemistry CD45 positive in tumor cells, D: 20x Cell proliferation rate measured with KI-67 8%, E: 20x immunohistochemistry CD20 positive in tumor cells, F: 20x immunohistochemistry CD10 positive in tumor cells, G: 20x immunohistochemistry BCL-2 marking in tumor cells, H: 20x immunohistochemistry CKAE1/AE3 evidences absence of reactivity in tumor cells
Written informed consent was obtained from the patient for the publication of this case report and its accompanying images.
Discussion
Follicular lymphoma (FL) is generally an indolent B cell lymphoproliferative condition of transformed follicular center B cells. Its clinical characteristics are diffuse lymphadenopathy, cytopenias, bone marrow infiltration, splenomegaly, and less commonly extranodal involve ment8. The extranodal localization may appear in any anatomical position sharing similar characteristics regard ing morphology, immunophenotype, and genetics with nodal lesions, however, this location is associated to an unfavorable outcome5.
The infiltration by FL in the breast may be primary or secondary, the latter being the most common clinical pre sentation, requiring for the diagnosis the previous confir mation of a generalized extra-mammary hematolymphoid neoplasia5, as noted in our patient, who presented with a retroperitoneal mass, lymph nodes and subsequently bilateral breast involvement. Besides the clinical course, the diagnostic images may also help differentiate between primary and secondary lesions, since more frequently multiple and bilateral tumor lesions are found2,4 in second ary breast lymphomas, seen in the diagnostic images of this case.
From a pathophysiological perspective, follicular lym phoma is characterized by clonal, diffuse proliferation of germinal center B lymphocytes, specifically centrocytes and centroblasts, 85% of which present the (14;18) (q32;q21) translocation resulting in the fusion gene IGH-BCL2, associated to the overexpression of the B-cell leukemia/lymphoma 2 (BCL2) which induces the apoptosis blockade9.
Based on clinical factors, the patient was categorized according to the size of the tumor with the Lugano clas sification, which considers the involvement of one or two lymphatic regions in the limited phase (stages I and II), it adds the letter E when an organ outside the lymphatic system is affected, while the advanced phase (Stages III and IV) involves lymphatic regions on both sides of the diaphragm, and is diffuse in extra lymphatic organs. The patient was initially staged IIE due to the presence of the retroperitoneal mass and the involvement of lateral right retroperitoneal and inguinal lymph nodes, and subsequently in the tumor progression phase she was defined as stage IV, given the bilateral infiltration of the breasts9.
To consider the patient’s prognosis as low risk at the time of the diagnosis, a combination of clinical variables was used, which together belong to the Follicular Lym phoma International Prognostic Index (FLIPI), in order to estimate the overall survival (OS) and subsequently, with FLIPI-2 establish disease-free survival, after introducing the therapy with anti CD20 monoclonal antibodies8-10. The criteria used for the assessment were: older than 60 years of age, hemoglobin levels in peripheral blood lower than 12 g/dl, identification of Ann Arbor stage III and IV (cur rently modified in the Lugano System), high serum LDH values, and the number of nodes involved higher than 4. With these criteria the categorization is as low risk (score 0-1), intermediate (score 2) and high risk (≥ 3), estimating 91%, 78% and 53% OS at 5 years, respectively for each of the categories8-10.
The histologic characteristics of the tumor cells were analyzed to establish the morphologic classification as LF1, considering the number of centroblasts per high-power field: LF1 less than 6 centroblasts; LF2 from 5 to 15 centroblasts; LF3A more than 15 centroblasts and LF3B exclusive representation of centroblasts. This histologic grading system is relevant from the prognostic perspective since the scientific literature has shown that grade LF3B presents an aggressive clinical course with a higher risk of becoming DLBCL, while survival in grades LF1-3A exceeds 12 years11.
Staging with the above-described parameters led to the selection of the right treatment algorithm according to the National Comprehensive Cancer Network (NCCN) guidelines proposed for FL. Thus, for stages I or II and histologic grade LF1-3A9-12 the recommendation includes radiotherapy in the affected site (ISRT) with curative in tent. However, in the presence of large intra-abdominal and mesenteric lesions, first-line therapy with anti CD20 monoclonal antibodies is indicated (obinutuzumab or rituximab) plus CHOP chemotherapy12, leading to disease-free survival rates reported in the literature at three years of 68%12. Given the partial response to treatment and disease progression to Stage IV and the identification of large bilateral breast tumors, the treatment indications were assessed and following the NCCN guidelines, the second-line treatment was initiated with the rituximab + bendamustine scheme and consolidation with 375 mg/ m2 rituximab doses every 12 weeks12, with satisfactory response so far.
In conclusion, this case is an exceptional presentation of follicular lymphoma due to its bilateral breast extranodal location, where understanding the biological behavior of the pathology, through the analysis of clinical, histologic and prognostic factors, allowed for the final staging. This was relevant for individualized therapy selection accord ing to the clinical practice guidelines based on scientific evidence, with a positive impact on the medical progress of the patient.














