KEY POINTS
• In 2021, an online survey was answered by 1425 people with diabetes and their close contacts, mainly residents in different areas of Argentina and from all age groups.
• The annual vaccination rate of people with diabetes was 72% and was maintained even during the COVID-19 pandemic.
• The confidence level found in vaccines in general and in the influenza vaccine, in particular, was very high, and there is awareness about the risk posed by influenza for people with diabetes.
• Most surveyees said they had not found impediments that discouraged vaccination, but the difficulty among those who did lay in vaccines’ unavailability.
• Finally, it is necessary to highlight the need for more information regarding the topic in the media.
People with diabetes mellitus are more sus ceptible to numerous infections1-5, and respira tory pathogens are among the leading causes of severe conditions3,4,6. In the presence of diabe tes, influenza triples the risk of hospitalization, quadruples the probability of requiring inten sive care3,5, and increases the incidence of car diovascular events3,4,7.
Timely and appropriate immunization is the most cost-effective form of primary prevention of infections and their complications6,8-11. With the currently available vaccines, people with diabetes develop an adequate immune response3,8,9,12 and adverse effects are usually mild8.
As for the flu vaccine, the benefits are con sistent and have been demonstrated in exten sive studies and meta-analyses. Overall, the seasonal flu vaccine presents 58% effectiveness in reducing hospitalization and its efficacy for preventing death from any cause ranges from 38% to 56%1,3. It has been documented that the influenza vaccine is associated with a lower in cidence of respiratory failure in people over 75 years and pneumonia at any age1,10,12. The data also reveals that the vaccine is responsible for significantly decreasing mortality caused by car diovascular events in people with diabetes1,3,7,12. The efficacy of the pneumococcal vaccine varies from 56% to 84% (with the 23-valent polysaccha ride vaccine) to prevent pneumonia and reduce the use of health care services, even in patients aged over 75 years with diabetes8.
Based on the efficacy and safety of vaccines, annual vaccination against influenza, pneumo coccus, and hepatitis B is strongly recommended for all people with diabetes3,6,11,14-16. Diphtheria/ tetanus (DT) and zoster vaccines are also recom mended for adult patients17. In Argentina, all the immunizations mentioned, except for the last one, are included in the National Vaccination Calendar for free16,18.
In Latin America, 90% of countries have na tional policies/programs that include seasonal influenza vaccination. However, regional data on vaccination coverage are scarce, especially stratified according to risk levels19. It is essential to know the percentage of individuals who ef fectively access vaccination to implement com municable disease prevention strategies suc cessfully20.
Observational studies, such as surveys, al low data to be obtained and elaborated quickly and efficiently and provide valuable evidence to health policy-makers when evaluating vaccines’ effectiveness under real-world conditions14. Re search surveys on the population’s needs, opin ions and knowledge regarding issues related to their health are valuable to generate positive changes in people’s quality of life.
The Asociación para el Cuidado de la Diabetes en Argentina (Association for the Care of Diabe tes in Argentina - CUI.D.AR) is a non-profit or ganization whose goal is to improve the qual ity of life of people with chronic diseases such as diabetes. This paper synthesizes the results of a survey on people with diabetes and their close contacts. The survey has been specifically designed to gather the knowledge and the per ceptions participants have about the influenza virus, the disease and their associated poten tial risks. It also seeks to explore the confidence level in vaccines in general and in the influenza vaccine in particular.
Materials and methods
The survey “What is your opinion and level of confi dence in vaccination?” was allocated to people with dia betes mellitus and their close contacts, such as relatives, caregivers or other close contacts (people who are not blood relatives or active caregivers of the individual with diabetes, but are part of their environment and actively participate in daily decisions) mainly residing in Argen tina (96%), while also including a small share of non-res idents in the country (4%). The structured questionnaire presented 21 closed questions following a logical order so that the same topic questions were presented correla tively. Questions included multiple choice and close-end ed questions (yes/no and rating scale/drop-down).
The questionnaire was available through an online form to a non-probabilistic population sample between September 30 and November 15, 2021. The dissemination was carried out through CUI.D.AR social networks (Face book, Instagram, and Twitter) and mailing campaign sent to the CUI.D.AR database.
Participants answered the questionnaire anonymous ly, and their profile was strictly descriptive. Gender, age, place of residence and type of diabetes (if applicable) was the only information required to analyze it in a seg mented way based on these variables. The findings are presented in percentages to facilitate interpretation.
A response time of approximately 3 minutes was calculated because a more extended duration increases the dropout rate. A neutral Spanish language was used to maintain impartiality and avoid bias influencing the choice of one option over the rest. The questions were de signed to gather information on:
• The participants’ profile
• Knowledge about the influenza virus and flu and their potential risks and complications for people with diabetes
• The intervention of health professionals in vaccina tion strategies
• The participants’ confidence levels and opinions about vaccines in general and influenza vaccine in par ticular
• Compliance with immunization plans and their pe riodicity
• Potential impediments, problems or setbacks that discourage the application of the influenza vaccine
• The participants’ preference regarding the means they choose to be informed
Results
In total, 1425 participants completed the sur vey. Of the 822 people with diabetes (57.7% of the sample), 58.0% and 38.3% had type 1 and type 2 diabetes, respectively, and 3.7% had latent auto immune diabetes in adults (LADA) or gestational diabetes. The remaining 603 participants (42.3% of the sample) were family members, caregivers or close contacts of an individual with diabetes. Overall, there was evidence of a higher relation percentage (69.8%) with type 1 diabetes, either because they were people with the disease or people who were close contacts.
Regarding the age of people with diabetes, the most represented range were children under 18 (29.5%), and the least represented were people over 80 (1.3%). The rest of the age ranges, divid ed by decades, were equally represented. Of the people with diabetes, 59.6% were female, 40.0% male and 0.4% stated a different gender or pre ferred not to disclose it.
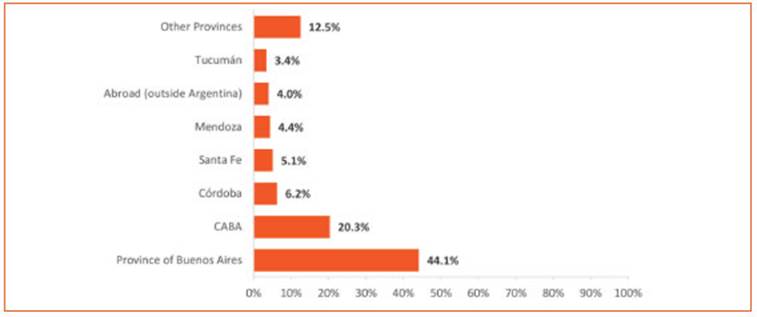
As for the geographical distribution of the participants, all the provinces were represent ed, including the Autonomous City of Buenos Aires (CABA) and a percentage of residents outside the country (4%). The province of Buenos Aires contributed the largest number of partici pants (Fig. 1).
Concerning the health system providing health care services, 51.2% of people with dia betes received assistance through health in surance institutions, including ~4% covered by the Comprehensive Medical Attention Program (PAMI by its Spanish acronym, a public health insurance organism managed by the Argentin ian Ministry of Health), 33.9% through prepaid medicine companies, and 14.9% received care in the public sector.
Regarding knowledge and perceptions of the influenza virus and the risks associated with infection, 81% of people with diabetes (666 par ticipants) and 91% of their family members, caregivers and close contacts (546 participants) considered that they pose a health risk to those with diabetes. Accordingly, 86.2% of participants (1228 individuals) stated that the flu could affect diabetes control.
About half of the participants (54.1%) respond ed that they did not remember or had never re ceived particulars from their physicians about the flu’s risks to people with diabetes. People with type 2 diabetes showed a more significant lack of knowledge: 3 out of 4 had not received or did not remember receiving information about the flu’s risks. Participants who reported receiv ing the most information were those with type 1 diabetes younger than 18 years or with type 2 diabetes between 50 and 59 years.
More than 96% of participants (1371 individu als) considered it important to extremely im portant for physicians to take an active role in vaccine prescription, and 9 out of 10 people with diabetes (88.2%) responded that the doctor had instructed them to get the flu vaccine at least once.
Regarding the confidence levels of the partici pants in the vaccines in general and in the influ enza vaccine in particular, the results were very similar: 9 out of 10 people expressed sufficient, much, or absolute confidence, and less than 10% reported having little or no confidence. On av erage, 64% of the participants (912 individuals) conveyed answers in a range between a lot and absolute confidence.
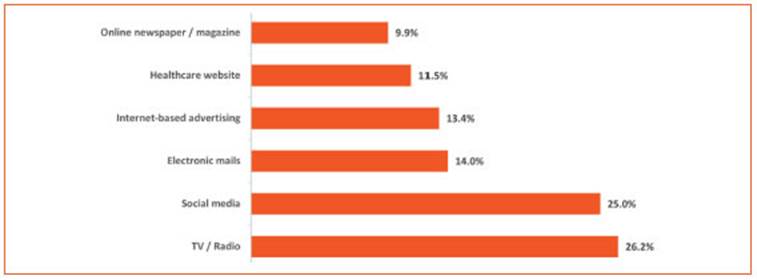
A 88% of respondents (1254 participants) stat ed that the person with diabetes had gotten the flu shot annually. The reasons for the decision to get it or not -which exclude each other mutu ally- are broken down in Figure 2.
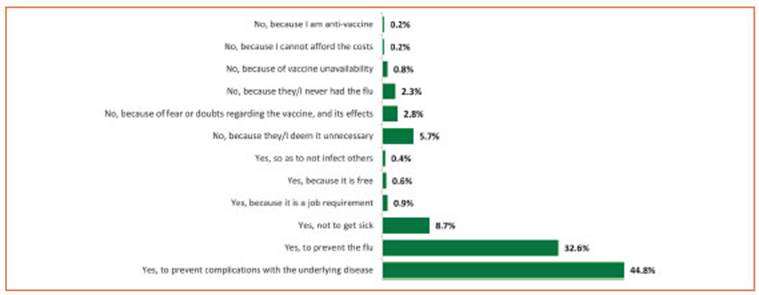
Figure 2 Influenza vaccination or lack of it and reasons for that decision (out of a total of 1425 participants)
Of the people who answered ‘yes’, half argued that they had chosen vaccination to avoid com plications of the underlying disease; others had done so to prevent the flu, and others, yet to a lesser extent, provided other reasons. The peo ple who chose not to get the flu vaccine mainly claimed that they considered it unnecessary, feared or doubted the vaccine and its effects, or gave other reasons for their decision. In some cases, the lack of vaccination was due to prob lems with vaccine availability or struggles in af fording it.
The COVID-19 pandemic made no significant change in the proportion of people with diabetes who received annual flu vaccination on a regu lar basis (72.0% in pandemic vs 73.5% pre-pan demic). However, there was a perceived impact on the group who had previously received the vaccine intermittently, as the number of people with diabetes in this group decreased from 8.6% pre-pandemic (123 individuals) to 2.3% during the pandemic (33 individuals). This decline ap pears to have contributed to the higher percent age of those who did not receive the vaccine during the COVID-19 pandemic. (Fig. 3).
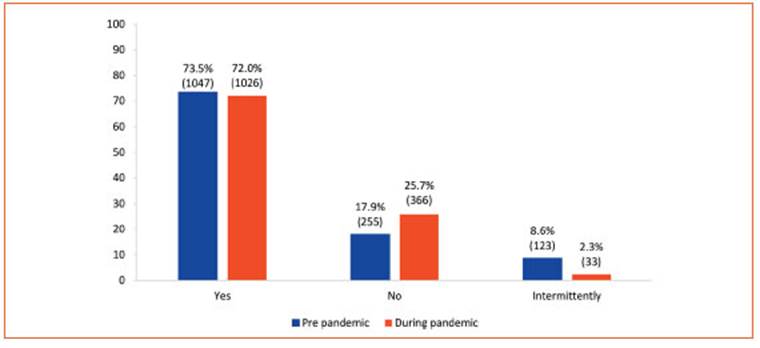
Figure 3 Percentage of consistent annual flu vaccination among people with diabetes before and during the COVID-19 pandemic (out of a total of 1425 participants)
Indicating coherence among the answers to related questions, 71% of the participants an swered that the person with diabetes had been vaccinated in the last year, a percentage consis tent with that of those who stated that they con tinued to receive the annual influenza vaccina tion during the pandemic (72%).
We asked if, at any time, any inconvenience discouraged or prevented people with diabetes from getting the influenza vaccine. Eighty-four per cent of participants reported that they never had any problems in this sense. Those who re ported having had some inconvenience men tioned the most frequent problem was the lack of vaccine availability (5.9%), followed by lack of trust in it (4.0%), previous bad experiences (3.2%), and logistics issues (scarce doctor’s appoint ments, error in prescriptions, excessive distance to vaccination centers), or monetary reasons.
For 75% of the participants, it was important for the person cohabiting with an individual with diabetes to get the flu vaccine. Of the par ticipants, 74.3% were aware that the flu vaccine was included in the National Vaccination Calen dar for free for people with diabetes, and 93.5% of participants considered that there should be more information in the media about vaccines. As for the preferred means of communication to receive information about influenza, its risks and prevention, answers varied, although televi sion, radio and social network options prevailed (Figure 4). Social networks were the means of communication chosen in the first place by peo ple between ages 18 to 50.
Discussion
The population that answered the survey in cluded people with diabetes and close contacts, mainly residents in different geographical areas of the country, of different ages and with varied health care coverage.
As a positive result, most survey respondents knew that the influenza virus poses a health risk to people with diabetes. Besides, 88% of them had been advised once to apply the influenza vaccine. Furthermore, 96% considered it essen tial that the physician’s role in vaccine prescrip tion was active. However, a high percentage of surveyees, especially those with type 2 diabetes and their close contacts, did not remember or had not received from their doctor information about the potential risks the influenza virus can pose for diabetes.
In the present survey, many participants ex pressed confidence in vaccines, and only a few people expressed distrust or previous bad expe riences. Concerning potential impediments to immunization, most participants reported no problems which might have discouraged being vaccinated against influenza. Whenever that was the case, the most frequent problem re ported was vaccine availability, which has also been documented in other countries in Latin America21.
The 72% annual influenza vaccination of people with diabetes reported by surveyees re mained unchanged during the COVID-19 pan demic. In addition, these data indicate that influenza vaccination coverage has improved in the population with diabetes in the country compared to previously published data.
Specifically, in 2013, the Encuesta Nacional de Factores de Riesgo (National Risk Factors Survey) conducted by the Argentinian Ministry of Health included for the first time a module designed to know the use of four of the recommended vac cines for adults (influenza, pneumococcus, hepa titis B and tetanus)20. According to the data collect ed then, 54.2% of the influenza vaccine use was for people between 18 and 64 with diabetes. Only 19.3% of individuals with diabetes reported receiv ing the pneumococcal vaccine, although the actu al figure might be underestimated because some people received this vaccine outside the period considered in the survey (2008-2013)20. Other local data available was from a survey on the diabetic population of Villa María, Córdoba, carried out in 2008-2009. In this study, only 41% of the sample population aged >45 reported receiving the influ enza vaccine within the last 12 months22.
Globally, annual influenza immunization rates are far from the 75% proposed by WHO, despite solid recommendations and growing evidence of benefits21. Reported coverage figures show considerable heterogeneity by country, covered period, age and risk level of people included in the studies. In the US, reported rates range from 50% to 62%; in Poland, they have been as low as 10%. On the other hand, they are close to 60% in the UK3,11, and Northern Ireland alone reached the recommended 75% target3.
The coverage rate is even lower in Asian countries6. In Thailand, retrospectively ana lyzed data from outpatients with diabetes - who had received health care services between 2010 and 2018- indicated influenza and pneu mococcal vaccination rates of 39.6% and 17.4%, respectively, and only 13.7% received both vac cines6. In Korea, the data analyzed for 2016- 2018, founded on an annual survey (KNHANES), showed a 60% coverage of the influenza vaccine for people with diabetes11. Another retrospec tive analysis, based on data from the same sur vey compiled between 2014 and 2017, reported that the flu vaccination rate was only 36.5% among diabetes patients under 6510. In 2022 in Saudi Arabia, a self-administered question naire given to a sample of adult patients with diabetes who had been assisted in a specialized center revealed that the prevalence of influenza vaccination was 43.5%15.
According to the published literature, the rea sons for rejection and impediments to vaccina tion are remarkably diverse3,12,13,15,23. It is neces sary to develop specific strategies for the context, the population and the vaccine to achieve high vaccination rates at population levels24. The underlying factors to support broad vaccine coverage are the dissemination of awareness and vaccine availability. However, an optimal doctor-patient interaction must also be added as a rel evant factor15,24.
Twenty-five per cent of the participants in this survey were unaware that the flu vaccine is accessible and free for all individuals with dia betes in Argentina. In fact, the flu vaccine has been present in the National Vaccination Calen dar since 2011, including people aged ≥ 65 and from 2 to 64 with risk factors, including diabetes. Also, the pneumococcal vaccine has been rec ommended since 2001 for people ≥ 65 years and ≤ 64 years with risk factors, including diabetes20.
More than 93% of surveyees felt there was a need for more information about vaccines in the media. The media relevance was also revealed in the 2013 Risk Factors National Survey, in which 71% of participants claimed to have received information about adult vaccines through tele vision, radio, the Internet or posters in public places20. The increasing digitalization of society and the use of innovative technological resourc es can be another means to increase vaccination rates, promote a positive attitude towards vac cines and collect information as a way of feed back for the health system6,24.
There are different strategies for assessing the use of vaccines, surveys being one of them. Surveys are commonly used in different parts of the world and allow us to know the temporal evolution of vaccine coverage, detect problems or obstacles to vaccination, and develop strate gies to overcome them20. However, this tool pres ents a disadvantage: vaccination coverage might be overestimated, and the data may pose inter pretation challenges20. One of the limitations of this survey is that, due to its non-probabilistic nature, the information presented cannot be generalized to the entire population with diabe tes in Argentina.
Finally, as in the present survey, the online format has advantages and limitations. The advantages include lower costs, time savings, simplified logistics and ease of use, while the disadvantages may include the challenge of comprising an adequate sampling framework and the exclusion of non-digitized parts of the population25.
Vaccination rates result from the complex in terrelationship between sociodemographic and behavioral factors, such as the perception of vaccines’ efficacy and safety. Data obtained in a real-life context, such as those presented in this paper, can help to comprehend the experiences, opinions and behavior of people with diabetes and their close contacts. Monitoring indicators through this kind of survey allows the genera tion of real-life evidence essential to optimize immunization programs for at-risk groups, thus improving people’s outcomes and quality of life26,27. In addition, the potential hospitalization reduction can be cost-effective28-30 and contrib ute to the health system’s sustainability.