INTRODUCTION
Lipoid pneumonia is a rare disease that results from the aspiration of mineral, animal or vegeta ble oils into the lungs. Once the oil is inhaled, it is phagocytized by the macrophages that fill the alveoli and loosen the alveolar walls, causing acute, chronic pneumonitis. Over time, the macrophages carry the oils from the alveoli to the interlobular septa, resulting in localized granulomas and pul monary fibrosis2. Predisposing factors include neu romuscular disorders and esophageal anomalies2.
We present the case of a male patient diagnosed with lipoid pneumonia. This case is of great in terest because the patient didn’t have swallowing disorders and showed an atypical-particular radio logical image, a spiculated lung mass with ground glass infiltrates and bilateral interlobular septal lines.
CASE REPORT
64-year-old male patient, university teacher, with history of insulin-dependent type I diabetes and chronic consti pation, and without history of smoking. The patient was admitted to our institution with fever associated with asthenia, myalgia and arthralgia of 10 days of evolution. Subsequently, he had generalized cephalea and chronic cough. Given the current epidemiological context, the patient was tested for COVID-19 on two occasions, with negative results. Physical examination: BP 140/80; HR 85 lpm, BR 28 rpm, SatO2 94% aa, temperature 37.5 °C. He showed good ventilatory mechanics, and the auscultation identified fine crepitant rales in the left pulmonary base. Lab tests, cultures and specific serology were requested: hemoglobin, 8.9 mg-dl, PCR 27.8, negative hemocultures, negative urine cultures, negative sputum, negative galac tomannan. A chest radiography was performed initially, showing a left basal consolidation; so, the patient began antibiotic treatment with azithromycin-ceftriaxone for 5 days, and then the regimen was modified and the patient continued with piperacillin-tazobactam because he had persistent fever. Due to persistent fever and lack of clinical response to treatment, a high-resolution chest tomography was performed, and it showed a spiculated, heterogenous lung mass with fibro-retractable bands and intralesional foci with negative density (fat density), located in the an terior and lateral segment of the left lower lobe. The mass was associated with patchy areas with increased interstitial-alveolar density, in ground glass opacity with geographic borders, with mild interlobular septal thickening (crazy paving pattern), in middle lobe, lingula and left lower lobe, with fine cylindrical bronchiectasis in the lingula. Absence of adenopathies and pleural effusion (Figure 1).
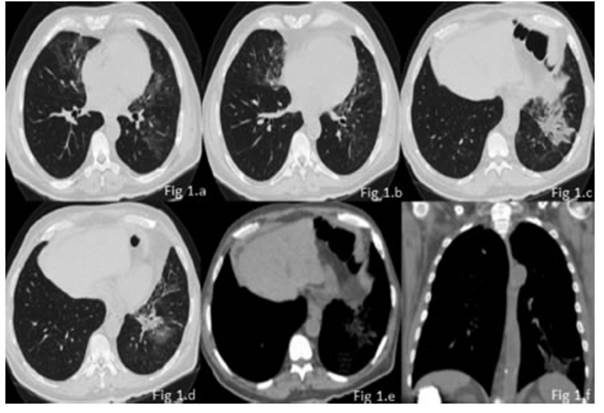
Figure 1 a and b High-resolution chest tomography: increase of interstitial density with patchy areas in ground glass opacity with geographic borders, associated with mild interlobular septal thickening (crazy paving pattern), with fine cylindrical bronchiectasis. c; d; e; f. Lung and medias tinal window showing a consolidation that simulates a “mass” of irregular borders, lipid range at tenuation, with bronchography and angiography in the anterior and lateral segment of right lower lobe. Findings suggestive of non-fibrosing exogenous lipoid pneumonia.
Due to radiological findings, a bronchoscopy with bronchoalveolar lavage (BAL) was performed: no germ development, negative BAAR (acid-alcohol-resistant baci llus), no yeast-like elements detected. From the clinical and radiological point of view, we were considering a differential diagnosis between lipoid pneumonia and lung neoplasm, so we decided to perform a biopsy for histopathological confirmation. First, a transbronchial biopsy was taken, in which we could observe small fragments of pulmonary parenchyma with moderate mononuclear, focal and diffuse inflammatory infiltrate. Also, groups of lipophages were recognized. Since the diagnosis wasn’t clear, a transtho racic puncture was carried out: its anatomopathological report showed lung tissue with alveolar spaces covered by pneumocytes without atypia, deposits of intraalveolar and interstitial lipophages, and interstitial adipocytes. Epithelial malignancy was discarded, and it was reported that morphological findings suggest the diagnosis of lipoid pneumonia.
DISCUSSION
The radiological presentation of our case is of great relevance, since it showed a lesion with heteroge neous density, with an evident lipid component in the mediastinal window (lipid range), simulating a mass of irregular borders which, together with the consumption of liquid vaseline, suggested the diagnosis of exogenous lipoid pneumonia without the fibrosing component.
It was produced as a consequence of the aspira tion of oils of vegetable, animal or mineral origin, and it can present itself in an acute form, due to the accidental aspiration of a large volume in a short time, or in a chronic form, with recurring intake of the compound through the airways for a long period. The degree of inflammation and lung fibrosis is related to oil aspiration: it depends on the amount of free fatty acids present. In gene ral, animal fat produces more inflammation and fibrosis than vegetable or mineral fat, because it is hydrolyzed by pulmonary lipases and releases free fatty acids3.
Regarding the clinical presentation, it may be asymptomatic and show casual radiographic alte rations or, there may be non-specific symptoms such as chronic cough, sometimes productive cough, dyspnea or intermittent fever3,5. Other less common symptoms are: chest pain, hemoptysis, and weight loss.
The radiographic aspect is non-specific, and can be described as consolidations or interstitial opacities, or as a noteworthy mass suspicious for pulmonary neoplasm5.
Tomographic findings in exogenous lipoid pneu monia include a sequence of radiological events, with initial predominance of ground glass opacities with centrilobular distribution, with low attenua tion value (-25 and -75 Hounsfield units). After one week, the density of the aspirated segment increa ses until it forms a clear consolidation, increasing the value of the segment’s HUs.
After two weeks, the density is reduced and returns mainly to ground glass opacities; during this period, the crazy paving pattern appears (due to the migration of macrophages and inflammatory cells to the interstitial lymphatic vessels). These opacities can be completely resolved, leaving resi dual thickening of the interlobular septa. If that doesn’t happen, as opacities increase, fibrosis will appear with up to approximately 50% volume loss of the affected segment, with vascular clustering, traction bronchiectasis and fissure displacement5.
Within the forms of radiologic presentation, we found that consolidation is the most frequent finding in 90% of the cases, with fat attenuation in 80%.
Then comes the form of irregular mass in 66% of the cases.
Ground glass opacities were found in 50% of isolated patients or associated with previously described findings, just like the crazy paving pat tern in 33%.
In cases of acute aspiration, we don’t see any sign of volume loss, which does occur in the chronic forms of the disease, in 80% of the patiens5.
Distribution is dependent on severity: the poste rior segments of upper lobes and apical segments of lower lobes being the most affected, in supine position, and basal segments in standing position5.
Regarding the resolution, acute aspiration usually improves in up to 80% of the patients, but very rarely disappears completely. But chronic aspiration normally remains stable over time5.
Diagnosing lipoid pneumonia is usually difficult because it is not routinely suspected when it first appears. Often, the cases are treated as commu nity-acquired pneumonia, and an alternative diagnosis is considered only if the patient doesn’t respond to treatment, as in our case. So, a detailed medical record has to be written, emphasizing pre vious exposure to fatty substances. Once the ELP is suspected, it is necessary to detect intraalveolar lipids and lipid-laden macrophages in respiratory samples. The samples may be taken from sputum, BAL, transthoracic puncture-aspiration cytology or surgical lung biopsy. With regard to the sputum, it is available but many patients can’t produce it, and so it may be difficult to obtain a representa tive sample. It also has questionable reliability, and lipid-laden macrophages have been found in the sputum in the absence of lipoid pneumonia6. The BAL is widely available nowadays, and its usefulness has been proven. It may show a turbid or off-white liquid with visible drops of fat on the surface. Transthoracic puncture is also a minima lly invasive procedure of diagnostic usefulness, though false negatives can be obtained due to the size of the sample. Thus, in some cases, a transbronchial lung biopsy or even a surgical biopsy may be necessary. Most reports have used lipid-laden macrophages as diagnostic markers of lipoid pneumonia; however, some authors have questioned their specificity6. So, the diagnosis of exogenous lipoid pneumonia must be based on the conjunction of the patient’s history of mineral oil intake, compatible radiologic findings, and the presence of intraalveolar lipids or macrophages with lipid content6.
Some possible complications are: over infection by atypical mycobacteria, which should be suspec ted in the presence of cavitary nodules, and also the occasional appearance of epidermoid carcinoma in chronic aspiration3,5.
With regard to treatment, there aren’t any studies that define the best therapeutic option, though the first measure that should be taken is to identify and suspend the use of the causative agent, which should generally be enough, mostly if the patient is asymptomatic4. Some reports suggest the use of corticosteroids to reduce inflammation. This treatment is reserved for acute cases with severe lung damage. Another option is the use of whole-lung lavage as it is used in alveolar protei nosis. Surgical treatment is reserved for patients that don’t respond to these last options and for esophageal alterations1,5.














