Insulin resistance is defined by a requirement greater thInsulin resistance is defined by a requirement greater than 200 IU/day of insulin1. Subcutaneous insulin resis tance syndrome (SIRS) is characterized by severe resis tance to subcutaneous administration (SC) of insulin with normal sensitivity when administered intravenously (IV)2,3.
In 1975, Schneider and Bennet described the first case of subcutaneous insulin resistance with a normal IV response in a patient with type 1 diabetes2.
Its pathogenesis has not yet been elucidated, although an increase in the enzymatic degradation of insulin in the subcutaneous tissue or inactivation by antibodies have been proposed as most probable causes4,5.
We present the case of an 18-year-old adolescent with type 1 diabetes, who was diagnosed with subcutaneous insulin resistance syndrome, and she received pancreatic transplant as definitive treatment.
Clinical case
An 18-year-old woman reported a history of type 1 diabetes since the age of 12 years. Family history was negative for diabetes and autoimmune diseases. She was treated with different kinds of subcutaneous insulin regimens and more recently with continuous subcutaneous insulin infusion (CSII). Despite her compliance, imbalance progressively worsened with permanent life-threatening ketosis during the last 3 years. It became obvious that ketosis could only be reduced via in travenous insulin therapy since subcutaneous injections were totally ineffective. The patient was hospitalized in another institution for months on account of numerous ketoacidosis episodes, where this problem was interpreted as an immune insulin resistance. She was treated with oral steroids and admitted to our institution. Physical examination on admission revealed a healthy state with a body mass index (BMI): 25.6 kg/m2. There was no sign of macrovascular and microvascular complications. Other examination findings were unremarkable.
Laboratory evaluations were: hemoglobin 13 g/dl, white blood cells 8.7 × 109/l and platelet count 220 × 109/l, serum AST 11U/l, ALT: 9 U/l, total bilirubin 0.9 mg/dl, LDH 335 mg/ dl, HbA1c 8.8%, total serum protein 7.2 g/dl, albumin: 4 g/dl, gamma globulin 0.82 g/dl, beta subunit negative, TSH 4.76 μU/ ml, peroxidase antibody 209 UI/ml, serum cortisol 25 μg/dl and C peptide < 0.1ng/ml. Urinalysis was normal, acid base state pH 7.37, PCO2 37 mmHg, HCO3- 21 mmol/l.
Ketoacids, HIV, HbsAg, HCV, celiac antibodies, circulat ing insulin autoantibodies and blood and urine cultures were negative.
Ophthalmoscopy, thoracic X-ray, electrocardiography, ab dominal and gynecological ultrasound were normal.
Considering the diagnosis of subcutaneous insulin re sistance syndrome immune mediated, we performed a skin biopsy to determine A and G immunoglobulins and C3 comple ment, which were negative.
Insulin was infused endovenously resulting in glucose monitoring improvement and blood insulin level of 58.2 μU/ml.
After switching to subcutaneous insulin, blood glucose level increased and blood insulin level decreased to 9.2 μU/ml requiring high insulin doses up to 356 units per day.
In order to establish an insulin regimen that the patient could continue at home, we added heparin to insulin lispro (1:10 in volume) in CSII with an increased serum insulin level (21.4 μU/ml) and bit of improvement in blood glucose level.
She was transferred for pancreas transplant alone form cadaveric donors. At 10 months’ post transplantation, she maintained an Hb1C of 6.9% and a C peptide of 1.9 ng/ml (VN 0.5-3.5 ng/ml) with immunosuppressive medication with early corticosteroid withdrawal and mycophenolate mofetil, without requiring insulin therapy.
Discussion
Subcutaneous insulin resistance syndrome is a rare cause of unstable diabetes, characterized by poor glycemic control despite the use of high doses of SC insulin, and that improves, along with decreased insulin requirements, when insulin is administered by IV route. Paulsen et al. established the diagnosis of this syndrome based on three criteria: resistance to the hypoglycemic action of SC insulin with normal sensitivity by IV route, absence of elevated insulin levels after injecting high SC doses, and increased degradation of insulin in the subcutaneous tissue3,5,6.
Clinical findings associated with severe insulin resis tance are highly variable and depend on the cause of the severe insulin resistance. These manifestations may include diffuse acanthosis nigricans and skin tags, ovarian hyperandrogenism, including hirsutism, oligoamenorrhea, and infertility. Some patients may have abnormal pheno types, including lipodystrophy and / or pseudo acromegaly1.
This patient had none of the known causes of insulin resistance. She had non hormonal dysregulation, no increase in the circulating antibodies to insulin. Her sen sitivity to IV insulin was not in favor of a genetic cause. She had neither lipo-dystrophy, atrophy nor dyslipidemia. No evidence of surreptitious administration of insulin or infection condition could be found.
SIRS excludes insensitivity to insulin at other levels (anti insulin or anti insulin receptor antibodies, receptor or post receptor defects), as well as inadequate compliance with treatment6.
The patiente we present had type 1 diabetes with low C peptide level. She progressively developed insulin resis tance as demonstrated by repeated ketoacidotic episodes when insulin was given subcutaneously, but she remained sensitive to intravenous insulin.
As our case, most of these insulin resistance syndrome cases are described in young women with type 1 diabetes, poor metabolic control, and multiple ketosis despite the increase in SC insulin doses. In some cases, the onset of the condition coincides with infections. However, most of the times, the apparent cause is not found3,5,7,8.
SIRS may be caused by various etiologies: one of these is increased insulin inactivation or proteolysis degradation in the dermal tissue3. We did not find A and G immunoglobulins and C3 complement in skin biopsy. Therefore, we suspected severe subcutaneous insulin resistance related to impaired transport of injected insulin from subcutaneous tissue into the circulation.
Insulin degradation takes place primarily in the liver, but nearly all peripheral tissues contain insulin-degrading enzymes. Its etiology is unknown but excessive insulin degradation in subcutaneous tissue by unidentified proteases or antibodies, or decreased insulin binding to adipocytes has been described1,9.
The average total daily insulin dose requirement for patients with type 1 diabetes is around 0.3-0.6 UI/ kg/day, with the notable exception of adolescents who typically require 1-1.5 UI/kg/day. A practical approach is to consider that anyone with total daily insulin dose (TDID) <1 UI/kg/ day has normal insulin sensitivity. The average TDID for patients with type 2 diabetes is around 1-1.5 UI/kg/day, however it can be as high as 2 UI/kg/day. In the context of type 2 diabetes, severe insulin resistance cases were defined as those patients who require more than 200 U insulin per day, because above this dose, the response to additional insulin ad ministration is attenuated. However, given the obesity epidemic, and the fact that insulin dose is significantly dependent on body weight, it is not unusual today for these patients to require more than 200 U of insulin per day. Therefore, it is preferred to define severe insulin resistance when TDID is higher than 2U kg/ day1,4. Our results showed 1) a significant decrease in glycemia only when insulin was injected intravenously by comparison with subcutaneous injections whatever the dose; 2) higher insulinemia levels with intravenous than with subcutaneous admnistration.
The term extreme insulin resistance is used to de scribe those patients with extremely high insulin require ments, defined as TDID > 3UI/ kg / day. Most of them are not obese and have a body mass index of less than 30 kg/m1,2,10.
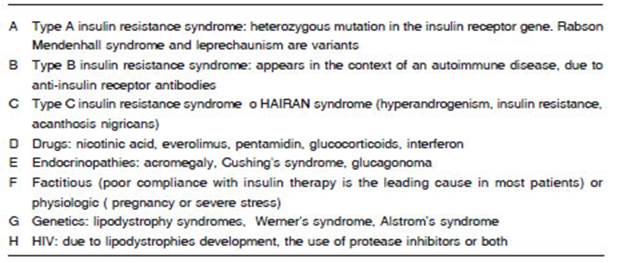
Rare disorders that lead to severe insulin resistance could be the underlying cause in some patients, such as insulin resistance syndrome type A, type B or type C, drugs (of non-habitual use) or endocrinopathies, among other causes (Table 1).
We used a subcutaneous insulin regimen with added heparin to insulin lispro, which increased serum insulin level, and decreased the blood glucose level. Some strategies of treatment have been tried: a) addition of aprotionin or heparin to insulin, due to the suspicion of insulin inactiva tion in subcutaneous tissue, with limited results5,8, b) lispro insulin analog has been reported to decrease the insulin resistance, probably because it can be rapidly absorbed and it escapes to the destruction process of subcutane ous insulin. For that reason, it has been reported that lispro analog insulin is effective in subjects with appar ent subcutaneous insulin resistance5,11, c) restoration of insulin secretion by pancreas transplant or beta cell transplantation12, d) administration of insulin by a route other than subcutaneous, initially continuous intravenous (with risk of thrombosis or infection of the catheter) and, more recently, through a connected in traperitoneal catheter with a programmable, external or implanted pump. Although the most accepted treatment is intraperitoneal insulin infusion, a possible temporary solution may be the use of a system that allows intraperi toneal infusion insulin, and6,13, immunosuppressive or immunomodulatory therapy, including glucocorticoids, cyclosporine A, cyclophosphamide, azathioprine, my cophenolate mofetil. Intravenous immunoglobulin and rituximab, have been reported favorable, especially in the treatment of severe insulin resistance syndrome type B. Plasmapheresis has been used successful in the treatment of severe type B insulin resistance syndrome, as well as in one case of severe insulin resistance due to anti-insulin antibodies (hypersensitivity), but has only temporary benefits4,9.
The case we present seems to correspond to a syn drome of resistance to subcutaneous insulin, demonstrat ed by the ineffectiveness of SC administration, as well as an improvement with IV insulin addministration. Previous treatments were ineffective or they only got temporary improvements. It seems to be caused not by the dermal inactivation of insulin but by the defects in the absorption processes of subcutaneous insulin.
Despite the fact that the effectiveness of heparin plus lispro insulin may lead us to further understanding of pathophysiology of this syndrome, our patient required to be transferred for pancreas transplantation.