Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Medicina (Buenos Aires)
versión impresa ISSN 0025-7680
Medicina (B. Aires) vol.75 no.5 Ciudad Autónoma de Buenos Aires oct. 2015
ORIGINAL ARTICLE
Epidemiology of angioedema without wheals in an allergy and immunology center
Eloisa Malbrán, Diego Fernández Romero, Maria Cecilia Juri, Blas J. Larrauri, Alejandro Malbrán
Unidad de Alergia, Asma e Inmunología Clínica, Buenos Aires, Argentina
Postal address: Eloísa Malbrán, Av. Roque Sáenz Peña 1160 1° B, 1035 Buenos Aires, Argentina
e-mail: elomalbran@hotmail.com
Received: 10-III-2015
Accepted: 12-VIII-2015
Abstract
We describe the diagnostic epidemiology, the clinical course, the family history and the response to treatment of patients with angioedema without wheals (AWW) at an Allergy and Immunology Clinical Center. We reviewed the case records of all patients at our office from January 1997 to April 2013. We recorded sex, age, age at onset of symptoms, family history of angioedema, number of visits to the office, type of angioedema, and response to treatment from those patients with angioedema without wheals. We classified angioedema according to its pathophysiology. We also describe those patients with angioedema mimics. From a total of 17 823 new patients, 303 had a presumptive diagnosis of angioedema without wheals. Twenty-three patients had an angioedema mimic. Forty percent were male and 60% were female. Average age at first visit was 40.6. Average number of visits was 2.4. Fifty-seven patients referred a family history. We attributed idiopathic angioedema to 55.7% of patients, 24.3% were drug related, 15.7% were due to C1 inhibitor deficiency, 2.1% were drug related + idiopathic angioedema, 1.4% were type III and 0.7% had exercise-induced angioedema. Ninety six percent of 53 evaluable idiopathic angioedema patients referred a benefit with anti-histamine therapy. AWW was a rare cause of consultation. Most of our patients had anti H1 responsive idiopathic angioedema and none had allergic angioedema. Women cases prevailed over men´s. Family history and average age of onset of symptoms were different among the different types of angioedema.
Key words: Angioedema; Epidemiology; Allergy.
Resumen
Epidemiología del angioedema sin urticaria en un consultorio de alergia e inmunología.
Describimos la epidemiología, historia clínica, antecedentes familiares y respuesta al tratamiento de los pacientes consultando por angioedema sin urticaria en nuestra clínica especializada en Alergia e Inmunología. Revisamos retrospectivamente todas las historias clínicas de nuestro consultorio entre enero de 1997 y abril de 2013. Seleccionamos aquellos pacientes que habían consultado por angioedema sin urticaria y registramos el sexo, edad, edad de comienzo de síntomas, antecedentes familiares de angioedema, número de consultas, tipo de angioedema y respuesta al tratamiento. Clasificamos el angioedema de acuerdo a su fisiopatología. Describimos también los diagnósticos diferenciales que encontramos. De un total de 17 823 pacientes, 303 consultaron por angioedema sin ronchas. Veintitrés presentaban un diagnóstico alternativo. El 40% eran hombres y el 60% mujeres. La edad promedio de la primera visita fue 40.6 años. El promedio de consultas fue 2.4. Cincuenta y siete refirieron antecedentes familiares. El 55.7% fue clasificado como angioedema idiopático, el 24.3% secundario a drogas, el 15.7% secundario a deficiencia del inhibidor C1, 2.1% por drogas + idiopático, 1.4% angioedema tipo III y 0.71% asociado al ejercicio. Noventa y seis por ciento de 53 pacientes evaluables con angioedema idiopático se beneficiaron con antihistamínicos. El angioedema sin urticaria fue una causa rara de consultas. Las mujeres prevalecieron sobre los hombres. Los antecedentes familiares y la edad de comienzo de síntomas variaron de acuerdo al tipo de angioedema.
Palabras clave: Angioedema; Epidemiología; Alergia.
Angioedema is a reversible localized swelling of the deep cutaneous layers caused by mediators that enhance vascular permeability1. It generally involves the skin, particularly in the face, but it can also involve the mucosa of the upper respiratory and/or digestive tracts, the extremities and genitals. It is a non-pitting, skin-colored edema, and it shows a predilection for areas where the skin is lax rather than taut, specially the face and genitalia2. Heat and pain are variable additional symptoms, itching is rare; there is no desquamation or staining of the skin although scratching or rubbing may cause bruising2. It is often associated with urticaria, but occasionally it occurs without urticaria as angioedema without wheals (AWW)3.
Several mediators are involved in the pathophysiology of AWW, including histamine, leukotrienes and bradykinin4-8, leading to the classification of angioedema according to its mediator9, 10. The differential diagnosis of angioedema is very important since its treatment and prognosis are very different6, 8, 10-13. On the one hand, angioedema produced through histamine is usually controlled with anti-H1 anti-histamines, it rarely compromises areas outside the face, and it is usually benign. On the other hand, bradykinin mediated angioedema, like hereditary angioedema, requires a whole different therapeutic approach and it has 15% to 50% asphyxia related mortality6, 12. The epidemiology of the different types of angioedema in a particular population has only been described once in a tertiary referral center, with a special interest in hereditary angioedema3, but, there is not much knowledge of how often and which type of AWW can be present at an Allergy and Immunology Community Clinic.
In this paper we describe the diagnostic epidemiology, clinical course, family history and response to treatment of patients consulting with angioedema without wheals at an Allergy and Immunology Clinic.
Materials and Methods
We conducted a retrospective study, reviewing all case records of patients at our office from January 1997 to April 2013. We differentiated those patients who, at their first visit, were diagnosed angioedema without wheals. In all occasions, patients were asked about the presence of urticaria during or before the appearance of angioedema and about any other episode of prolonged urticaria they might have experienced before. If that was the case, they were assumed as chronic urticaria patients and were excluded.
We recorded sex and age at first visit, age at onset of symptoms, family history for angioedema, the number of visits to the office, the type of angioedema presumed and the response to treatment.
We intended to classify angioedema as follows: drug-related angioedema cases were those patients that had a clear history of angioedema related either to ACE inhibitors, NSAIDS or any other drug described as producing AWW, and whose symptoms did not recur after discontinuation. C1 inhibitor related angioedema could be either hereditary HAE Type I (low C1 inhibitor in serum) and HAE Type II (functional alteration in C1 inhibitor) ± family history of angioedema, or acquired (secondary to autoimmune, lymphoproliferative or other diseases). Type III angioedema patients were those whose angioedema was clinically similar to HAE, who had a family history of angioedema and normal C4 and C1 inhibitor activity. IgE mediated or allergic angioedema was diagnosed in those cases that had a clear cause effect; patients presented the symptoms after having contact with the antigen, and their symptoms disappeared while avoiding the cause. Idiopathic angioedema was assigned to those patients who did not have a clear cause of IgE mediated angioedema, who did not receive drugs suspected to induce symptoms, and who did not have any hereditary type of angioedema. This group was sub classified as histamine resistant or not, according to the response to antihistamines. Exercise-induced angioedema were those patients who presented angioedema while exercising. A last group named drugs + idiopathic angioedema included those patients whose angioedema was initially classified as drug-related, but continued presenting occasional attacks after discontinuation of drug.
We evaluated the response to treatment of those patients with idiopathic angioedema who presented episodes more frequently than twice a month, who were prescribed with anti-H1 anti-histamines and who returned for follow up visits (twice or more times).
In a group of patients, an angioedema mimic was diagnosed. We also described the epidemiology of those patients.
All the data was collected and analyzed with Epi-Info 7.1.1.4, CDC.
Results
Out of the 17 823 new patients consulting our Office from January 1997 to April 2013, 303 patients had a presumed diagnosis of angioedema without wheals, with a prevalence of 1.7%. We received 27 209 patients consults during 2011, 2012 and 2013; 155 of such visits (0.6%) were AWW related.
Twenty three patients out of the 303 had an angioedema mimic. The remaining 280 patients were diagnosed AWW; 113 patients (40.4%) were male, and 167 (59.6%) were female. The average age at first visit was 40.6 ± 17.4 y/o (range 4-89, median 37) and the mean age of onset of symptoms was 35.5 ± 19.1 y/o (range 0-88, median 32). According to sex, mean age at first visit was 38.2 ± 17.1 y/o in females and 44.2 ± 17.4 y/o in males. Mean age of onset of symptoms was 32.9 ± 18.3 and 39.3 ± 18.5 respectively. Final diagnosis frequencies, age at onset of symptoms, age at diagnosis and presence of family history are depicted in Table 1.
Table 1. Epidemiology of angioedema

The mean number of visits was 2.4 ± 2.4 (range 1-27, median 2, mode 1). Fifty-seven patients out of 252 (22.6%) referred a family history of the AWW; 35 (61.4%) of those patients had C1 inhibitor deficiency related angioedema. No information was available in 30 patients.
Of the 68 patients that were classified as drug related angioedema, 42 (61.8%) were associated with non steroidal anti-inflammatory drugs (NSAID), 25 (36.8%) with ACE inhibitors (ACEI) and one (1.5%) was associated with other drugs. This distribution was similar for men and women (Table 2).
Table 2. Drug related angioedema prevalence

Idiopathic angioedema patients with symptoms twice or more times per month were treated with cetirizine 10 to 20 mg/day. Ninety-three of the 156 patients returned for follow up twice or more times; fifty-one (96%) out of fifty-three evaluable patients referred a benefit with such treatment, the others either did not take the medication or its efficacy was not recorded in the case record.
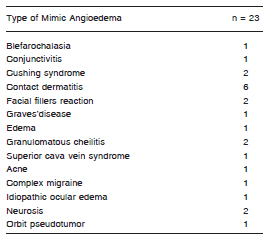
Twenty-three out of the 303 patients consulted for angioedema but had an angioedema mimic instead. Their final diagnosis is listed in Table 3. All of them were clinically characterized by swelling, lasting over several days or weeks, sometimes presenting erythema overlying the angioedema area. The most common mimic angioedema diagnosed was contact dermatitis. Those patients with Cushings syndrome had the feeling of fullness of their upper trunk and face without any objective angioedema as shown by patients with superior cava vein syndrome. Twenty-one patients were females and two were males. Mean age at first visit was 42.7 ± 15.2 y/o (range 18-7, median 41), and average age at onset of symptoms was 41.3 ± 15.5 y/o (range 13-71, median 37).
Table 3. Type of mimic angioedema
Discussion
Angioedema is a frequent companion of urticarial flares13. However, angioedema without wheals is a rare disorder and it represents only 1.7% of all first consults to our Allergy and Immunology Office. Moreover, AWW patients represented only 0.5% of total office visits during a random 3-year period. To our knowledge, this is the first study that assesses the frequency of AWW in an allergy practice. In this paper, we also describe the epidemiology and other characteristics of patients with angioedema.
In a detailed previous paper by Zingale et al3, working at a third level reference angioedema clinic, they described 776 patients recruited over10 years. Both in Zingale´s study and our own, women prevailed over men, the mean age at first visit was around 40 y/o and age of onset of disease in females was approximately 6 years earlier than in males. Both studies attempted to classify their patients on the basis of the presumed pathophysiology of the disease. However, there are some differences and similarities that reflect that ours is a primary care facility and Zingales is a specialized tertiary referral clinic. It is to be noted that most of our drug related angioedema were induced by NSAIDs and that we related none to allergies or infectious processes.
Even though most patients referred angioedema as an uncomfortable situation, average time from onset of symptoms to first visit was surprisingly long, mean 60 months. Delay time to diagnosis was longer in hereditary angioedema than in other causes of AWW, reflecting its very low incidence in the general population and lack of physician awareness on this disease.
A fifth of our patients referred a family history, including 80% of patients with hereditary angioedema and, by definition, 100% of patients with Type III angioedema. Some patients in the HAE group did not have a family history of angioedema and were assumed as first mutations. Noticeably, 10.3% of patients with drug related angioedema and 7.7% of patients with idiopathic angioedema had family history. The family history in these last two groups suggests some sort of predisposing defect still undisclosed.
As in the cohort described by Zingale et al, idiopathic angioedema was the principal type of angioedema found, but with a different distribution since 56 percent of our patients had idiopathic angioedema compared to 38 percent in theirs. The diagnosis of idiopathic recurrent angioedema was made after ruling out other causes of angioedema.
Patients were initially treated with antihistamines (cetirizine 10 to 20 mg/day) most of them presenting a benefit, suggesting that this reaction might be mediated by histamine, even though no specific cause is found. Anti H1 resistant cases received second line steroids. None of our patients received tranexamic acid as a prophylaxis.
The next most common cause of angioedema was drug-related, most often related to NSAID and to ACEI in second place, both in females and males. Patients referred onset of angioedema after receiving the causative drug; in many cases patients had received it for long time before symptoms appeared. It was easier relating angioedema to ACEI than to NSAIDS or other drugs since most patients did not consider NSAIDs as angioedema inducing drugs, and had difficulties recalling if they had or had not consumed this medication previous to the event. An exhaustive medical history is needed to make this diagnosis.
One of the patients in the drug-related group had symptoms affecting her arms, legs, face and abdominal pain while consuming oral contraceptives and disappeared while avoiding them, suggesting an estrogen relation, but she did not have a positive family history. It might have corresponded to a first mutation of Type III angioedema, but we were unable to sequence the factor XII gene.
In 6 of our patients, angioedema did not completely resolve after avoiding the drug, so we classified them as drug-related + idiopathic, considering that other mechanisms could also be present. All of these patients were males, and mean onset of symptoms was near 10 years later than those patients that responded to drug withdrawal.
We believe our HAE incidence is artificially high, since our office is associated to the British Hospital in Buenos Aires, where the Allergy and Immunology Department is a referral center for hereditary angioedema. Relatives of those patients and others consult our downtown office increasing the proportion of patients with HAE in our statistics. Most HAE patients referred long-standing and recurrent episodes of angioedema, abdominal pain episodes and a clear family history. All patients have a C4 and C1 inhibitor (quantitative and sometimes functional) measured, and in positive cases diagnosis was made. The true HAE consult incidence in a community practice is probably even lower than ours that is lower than the one found by Zingale.
We identified a few cases of Type III angioedema, all from different families. Three of them were females presenting with angioedema either during pregnancy or with the use of oral contraceptives containing estrogens, with onset of symptoms during young adulthood. The association of high estrogen situations, family history and normal C1 suggested this type of angioedema. There was one male patient, who presented with family history of angioedema, with normal C1 (quantity and functional); he was also classified as Type III, presenting with cutaneous angioedema, crisis of abdominal pain and laryngeal edema, unresponsive to anti H1 and to several icatibant injections, he partially improved on danazol 200 mg/day.
Two of our patients presented with angioedema exclusively while doing exercise. Both were women and had no family history of angioedema. Mean age of onset of symptoms was adolescence.
None of our patients had allergic or IgE mediated angioedema, suggesting that most allergic reactions combine urticarial flares or systemic symptoms.
In summary, in Allergy and Immunology, AWW is an uncommon diagnosis and cause of consultation. Most cases will be drug related or antihistamine responsive idiopathic angioedema, leaving a group of anti H1 resistant idiopathic angioedema patients along with HAE and type III hereditary angioedema. Those patients will need a dedicated care.
Conflict of interest: None to declare
1. Cicardi M, Bergamaschini L, Zingale LC, Gioffré D, Agostini A. Idiopathic non histaminergic angioedema. Am J Med 1999; 106: 650-4. [ Links ]
2. Kaplan AP, Greaves MW. Angioedema. J Am Acad Dermatol 2005; 53: 373-88. [ Links ]
3. Zingale L, Beltrami L, Zanichelli A, et al. Angioedema without urticaria: a large clinical Surrey. CMAJ 2006; 175: 1065-70. [ Links ]
4. Bernestein JA, Moellman J. Emerging concepts in the diagnosis and treatment of patients with undifferentiated angioedema. Int J Emerg Med 2012; 5: 39. [ Links ]
5. Cugno M, Nusseberger J, Cicardi M, Agostoni A. Bradykinin and the pathophysiology of angioedema. Int Immunopharmacol 2003; 3: 311-7. [ Links ]
6. Prematta MJ, Kemp JG, Gibbs JG, Mende C, Rhoads C, Craig TJ. Frequency, timing and type of prodromal symptoms associated with hereditary angioedema attacks. Allergy Asthma Proc 2009; 30: 506-11. [ Links ]
7. Malbrán A, Fernández Romero DS, Menéndez A. Hereditary Angioedema. A therapeutic guide. Medicina (B Aires) 2012; 72: 119-23. [ Links ]
8. Cicardi M, Aberer W, Banerji A, et al; HAWK under the patronage of EAACI. Classification, diagnosis and approach to treatment for angioedema: consensus report from the Hereditary Angioedema International Working Group. Allergy 2014; 69: 602-16. [ Links ]
9. Bork K, Fischer B, Dewald G. Recurrent episodes of skin angioedema and severe attacks of abdominal pain induced by oral contraceptives and hormone replacement therapy. Am J Med 2003; 114: 294-8. [ Links ]
10. Bork K, Wulff K, Witzke G, Stanger G, Lohse P, Hardt J. Antihistamine resistant angioedema in women with negative family history: estrogens and Factor XII gene mutations. Am J Med 2013; 126: 1142e9-1142e14. [ Links ]
11. Frigas E, Park M. Idiopathic recurrent angioedema. Immunol Allergy Clin North Am 2006; 26: 739-51. [ Links ]
12. Gunken A, Thurner K, Kanonier G, Sprinzl G, Thumfart W. Angioneurotic edema as a reaction to angiotensin-converting enzyme inhibitors. Am J Otolaryngol 1996; 17: 87-91. [ Links ]
13. Champion RH, Roberts SO, Carpenter RG, Roger JH. Urticaria and angio-oedema. A review of 554 patients. Br J Dermatol 1969; 81: 588-97. [ Links ]













