Desmoid type fibromatosis (DF) is a rare tumor characterized by monoclonal proliferation of fibroblasts in muscles, tendons, and ligaments. DF accounts for 3% of all soft-tissue tumors with an incidence of 0.2-0.4 cases/100 000 inhabitants/year1. According to the World Health Organization (WHO) 2013 classification of soft-tissue tumors, DF is considered an intermediate malignant, locally aggressive, and non-metastasizing tumor. Although DF is associated with a high recurrence rate (24-76%) the 10-year overall survival (OS) is higher than 90%2.
Two forms of presentation have been defined: the sporadic form, more frequently affecting young women, and the form associated with familial adenomatous polyposis (FAP) (7-16%)3.
Some studies suggest that DF derives from mesenchymal stromal cells4. A history of trauma is associated with DF5. Overall, 85% of the sporadic cases have a mutation in the CTNNB1 gene (the β-catenin gene)6. Some authors have suggested that the mutation spectrum is more complex in children than in adults, associated with AKT (31%), BRAF (19%), and p53 (9%) mutations, in addition to the CTNNB1 gene mutation7.
DF clinically presents as a firm, often asymptomatic, slow-growing mass, sometimes invading neighboring tissues and compromising vital structures.
Tumor location is divided into abdominal (6-8% of the cases) and extra-abdominal. Children seem to be more affected by head and neck-DF than adults. Head and neck are affected in 26-33% of children with DF, corresponding to the second most prevalent site in this population after primary trunk and limb tumors (versus 7-9% in the adult population)8. A multifocal presentation is less frequently observed9.
The disease course may be either indolent, in 5-10% of the cases, or aggressive, with a trend towards recurrence despite adequate surgical resection10. Among favorable prognostic factors, tumor size < 5 cm, head and neck location, and age younger than 10 years have been described11. Historically, margin-free surgical resection has been the treatment of choice. However, surgery may be difficult due to the infiltrative growth pattern of the tumor as well as contradictory results regarding microscopic margin status and recurrence-free survival12. currently it is recommended not to try to achieve margin-negative resection if this results in loss of function or significant morbidity13-17.
Radiotherapy is limited in children due to the increased risk of second neoplasm and a certain degree of radioresistance (5-year local control of 72% in ≤ 20 years compared to 97% in ≥ 40 years p = 0.009)18,19.
Over the last years, low dose chemotherapy (LDC) has been suggested as an alternative to extensive surgical resection20. Due to the slow-growing nature of the tumor with a slow response to chemotherapy, the treatment should be administered for a prolonged time. LDC consists of a combination of low weekly doses of methotrexate (MTX) together with vinca alkaloids21. Tamoxifen associated with sulindac or celecoxib is an additional treatment option with a 2-year progression free survival (PFS) rate of 36%22. A moderate response to hydroxyurea has been reported as well23.
Despite the heterogeneous behavior of DF, it is well known that the majority of the cases progress within the first two years, with a five-year PFS of 50% without treatment.
Based on these findings, the main international pediatric collaborative groups proposed a conservative (“watch-and-wait”) strategy21,24. The aim of this strategy is to evaluate disease behavior, avoiding treatment in patients that will have SD or even disease regression without treatment. If the tumor is located in a site that will compromise organ function, either leading to symptoms or showing rapid progressive growth, LDC should be recommended25. Primary surgery should only be considered if tumor-free margins can be achieved without sequelae26.
As previously mentioned, DF is a disease with an excellent survival, being the long-term sequelae, an important issue27.
The aim of this paper is to describe the clinical characteristics, response to treatment and outcome of a series of pediatric patients with DF treated in a single institution over 14 years, with special emphasis on the analysis of long-term sequelae.
Materials and methods
A retrospective descriptive study was conducted evaluating 18 tumors in 16 patients younger than 16 years with a histological diagnosis of DF treated at the Garrahan Hospital in Buenos Aires, Argentina, between January 2002 and December 2016. Garrahan Hospital is a third-level pediatric hospital, which treats approximately 40% of pediatric cancer in the country.
Initial tumor size as well as response to treatment was assessed using ultrasonography and/or computer tomography scan, and/or magnetic resonance imaging of the tumor site involved.
From 2005 onwards, patients have been treated according to the guidelines of the EpSSG non RMS 2005 protocol [vinblastine (VBL) 6 mg/m²/week, MTX 30 mg/m²/week], followed by 6 months of spacing the administration to every 2 weeks. Previously, there were no specific treatment guidelines.
Complete response (CR) was defined as complete disappearance of the tumor, PR as a tumor reduction between 33% and 99%, disease progression as any increase greater than 40%, and SD as cases that did not meet the criteria for either PR or DP. Tumor size was measured in 3 diameters, and tumor volume was determined.
The quality of resection in surgically treated patients was assessed according to the staging system of the Intergroup Rhabdomyosarcoma Study (IRS)28.
Adverse effects were graded according to the CTC criteria v.4.029.
We will refer to the number of tumors, in addition to the number of patients, given that in patients with more than one tumor, these tumors did not have the same evolution.
OS was defined as time from diagnosis to last follow up or death; PFS as the time from diagnosis to progressive disease (PD) or recurrence. Response rate to chemotherapy was defined as the percentage of patients who achieved PR or CR.OS and PFS curves were calculated with the Kaplan-Meier method using the statistical program IBM SPSS Statistics for Windows, Version 20.0.
Results
Sixteen patients with 18 desmoid tumors were included in the study. Median age at diagnosis was 11.5 years (range: 0.25-16) and male-to-female ratio was 1:1. The most commonly location was in the limbs (7) and trunk (6), followed by the head and neck (3) and abdomino-pelvic cavity (2) (Fig. 1). Two patients had multifocal tumor, one of whom was associated with FAP. Two patients had a history of surgical trauma, related to correction of congenital dislocation of the hip in one and colectomy in the other, the last related to FAP (Fig. 2). Two patients had a history of trauma, both due to a fall, in one with an associated fracture. Symptoms at diagnosis were tumor (9 patients), pain (5 patients), and decreased range of motion (3 patients). Median largest initial diameter was 9.9 cm (range 3.5-18). In 5 patients nerve involvement and in 3 compressions of adjacent structures was observed. Median time between symptom onset and biopsy was 358 days (range 28-2282 days). Clinical features of the patients are shown in Table 1.
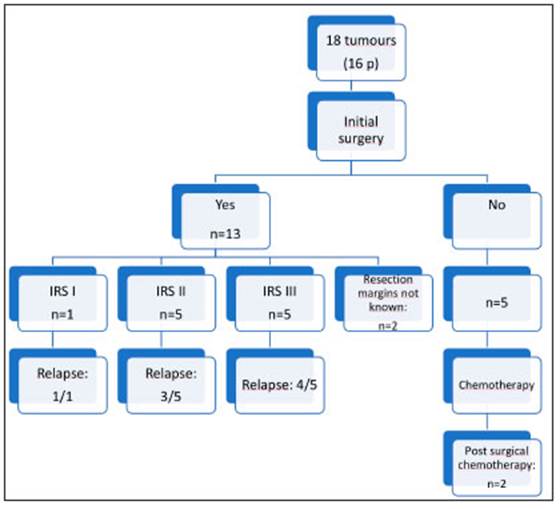
Initial surgery was performed in 13 of 18 tumors (12 patients) with a relapse rate of 76% (10/13), with a median time to relapse of 4.5 months (range 4-9). Four patients achieved CR following surgical treatment alone. Two of the 4 patients required 3 and 4 surgeries, respectively. Only 2 patients who underwent surgery are alive at the first CR at 12 and 38 months, both were extra-abdominal and with microscopic involvement of surgical resection margin (Fig. 3).
Eleven patients with 13 tumors underwent chemotherapy according to the EpSSG non RMS 2005 protocol. Two patients with 2 tumors each achieved CR in one tumor and PR in the other. In both patients, tumors achieved CR after initial surgery and received chemotherapy as surgical treatment consolidation and to treat the other tumor. The remaining 11 patients (one tumor each) achieved PR in 4 cases, SD in 3 cases and 2 patients presented PD. One of them achieved SD after 4 lines of treatment (MTX/VBL, cyclophosphamide/ vinorelbine, radiotherapy, and imatinib) and the other, who was lost to follow-up 3 months after diagnosis, returned to the hospital with PD and died because of intrathoracic compression of neighboring organs 35 months after the diagnosis. Overall, the response rate to upfront chemotherapy was 54% and up to 81% if SD cases were included (Fig. 4).
Median treatment duration was 11 months (range 1-36). Only 2 patients had significant tumor reduction (at least PR) 3 months after initiation of chemotherapy, while in the remaining patients the reduction occurred after 6 to 15 months. Median time of response to treatment was 8 months (range 1-15).
Two patients were found to have FAP; one of them had congenital multifocal tumor and the other developed a retroperitoneal tumor 12 months post-colectomy. The first patient kept SD for 6 years, until he showed PD, and surgery was performed. After surgery, the tumor showed fast growing and pain, so he underwent metronomic chemotherapy. The second case underwent surgery followed by radiotherapy and hormonal treatment.
No significant differences in PFS were found when comparing tumor size, location, and initial treatment (Fig. 5).

Fig. 5 Kaplan-Meier estimates presenting EFS of patients with desmoidtype fibromatosis according to (A) primary approach, (B) size and (C) location
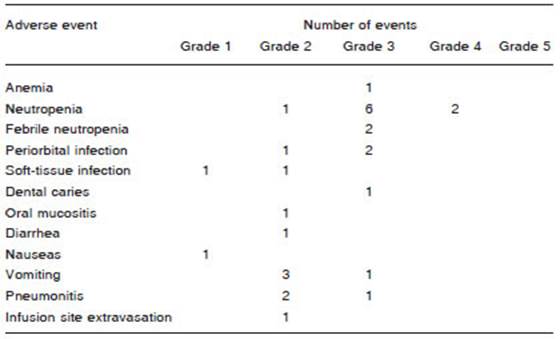
Only 2 patients had grade 4 toxicity, and neutropenia in both. Out of 41 courses of chemotherapy, febrile neutropenia was observed in two. Seven of 11 patients required a reduction of the VBL dose (of 6 mg/m2 to 4 mg/m2) because of treatment delay due to hematological toxicity (Table 2). After dose reduction there were no new suspensions of the treatment due to toxicity.
Two patients with PD received radiotherapy (dose: 50 -56 Gy) achieving PR in one case (receiving tamoxifen concomitantly with and after radiotherapy) and PD in the other. None of the patients had complications at 12 and 25 months after treatment completion.
Disease status at last evaluation was: one patient died and 15 patients with 17 tumors were alive. Considering tumor status of the last group, 7 tumors were in CR, 7 in PR, and 3 had SD.
Twelve of 15 patients (80%) had sequelae, which were cosmetic in 11, most frequently a keloid scar (5/11), and functional in 9, mainly consisting of decreased range of motion (5/9). In 8 cases sequelae were directly related to the surgical intervention and 3 of them were severe.
After a median follow-up of 40 months (range 12-149), the 5-year OS and PFS were 93.3% and 30%, respectively (Fig. 6).
Discussion
DF is a rare disease with a variable clinical behavior which has led to a delay in the development of general recommendations for the management of these patients. Although a number of agents showed activity against desmoid tumors, no accepted standard of care exists for systemic treatment of these tumors30.
The 5-year PFS and OS in our series were 30% and 93.7%, respectively, similar to the main pediatric series that reported a PFS and OS of 36.1% and 99.4% (Orbach et al.)21, 31% and 88% (Oudot et al)31, and 44% and 100% (Sparber-Sauer et al)27, respectively, and a PFS of 44% found in the COG study24.
In our series of 16 patients, the 4 patients treated previously to the year 2005 only underwent surgery and surgery and/or radiotherapy in case of recurrence, while after 2005, treatment with MTX/VBL has been used.
The relapse rate after surgery was 76%, being in the upper limit for the range of recurrence reported in the literature. No correlation was observed between quality of resection and incidence of recurrence which is in line with the results of most recent series16.
The response rate to chemotherapy was 51%, and up to 81% if SD cases were included. The best response was PR. Although these results are better than those reported by the COG (19%), EpSSG (35%), and Oudot et al (31%), the small sample size of our series makes it difficult to draw definitive conclusions. We should also be careful in attributing a cause-effect relationship to the treatment modalities used, as spontaneous remission has been reported in 20-28% of the cases32,33.
Response to treatment was slow, as described in the literature. Nevertheless, some authors reported an early improvement in terms of symptom relief34. In our series, patients who receive LDC as first-line therapy showed a trend towards a better prognosis than those who underwent initial surgery (this was already described by others); however, this difference was not statistically significant27. LDC was generally well tolerated, but the first patients in our series required lowering of the VBL dose to 2/3 due to hematological toxicity (in 7 patients). Neutropenia was the most common adverse effect, as found by other authors24. No more chemotherapy with drawal was required after the VBL dose was decreased. In a recent study conducted in Germany, the initial dose of VBL used was 3 mg/m2,27.
The only patient who received imatinib achieved dis ease stabilization after the failure of 3 treatment lines. Previous studies reported that TKI seem to induce long term disease stabilization but are associated with low response rates in terms of tumor size reduction.
Imatinib was the first tyrosine kinase inhibitor proposed in DF, showing a response rate of only 6%, however a 1-year PFS of 66% has been reported35.
Other TKI that have been proposed in DF are pazo paniband and sunitinib36,37. Recently, sorafenib has shown promising results with a 2-year event-free survival of 87% and an objective response of 33% versus 36% and 20%, respectively when compared to placebo38. A recently published review describes common signalling pathways active in DF and provides an up-to-date overview of their therapeutic potential39.
In our series, the response rate to radiotherapy was 50% which is below the response range reported in the literature; however, due to the small number of patients who underwent the treatment, no conclusions can be drawn. In our patients, the absence of complications may be explained by the short follow-up period, as complica tions appear after a mean time of 33 months with a rate of 26% after 20 years40.
The most frequent tumor locations found in our series were in the trunk and limbs, similar to other series; how ever, primary site in the head and neck was lower than that reported in the literature for DF in children20.
We did not find statistically significant differences in results regarding to tumor location and size; however, tumors < 5 cm tended to have a better prognosis.
The 2 patients with FAP showed a quite aggressive behavior of the disease and in both cases the surgery acted as a trigger.
Patients with DF and FAP tend to be younger at disease onset and more often have multifocal and intra-abdominal disease41,42. Surgery is a risk factor for the development of DF in patients with FAP; therefore, in these patients it is recommended to delay prophylactic colectomy43.
Gardner fibroma has a variable course, with a spectrum ranging from spontaneous regression in approximately 5-10% to a relapsing and remitting course in 30%, SD from onset in 50%, and rapid DP in 10%44. Optimal manage ment of patients with DF and FAP has not been defined. Nevertheless, the usefulness of celecoxib, which is also an effective treatment in DF, has been established for advanced adenomas with a decrease in incidence and recurrence45.
As previously mentioned, DF is a disease with an excel lent survival, being the long-term sequelae, an important issue. However, there are only few reports that describe the frequency and nature of them. In the Cooperative Weichteilsarkom Studiengruppe (CWS) publication severe late effects were reported only in 1% of patients who received systemic therapy in contrast to the 20% of patients who were treated by resection(s)27. A high rate of cosmetic and functional sequelae (80%) was found, and in 20% of patients they were severe. This was probably related to the fact that the majority underwent initial surgi cal treatment. We have registered a high number of initial surgeries (72% of the tumors), which in the most modern works is discouraged. The reason was that most of the patients were referred from the Orthopedics department after surgery.
In conclusion, DF is a locally aggressive disease with a high local relapse rate, regardless of microscopic involve ment of the surgical margins. The outcome of the patients in our series is similar to those reported in the literature.
LDC has allowed to achieved SD and even disease remission with low toxicity with a slow initial but continuous response throughout the treatment. Although the small number of our series and the retrospective nature of the study do not allow us to draw any definitive conclusion, we suggest using lower doses of VBL to avoid the need to delay treatment due to hematologic toxicity.
The high rate of sequelae found in our series is probably related to the initial surgery performed in the majority of pa tients and may be avoided by the use of neoadjuvant LDC.