KEY POINTS
• In Argentina, various hospital protocols for COVID-19 patients include drawing blood cultures on admittance, as well as the initiation of empirical antibiotic therapy. However, the usefulness of blood culture in patients with COVID-19 pneumonia has not been proved.
• We found no evidence of early bacteremia in patients suffering from COVID-19 pneumonia. We did find high rates of contaminated cultures. We therefore recommend against the drawing of early blood cultures and initiation of empirical antibiotic treatment.
The Coronavirus Disease 2019 (COVID-19) pandemic has strained the world’s health systems, resulting in high rates of bed occupancy and high costs in personal protective equipment, diagnostic studies, and therapeutic tools. That is why it is essential to find the most efficient diagnostic therapeutic approaches leaving aside unnecessary procedures.
The blood culture is a critical tool for the microbiological diagnosis in febrile patients, which is routinely used in patients with pneumonia requiring hospitalization when bacterial, but not viral, etiology is suspected1. Its diagnostic usefulness in patients with COVID-19 pneumonia has not been proved.
Although many hospital protocols for COVID-19 patients include drawing blood cultures on admittance, as well as the initiation of empirical antibiotic therapy aiming at potential bacterial co-infections, there is scarce evidence and variable criteria for this conduct2,3. Thus, the aim of this study is to describe the diagnostic yield of early blood cultures in patients with COVID-19 pneumonia in a public hospital in Buenos Aires.
Materials and methods
The present observational descriptive study constitutes a sec ondary analysis of a prospective cohort study, for which a detailed description of methods has already been published4. It was carried out in the Internal Medicine Ward of the Hospital General de Agudos Carlos G. Durand, located in Buenos Aires City. This hospital was designated as a referral health care cen ter for COVID-19 patients within the city’s public health system and has in-house availability of real time PCR (RT-PCR) for se vere acute respiratory syndrome Coronavirus 2 (SARS-CoV-2). The Internal Medicine ward has a 50-bed capacity, with around the clock patient admission. The sample was non-probabilistic, including patients (aged ≥ 18 years) admitted to the Internal Medicine ward between April 1, 2020 and July 30, 2020, with COVID-19 pneumonia diagnosis confirmed by RT-PCR in na sopharyngeal swab. In order to diagnose pneumonia, x-rays or chest tomography infiltrates were considered, and/or the pres ence of typical clinical characteristics (pathological findings in pulmonary auscultation associated with dyspnea, cough, chest pain or fever)1. Regarding blood cultures, the automated blood culture system BacT/ALERT® (Durham, NC, U SA) is routinely used at our center. Our main analysis included cultures drawn within a period of up to 5 days from hospital admission. In Ar gentina, hospital-acquired pneumonia (HAP) is defined as one that occurs 4 to 7 days after hospital admission5. The 5 days limit was therefore established in order to detect germs causing community-acquired pneumonia. The decision to perform blood cultures was based on the individual clinical judgment of the treating physician and no systematic protocol has been used. Cultures drawn after 5 days since admission were included as an additional analysis.
Clinical characteristics, laboratory, radiology, and treatment results data were obtained from medical records. All the col lected information came from routine practice and the study had no influence on the diagnostic or therapeutic conduct.
Severe pneumonia was defined if at least one of the following conditions was present upon admission: (a) Respiratory rate ≥ 30/ min; (b) Arterial partial pressure of oxygen (PaO2) < 70 mm Hg or peripheral oxygen saturation (SpO2) ≤ 93% on room air or PaO2/ FiO2 ≤ 300; (c) Lung involvement > 50% on chest radiography6.
The Sequential Organ Failure Assessment (SOFA) Score was calculated for all patients from whom a laboratory report was available within 48 hours of admission7. Since the SOFA index requires PaO2, which was not always available, SpO2 was used in those cases to calculate the SpO2/FiO2 index8. In patients who had arterial blood gas analysis within 48 hours of admission, the Pneumonia Severity Index (PSI) was calculated9.
The general characteristics of the included patients are described using proportions for qualitative variables and median with interquartile range for quantitative variables. The STATA® 14.2 (College Station, TX, United States) software was used.
The study protocol has been reviewed and approved by the Institutional Review Board of the Hospital General de Agudos Carlos G. Durand (Protocol No. 1437). The requirement for informed consent was waived because only routinely collected data from usual care was used.
Results
Between April 1 and July 31, 2020, 675 patients were ad mitted to the internal medicine ward, of which 457 (67.7%) had laboratory-confirmed COVID-19. Among them, 267 (58.4%) had pneumonia and 53 had blood cultures drawn anytime during hospitalization.
Table 1 depicts the demographic and clinical findings of the 38 patients in which blood cultures were drawn within the first 5 days since hospital admission. The median age was 51 years (interquartile range, 39-63 years); 23 (60%) were males. All patients had at least one comorbidity, be ing hypertension and obesity the most frequent ones, each present in around one third of the study population. Upon admission, 26 patients (68.4%) did not meet the criteria for severe pneumonia, and 11 (52.4%) had PSI score ≤ 70. Follow-up data shows that most of them (n = 34, 89.5%) required oxygen supplementation at some point during their stay, and 9 (23.7%) received invasive mechanical ventilation.

Table 1 Clinical characteristics of hospitalized patients with COVID-19 pneumonia and early drawn blood cultures
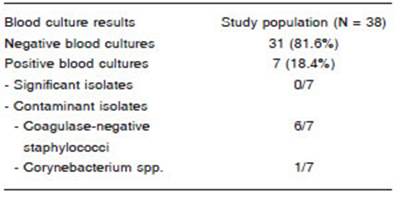
Among the 38 early drawn blood cultures, 31 (81.6%) were negative and the 7 that resulted positive were consid ered contaminated. Thus, there was no significant diagnostic yield (Table 2). Regarding the 15 blood cultures drawn after 5 days of hospital admission, 10 (66.7%) were negative. Among the 5 positive ones, we found 2 significant results (13.3%) and 3 were contaminants (20%). The clinical char acteristics of patients who had blood cultures drawn after five days of hospital admission are depicted in Appendix 1.
Discussion
In this descriptive study on 38 non-ventilated patients with COVID-19 pneumonia, no bacterial coinfection was found by blood culture within 5 days from admission.
Several studies showed that the diagnostic yield of blood cultures in community-acquired pneumonia is very low (5-25%)1,10. Local evidence suggests the same, with diagnostic rates of 18.8% in an argentine study11. A yield even lower (8.2%) was found in a Chilean study12. Considering this, our findings showed no evidence of its usefulness in patients with COVID-19 pneumonia. Therefore, we advocate that blood cultures in COVID-19 patients, as well as antibiotic therapy, be only used in face of clinical deterioration or suspicion of hospital-acquired infection.
Moreover, a high proportion of blood culture contami nation was identified (18.4% of blood culture pairs grew at least 1 contaminant bacteria). This number nearly doubles the usual percentage of contaminated blood cultures drawn in patients with community-acquired pneumonia (10%)13. As stated by Hughes and col., this could be explained by unfamiliarity of additional personal protective equipment worn by healthcare workers taking blood samples from patients with suspected or confirmed COVID-1914.
Our findings on low diagnostic yield of blood cultures for COVID-19 patients as well as the high proportion of those that yielded contaminants correlate with other published studies14,15.
Despite some significant positive results of blood cultures drawn in patients after five days of hospital admittance, they still show a high rate of contaminants. Furthermore, significant positive results might be attributed to hospital-acquired infections.
Additionally, we observed that while most patients had PSI scores I or II upon admission (usually considered as candidates for outpatient treatment), the vast majority of them (89.5%) required oxygen therapy during their stay16. Although further investigation is needed, we suggest cau tion in using the PSI score to decide outpatient care of patients with COVID-19 pneumonia.
Our study has limitations. First, blood cultures were drawn in a non-systematic fashion. Thus, they are not representative of all the patients admitted to the internal medicine ward. Second, the sample size is small and therefore the power to detect microbiological isolation from blood cultures is low. However, being a small subset of patients, most of them with risk-conferring co morbidities or clinical deterioration, a higher diagnostic yield is expected from blood cultures, reinforcing the clinical implications of not finding any microbiological isolation. Third, this study lacks a pre-pandemic control group to compare diagnostic yield and contamination rates nor have these rates been published for our study population. Therefore, we cannot establish if the observed rates represent a significant variation of standard care at our center. To the best of our knowl edge, this is the first study to examine the diagnostic yield of blood cultures in COVID-19 patients in a public hospital in Buenos Aires City.
In conclusion, we found no evidence of early bactere mia in patients with COVID-19 pneumonia. We therefore recommend against the drawing of early blood cultures and initiation of empirical antibiotic treatment.