KEY POINTS
• Influenza infection is a global public health problem, affecting millions of people, with high morbidity and economic burden. In Argentina, influenza-associated mortality is estimated at 6/100 000 person-years, but it is higher among men ≥ 65 years.
• Most patients in this study were older than 70 years and had at least one coexisting illness. However, in-hospital mortality was not higher than mortality reported in pre vious series of non-pandemic influenza. Bilateral lung compromise was more frequent among ICU patients compared with non-ICU patients in both chest x-rays and chest computed tomography. Hepatic enzyme impair ment was more frequent in ICU patients. Additionally, proBNP was higher among ICU patients. A total of 39.1% of 143 hospitalized patients required admission to ICU.
Influenza is a latent public health problem, affecting millions of people throughout the planet. It is an important cause of morbidity and mortality, especially for certain susceptible populations1,2. Common risk factors for presenting a severe influenza disease are aging, cardio vascular disease, malignancy, immunosuppression, and end-stage organ failures like liver or chronic renal disease. Obesity and pregnancy have also been associated with an increased risk of negative outcome3,4.
Periodic changes in the antigenicity of the virus, and also bacterial co-infection, can lead to severe respiratory illness5. Approximately 30-40% of hospitalized patients with laboratory-confirmed influenza are diagnosed with acute pneumonia6 and admission to intensive care unit (ICU) ranges from 5 to 10%7. In Argentina, influenza‐as sociated mortality is estimated at 6/100 000 person‐years, and is higher among men ≥ 65 years old8. Also, seasonal influenza imposes high morbidity and an increasing eco nomic burden on the region9.
Knowledge of the baseline characteristics and out comes of hospitalized patients is crucial for public health officials engaged in planning interventions to address local outbreaks. Thus, the objective of this study is to describe clinical characteristics, laboratory and imaging findings of patients who required hospitalization during 2019 in a high-complexity hospital located in Buenos Aires City.
Materials and methods
For this retrospective, single-center study, we recruited pa tients from January 1st to December 31st, 2019. Data were obtained from medical records of adult patients (18 years of age or older) with laboratory-confirmed influenza, hospitalized in a high-complexity university hospital located in Buenos Aires city.
All patients with influenza-like symptoms were screened at the emergency department. Influenza-like symptoms included sudden onset of fever, dyspnea, headache, cough, rhinorrhea, muscle-ache, acute exacerbation of chronic obstructive pul monary disease, gastrointestinal symptoms (such as nausea, vomiting, or diarrhea), and pneumonia. Hospital admission was decided by physicians based on patients’ coexisting medi cal conditions, age, and acute onset of respiratory symptoms. Only those with confirmed influenza infection by real-time reverse transcriptase-polymerase chain reaction (RT-PCR) assay of nasopharyngeal-swabs were included. Other respira tory viruses including adenovirus, respiratory syncytial virus, parainfluenza viruses, rhinovirus, enterovirus, coronavirus, and bocavirus were also screened by RT-PCR.
On admission, patients were examined by chest x-rays (Rx) or chest computed-tomography scans (CTs), and laboratory testing. Laboratory assessments consisted of a complete blood count, blood chemical analysis, coagulation testing, assess ment of liver and renal function, measures of electrolytes, procalcitonin, and pro-B-type natriuretic peptide (proBNP). Finally, the vaccination status was compiled from the medical record. Only patients who were vaccinated within the year were counted as immunized.
Clinical outcomes were followed up to March 2020. The study was approved by our hospital Ethics Committee in October 2019.
Categorical variables were summarized as counts and percentages and compared with the Fisher’s exact test. Con tinuous variables were expressed as medians and interquar tile ranges or simple ranges, as appropriate. Variables with normal distribution were tested by the t-test and variables without normal distribution were tested by the Mann-Whitney test. A two‐tailed P‐value < 0.05 was considered significant. No imputation was made for missing data. We used STATA 13.0 for all analyses.
Results
Demographic and clinical characteristics of patients are shown in Table 1. Of the 143 patients included in the study, 79 were women and 64 were men. The median age was 71 years (IQR 60-82). Among the overall population, 111 (77.6%) were older than 70 years, and 113 (79%) had at least one coexisting illness. Chronic obstructive pulmo nary disease was the most frequently observed (30.0%), followed by asthma, chronic heart disease, and active cancer, each one representing 11% (16 patients). Immunosuppression was registered in 26 patients (17.9%). In this subgroup, more patients with solid organ transplant remained at the general ward than in the ICU (12 [13.8%] vs. 1 [1.9%]; p = 0.016).
Fifty-six patients (39.1%) required ICU admission and the rest were treated in the general ward. Sixteen patients (11.1%) underwent invasive mechanical ventilation and 40 (27.9%) non-invasive ventilation or high-flow nasal cannula. Five (9%) of the 56 patients requiring ICU died. The average length of stay was 7 days (IQR 4-13) for all patients, 5 days (IQR 3-10) for those who did not require ICU, and 10 days (IQR 6-16) for those who did.
The vaccination status was known in all cases, with a vaccination rate of 32.1% (28) in non-ICU patients and 26.7% (15) in ICU patients. Three (6.9%) vaccinated and 13 (13%) unvaccinated patients required invasive mechanical ventilation (p = 0.39).
A total of 141 (98.6%) patients were infected by influ enza virus type-A, 88 (61.5%) by subtype H1N1, and 53 (37.0%) by H3N2. Most cases were reported during the 24th to 32nd epidemiological weeks (winter season) of the Southern hemisphere. The temporal distribution and the distribution of cases by viral type and subtype are detailed in Figures 1 and 2.
Coinfection with other respiratory viruses was detected in 22 (15.3%) patients. Rhinovirus (n: 7 [74.8%]) was the most frequently registered, followed by respiratory syncytial virus (n: 6 [4.1%]), coronavirus (n: 3 [2.0%]), parainfluenza (n: 3 [2.0%]), adenovirus (n: 2 [1.3%]), and bocavirus (n: 1 [0.6%]).
Regarding clinical findings on admission, fever was present in 93 (65.0%) patients. The second most common symptom was dyspnea in 83 (58.0%), followed by cough (n: 75 [52.4%]) and rhinorrhea (n: 28 [19.5%]); diarrhea, nausea, or vomiting (n: 7 [4.8%]) were uncommon. Dys pnea was more frequent in ICU patients (n: 39 [69.6%] vs. n: 44 [50.5%]; p = 0.0257).
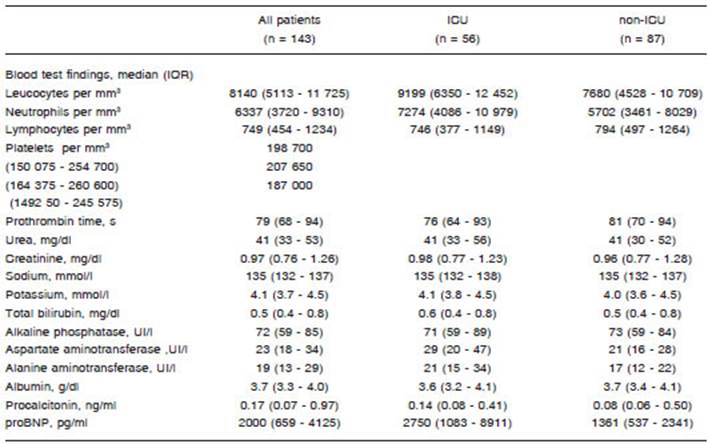
Table 2 shows laboratory findings. ICU patients pre sented significantly higher proBNP levels than non-ICU patients (28 [50.0%] vs. 11 [12.6%]; p < 0.001). Hepatic enzyme impairment was more frequent in ICU patients than in non-ICU patients (aspartate aminotransferase, n: 21 [37.5%] vs. n: 7 [8.0%]; p<0.001 and alanine amino transferase, n: 14 [25%] vs. n: 5 [5.7%]; p = 0.0018). No associated involvement of alkaline phosphatase, bilirubin, or prothrombin time was observed.
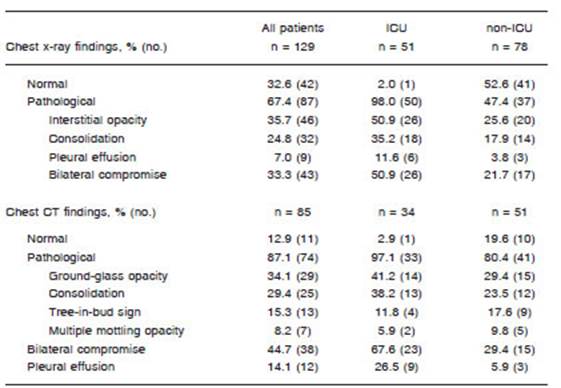
Table 3 shows Rx and CT imaging findings. Of 129 Rx performed at admission, 83 (67.4%) revealed abnormal results. The most common patterns observed were: inter stitial opacity (35.6%), consolidation (24.8%), and pleural effusion (6.9%). Also, 33.3% of the patients presented bilateral compromise. Moreover, almost all ICU cases (50 [98.1%]) showed pathological findings in Rx in contrast with admissions to general ward (37 [47.4%]). A total of 85 chest CTs were performed. No CT abnormality was found in 11 (12.9%) studies. Ground-glass opacity was found in 34.1%, followed by consolidation in 29.4%, tree in bud sign in 15.2%, and multiple mottling opacity in 8.2%. Bilateral compromise was informed in 44.7% and pleural effusion in 14.1%. Bilateral compromise was more frequent among ICU patients compared with non-ICU patients in both chest Rx (26 [50.9%] vs. 17 [21.7%]; p<0.001), and chest CT (23 [67.6%] vs. 15 [29.4%]; p = 0.002).
Discussion
In this cohort study, we report clinical characteristics and risk factors associated with clinical outcomes in patients with laboratory-confirmed influenza who required hospi talization during 2019. We found that the overall mortality was similar to that reported in previous series. Noticeably, ICU-mortality was lower despite the fact that the majority of the cases reported in our study were older than 70 years and had at least one coexisting illness10-14. Also, the rela tive number of patients admitted to ICU was higher. This may be attributed to the fact that age is not a restriction for invasive vital support in our ICU.
As regards chronic medical illnesses, we found a lower number of solid organ transplant patients hospitalized in ICU than in the general ward. Immunocompromised individuals, such as organ transplant recipients, are generally deemed to be at an increased risk of morbidity and mortality from influenza infection15,16. Nevertheless, our results are similar to those of a recent report showing that immunosuppressed patients had better outcomes and less organic failures than those who were immunocom petent. Stahl et al. found differences in ICU admission in immunocompetent vs. immunosuppressed patients (14% vs. 7%, p = 0.07), as well as in the requirement of me chanical ventilation (11% vs. 4%, p = 0.41), vasopressors (12% vs. 3%, p = 0.01), and mortality (12% vs. 3%, p= 0.23)17. In this sense, severe influenza infection is often associated with a hyperinflammatory phenotype, most likely the consequence of a dysregulated host response to influenza similar to sepsis, explaining the better outcomes observed among immunosuppressed patients18,19. It would be interesting to deepen the analysis of clinical and im munological characteristics of influenza in this group of patients to draw conclusions and extrapolate information to the general population.
In relation to the laboratory findings, the impairment of hepatic enzymes, mainly aspartate aminotransferase (ASAT), was far more frequent in ICU patients. In a re cently published research, an ASAT value superior to 68 IU/l was identified as a better predictor of 3-month mortality (hazard ratio 7.68 [IC 95% 1.6-35.1]) than other variables such as creatinine and PaO2/FiO220. Additionally, proBNP was higher in ICU patients. High levels of ProBNP have been reported to predict poor prognosis in patients with confirmed influenza21.
Regarding imaging studies, in our series only one patient of those requiring ICU had a normal result. More extensive lung compromise was seen in ICU cases, with more frequent bilateral involvement in both chest Rx and chest CTs in comparison with non-ICU patients. Similar data were found in other series where a higher percent age of pathological radiographic findings were detected in patients with a worse prognosis22-24.
Our study has several limitations. It is an observational study of a single center and data from other Argentine centers are necessary to know the impact of influenza in hospitalizations. Also, as previously noted, no post-ICU follow up was performed.
We conclude that in 2019 both the mortality and the severity of the cases were similar to those published in previous series of non-pandemic influenza. Analysis of annual data would be valuable to document the severity of influenza hospitalizations by age‐group and comorbidities according to the circulating influenza viruses. Multicenter data are needed to get a more complete picture of the hospitalization burden related to influenza.