KEY POINTS
Current knowledge
• The advent of the pandemic caused a change in the behavior of the population that caused people not to go to health centers and the loss of control of prevalent pathologies and healthy habits.
Article contribution
• Half of the people who needed to access the healthcare system refused to do so. The main reasons for this were to abide by the recommendation not to leave their home, physical impossibility of accessing the healthcare system and fear of infection. This caused many patients to have difficulty accessing their treatments and lose control of cardiovascular risk factors.
Medical advances throughout the 20th Century led to vast improvements in life expectancy worldwide1,2. Transformative developments such as the use of vaccines, discovery of antibiotics and efforts to increase disease awareness and prevention led a substantial transforma tion of the public health landscape. With increased life expectancy, cardiovascular disease became the leading cause of death3. The novel coronavirus disease (CO VID-19) pandemic now threatens to upset this long-term trend and appears as a new challenge to even the most solid healthcare systems worldwide. As an infectious disease, SARS-CoV-2 represents an obvious threat as a direct hazard to the population, especially to those with advanced age and with comorbidities that increase risk of death. A second, less understood hazard is the effect COVID-19 risks and healthcare measures on the population psychology: the physical distancing measures (either directed by governments or self-imposed by the people) required to contain the spread of the virus cre ated, as an unexpected consequence, a sudden change in the population behavior that led to a negative impact in healthcare management. Multiple educational campaigns were needed over decades to gain population behaviors that improved cardiovascular disease (CVD) detection and prognosis4. However, recent reports already show a dramatic reduction in CVD treatment worldwide. Chinese reported patients suffering from heart attacks waited four times longer than the historic average time to call for medi cal help5. In Europe and USA, there was a 40% reduction in the number of primary angioplasties in patients with acute coronary syndrome with ST segment deviation6-8.
On May 9th, 2020, Argentina had completed 10 weeks of mandatory social isolation, COVID-19 had infected 5776 people and claimed 300 lives9. However, most of outpatient clinics in public and private institutions have been closed.
Patients are delaying their medical check-ups and have difficulty obtaining prescriptions, limiting access to medication. This represents an imminent threat from a car diovascular perspective. Multiple reports worldwide point to a large reduction in the number of medical visits, even urgent visits. The reason for this decrease is however not fully understood. The aim of this study was to understand the reasons that led to this detrimental change in social behavior and determine the impact of the pandemic on health control in general and on cardiovascular risk fac tors in particular.
Material and methods
The study was carried out following the medical research recommendations suggested by the Declaration of Helsinki, the Good Clinical Practice Guidelines, and current legal regulations. All respondents gave their express consent to participate in the survey.
Surveys are a common method for assessing patient per ceptions, knowledge, beliefs, attitudes, and behavior related to health10,11. We performed a cross-sectional, web-based survey using an online questionnaire developed using Google Forms, an online survey software, between 9 and 17 May 2020. The inclusion criteria were that the respondents belong to general population from Argentine Republic and were older than 16. Physicians and health personnel were expressly excluded from the survey. The survey was distributed via the What sApp application for smartphones among subjects across the Argentine territory using a combination of convenience (social assistants, union leaders, employers, and teachers) and snow ball sampling. When respondents had completed the survey, they received a message encouraging them to disseminate the survey. Respondents were informed that their participation was voluntary and all gave express consent to participate.
The research team drafted all the items, instructions, and answer options to generate a first version and conduct a re stricted pilot survey. Through informal discussion groups with experts and semi-structured individual interviews with subjects not belonging to the healthcare system, the responses from the pilot test were used to improve the readability of the survey content, determine the adequate vocabulary, and evaluate if the items were culturally applicable. Pilot test interviewees included subjects of different ages, gender, and socioeconomic levels. After this stage, a second version of the instrument was made available to the broad population.
In this investigation, the subjects completed a survey on the perceptions, knowledge, beliefs, attitudes, and behavior related to the COVID-19 pandemic in the healthcare setting. Demographic data such as age, sex, educational level, employment situation or medical coverage were collected. Questions were designed to learn about the opinion of each individual regard ing the current situation of the Argentine health system and about the potential behaviors in medical consultations. Fur thermore, the survey provided information on the participant´s perception of their own health and the presence of chronic diseases that could increase the risk of COVID-19. In addition, questions about the impact of the pandemic on cardiovascu lar risk factors, vaccination, correct use of pharmacological therapies and habits such as exercise, diet, or alcohol intake were collected. The survey also collected information on car diovascular history and its care during the pandemic.
Continuous data were compared between groups, using the T test for normal distribution or the Mann-Whitney-Wilcoxon test for non-normal distribution. Continuous variables were expressed as mean ± standard deviation and categorical variables as percentages. A two-tailed p-value < 0.05 was considered statistically significant. STATA 11.1 software pack age was used for all statistical analyses.
The survey was carried out between May 9th and May 17th, 2020, seven weeks after the start of compulsory social isolation, which began on March 20.
Results
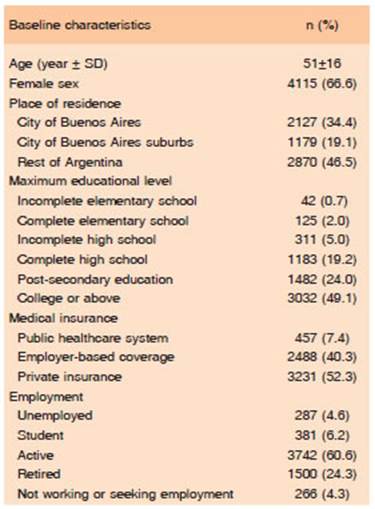
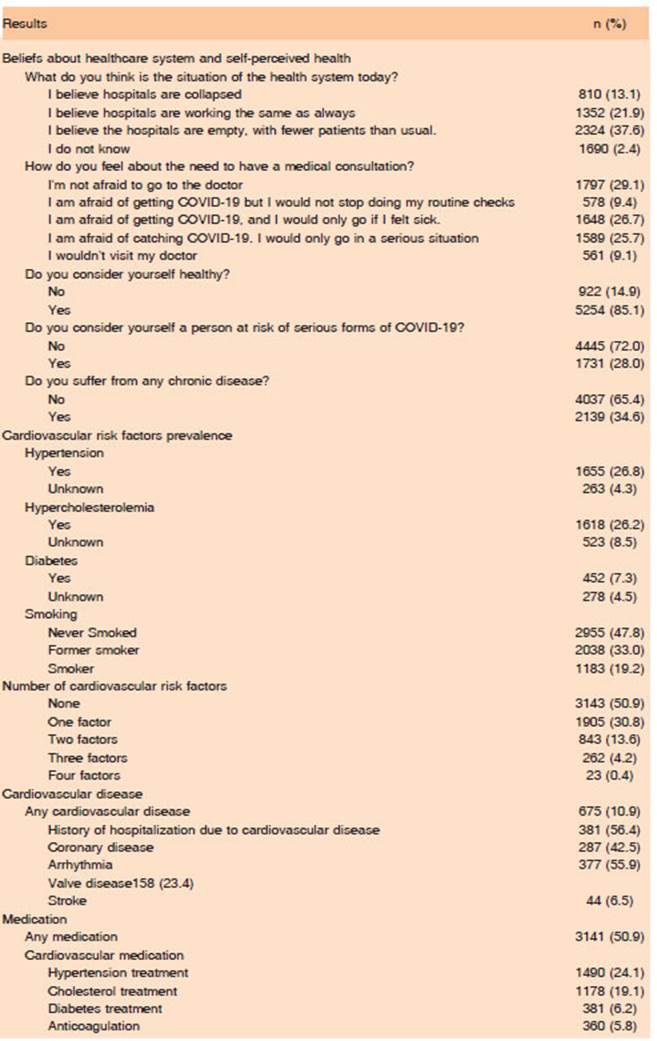
This survey received 6176 unique responses. Basal population characteristics are described in Table 1. Me dian population age was 51±16 years, with 2/3 female respondents. Half of participants had completed college or more, 24% completed some post-high school learning, 19% had completed high school, and 8% did not complete high school. One out of every seven of respondents believed that hospitals were collapsed at the time of the survey. Almost 70% of respondents manifested some level of fear of visiting a physician, whereas about a third of the respondents would only visit a physician on severe cases or would not consult under any circumstances.
Even if 85% of respondents considered themselves as healthy, 28% revealed belonging to an at-risk group, 50% manifested at least one cardiovascular risk factor and 10% disclosed cardiovascular disease (Table 1)
One third of respondents manifested having a desire or need in at least one occasion of visiting a physician but, of these, 48% avoided it. The main reasons listed by the respondents for avoiding the visit were: 1) a recom mendation of staying home (40%); 2) lack of access to the physician (35%); and 3) fear of contagion (26%) (Fig. 1). However, 21% of those that avoided the visit considered that avoiding the visit was detrimental to their health.
In contrast, 1085 respondents (18%) tried to visit a physician despite the quarantine’s limitations. A total of 509 respondents (47%) declared that accessing the healthcare system was easier than usual, 322 (30%) did not note any differences, but 220 (20%) found that access the health care system was more difficult and for 34 (3%) it was not possible. The only two variables that were independently associated with a perception of access to the healthcare system were the own perception of belonging to a risk group (OR 1.3; IC95% 1.02-1.83; p = 0.03) and having manifested fear of the visit to a physician (OR 1.5; IC95% 1.11-2.08; p = 0.008). The most common forms of consultation were via email, telephone or WhatsApp (41% of cases), fol lowed by a conventional visit to a physician’s office (35% of cases), any telemedicine platforms (10%), a call to an emergency number (10%) and a call to an ambulance to the respondent’s address (4%). There were no statistical differences on the mode of consultation between those that perceived more difficulties to access the healthcare system and those that did not. One of 5 respondents had a difficulty to obtain a prescription for a medication and 5% stopped the use of at least one drug. This last data point is even more alarming among those with cardiovascular disease: 7% of these patients suspended at least one medication (OR 1.7; IC95% 1.2-2.5; p = 0.002) (Table 2).
After the implementation of the quarantine restrictions, many changes in population habits and behaviors were evident. The most dramatic change was a reduction in physical activity, manifested by 62% of respondents. Simi larly, there was an increase in salt consumption among those with a diagnosis of arterial hypertension and of fats among respondents that manifested dyslipidemia. These nutritional changes, together with an increased alcohol use manifested by nearly 10% of respondents, contributed to the increase in body weight revealed by 38%. Almost half of them did not measure their own blood pressure during the period lasting almost two months since the beginning of the quarantine’s restrictions. Of those that controlled their blood pressure at least once within this period, 16% acknowledged higher blood pressure than before the start of the quarantine. The data is even more alarming when analyzing the most socially vulnerable groups (unem ployed, people without complete high school studies, and those that use the public healthcare system) (Table 3).
There was an 18% increase in the rate of flu vaccination among those with an indication for the vaccine, compared to 2019 (58% vs. 69.0%; p < 0.0001). Moreover, 52% of those that did not obtain the flu vaccine, manifested desire, or intention of getting it.
Discussion
Two months after the quarantine movement restrictions were imposed in the Argentine Republic, a third of the surveyed population wished for or needed to visit a doctor. However, half of these did not visit any doctor’s office. This behavior does not seem to be exclusive to the Argentine population; a recent survey conducted by the Kaiser Fami ly Foundation in the United States of America revealed that almost half of respondents skipped or delayed care due to COVID-1912.The main reasons for this behavior were 1) a respect for the indication to stay home, 2) being un able to access the doctor, and 3) fear of contagion during the doctor’s visit. Historically, schools and hospitals have been temples that guard the most expensive treasures of modern societies. In times of pandemic, schools are closed and people are afraid to go to hospitals. Although this is an alarming reflection for any society, it is even more so if it occurs within a Latin American society due to the profound socioeconomic inequities in this region13,14. In 2016, the Argentine government established a policy of universal access to health as a strategic priority. The goals of such policy were to ensure that every person in the Argentine territory was able to access the required healthcare services, while maintaining a good quality of care and preventing any financial hardships due to excessive costs15. While indisputably a laudable objective, it remains far from being reached. A main barrier to the successful implementation of this objective is the large fragmentation of the Argentine healthcare system: 60% of the population relies on different types of employer-based coverage, 30% uses the public healthcare system, and 10% has direct private health insurance16. In addition to the common barriers to accessing the health system (availability, financial and administrative), self-imposed barriers are added by the users themselves during the first months of the COVID-19 pandemic. These new barriers originated from public communication strategies that prioritized “stay at home” objectives above any other need. It is not surprising that the most vulnerable people abstained from visiting a doctor in larger proportions and that, when they did, they had to go to an emergency ser vice more frequently. Historically, pandemics have been experienced unequally, with higher rates of infection and mortality among the most disadvantaged communities-particularly in more socially unequal countries17. As of June 27, 2020, the prevalence of COVID-19 in the city of Buenos Aires was 8.47 cases per 1000 inhabitants, while in vulnerable neighborhoods the prevalence is 52 cases per 1000 inhabitants18,19.
Telemedicine is becoming an alternative to safely connect patients with physicians. However, few providers have the required infrastructure to provide this service20,21. The few existing telemedicine platforms belong to private healthcare systems, which prevents access to those vul nerable and with limited financial resources. Moreover, because the vast majority of healthcare providers do not yet recognize telemedicine as a medical service, those physicians providing it may not be remunerated for their work.
In the first two months of the quarantine, a loss was ob served in the practice of healthy behaviors. As expected, the greatest impact of confinement was observed in the decrease in physical activity; almost two thirds of the popu lation reported doing less physical activity than prior to the pandemic. We do not know if the remaining third did not decrease their exercise regimen because they continued training or because they were already sedentary. Regard less of the reasons, these numbers are alarming, since not reaching the minimum dose of 150 minutes of moderate intensity weekly exercise recommended by the guidelines is associated with an increase in total mortality and major cardiovascular events22,23. Similarly, the increase in the consumption of salt and fats in the diet was reflected in the increase in blood pressure values and a disturbing increase in weight reported by 38% of the respondents. These findings, added to the fact that 1 out of 5 patients had difficulties in obtaining a medication prescription and that 5% of them abandoned at least one medication, heralds an increase in cardiovascular events and total mortality24,25. This alarming situation is not restricted to outpatient care. Shortly after the quarantine movement restrictions, data from an industry group representing private healthcare system nationwide, ADECRA+CEDIM, revealed that visits to emergency rooms due to coronary syndrome decreased by 62%, while calls for stroke, de creased by 46%. This led to a reduction by 59% in the number of angioplasties, and a decrease of 58% in central cardiac surgeries26.
Considering that 28% of the 336 823 deaths that oc curred in Argentina during 2018 were due to cardiovascular events27, the dramatic reduction in outpatient visits, emer gency calls and cardiovascular procedures is alarming. Between 1995 and 2010, there was a 30% reduction in cardiovascular mortality in Argentina (IMPACT-CHD AR GENTINA study), of which about half can be attributed to angioplasties, surgeries, and other therapeutic procedures, and a third to better control of risk factors such as hyper tension, diabetes, and dyslipidemias28. However, we can expect up to 9000 deaths annually due to coronary disease and up to 30 000 more deaths annually due to cardiovas cular disease if the population abandons their control of the cardiovascular health due to COVID-19 concerns.
Beyond the changes in measurable habits, preventive and compulsory social isolation leads to a loss of social interaction between people, which is a determinant of the appearance of depression, which is also a determinant of cardiovascular disease29,30.
A limitation of the methodology used is that it does not allow us to know the number of people who received the questionnaire in order to report the response rate. Beyond this limitation, “snowball” sampling constitutes a non-probability sampling technique that is increasingly used in qualitative research, especially in the framework of the social sciences and human behavior. This sampling technique, used in conjunction with new technologies and social networks, allowed us to reach a large number of individuals in a short time, allowing us to learn about the barriers perceived by the population to access the health system. This methodology is validated and is of recognized utility to gain access to relegated or marginalized popula tions31. In the first months of compulsory social isolation, where the “stay home” message prevailed, walking the streets and even more going to a health center or meeting a health worker was at least taboo if not a flagrant violation to the established standards of care.
Despite the efforts made to achieve a representative sample of the entire community, the demographic char acteristics of our population, where half have a university education and private health insurance is typical of the most affluent neighborhoods of the city of Buenos Aires and large urban centers32. Thus, it is possible that the situation is even more worrying among the less favored from the socio-economic point of view.
In conclusion, on times of the COVID-19 pandemic, the threat to public health arises not only from the damage derived from the virus but also from the loss of continuity of care for many other pathologies. Half of the people who needed to access the healthcare system refused to do so. The main reasons for this were to abide by the recom mendation not to leave their home, physical impossibility of accessing the healthcare system and fear of infection. The message to the community should be both to maintain social isolation and not to abandon the treatment of pre-existing pathologies. All healthcare systems must open face-to-face and remote communication channels that guarantee access to the System for all citizens.