KEY POINTS
Current knowledge
• Local data indicates that people with advanced cancer have insufficient access to palliative care (PC). Given that treating oncologists are the ones who decide wheth er to include PC in their patients´ treatment plan, it is important to investigate oncologists´ beliefs and knowl edge about PC and their attitudes towards PC referral.
Contribution of the article to current knowledge
• Through a survey of clinical oncologists listed in the main associations in Argentina, information was obtained on the rates and timing of referral to PC and its predictors, the criteria used for referral and the reasons for not doing so, their beliefs and knowledge about the benefits of PC for a patient with advanced cancer, and the availability and complexity of associated PC services.
Patients with advanced cancer have multiple and com plex physical, psychosocial and spiritual needs. Palliative care (PC) is the active, holistic care of individuals with se vere health-related suffering and their caregivers1. Several controlled studies have demonstrated that the approach of PC for people with advanced incurable cancer improved their quality of life (QoL)2,3 and their psychological and physical symptom burden4, and increased survival length for some types of cancer3,5. It was also shown to allow less aggressive end-of-life care6,7 and to reduce healthcare costs7,8. Despite this, PC remains underutilized for these patients in developing countries. Recent research in Latin America reveals that less than 10% of people with cancer in need of PC access it9,10.
The evolving model of PC encourages its early intro duction into the management plans of patients with cancer. Its inclusion is recommended as close as possible to the diagnosis of an incurable disease, regardless of whether patients follow life-sustaining or curative treatments11- 14.
Usually, the oncologist is the person who enables and gives participation to the PC specialist. The interphase between these two care domains is more complex than just referring the patient to another specialist and should ideally occur in a longitudinal and coordinated manner. Previous research on oncologists’ attitudes towards re ferral to PC in highly developed countries revealed that the main hindering factors were oncologists’ inaccurate knowledge of the field of palliative medicine, their negative beliefs about the benefits of PC, and the lack of uniform criteria to identify the reasons and timing to refer a patient with cancer15- 21.
Former studies in Argentina showed that the concurrent integration of PC into standard oncology, if any, usually occurs late in the course of the disease, as an isolated event with different physicians participating sequentially22,23. The possible causes from the perspective of oncologists have not been investigated. Given that the beliefs and attitudes of oncologists regarding PC inclusion could be influenced by social, cultural, and economic determinants, the generation of local evidence is needed to understand which factors motivate or prevent referral in our country. Therefore, we surveyed a nationally representative sample of oncologists to address: 1) the rates and timing of re ferral of their patients to a specialized PC service and its predictors, 2) the criteria that they use to decide the refer ral and the reasons for not doing so, 3) their beliefs and knowledge about the scopes and benefits of PC, and 4) the availability and complexity of associated PC services.
Materials and methods
Study design
Exploratory descriptive, cross-sectional, and quantitative study, granted by the National Cancer Institute, Argentina. An 11- item closed-ended questionnaire was developed to identify potential barriers, attitudinal and perceptual items about re ferring a patient with advanced incurable cancer to PC. The survey content was designed by a focus group of oncology and PC specialists skilled in PC education and training, on the basis of their experience and the review of existing relevant literature. The study and the final version of the questionnaire were reviewed and approved by the Ethics Committee Claude Bernard, Rosario, Santa Fe, Argentina. The acceptance to answer the questionnaire was considered to be a consent to participate.
Inclusion and exclusion criteria
A nationwide list was drawn of clinical oncologists practicing in the public and private sectors of the 24 provinces in the Argen tine territory. Eligible participants were all physician members of the main associations of Clinical Oncology of Argentina, which represents the large majority of medical oncologists in the country. Oncologists who had retired or did not respond after 3 contact attempts were excluded.
Data collection
Participants were interviewed by telephone between Janu ary 2018 and March 2019. The main outcomes were the frequency and timing of PC referral and the reasons for referring/not referring a patient to PC. Secondary outcomes included oncologists’ knowledge and perceptions towards the scopes and benefits of PC for cancer patients, the complexity of available PC services, and the association between their personal, professional, and environmental characteristics and their referral behavior.
Oncologists were asked how often they referred their pa tients to PC services (usually, exceptionally, never), and which of the different existing types of PC services in Argentina was present in their practice. Options were: a PC specialist (anes thetist/clinician/other) that agrees to receive patients requiring PC, a basic team (PC specialist and a nurse or a psychologist), a multi-professional interdisciplinary team skilled in PC either with inpatient facilities or mobile hospital-based team, or no PC team/specialist to refer a patient in need of PC. They were asked for the existence and reasons for collaborative (close or interdisciplinary) work with a PC team or specialist.
Options were: yes; no, because it is not necessary; no, due to economic barriers to access PC services; no, because there is no accessible PC team/specialist; or no, due to disagreements with the accessible PC team/specialist.
The oncologists who usually or exceptionally referred patients to PC services were asked for the criteria they used for a referral. Options were: limited survival, the presence of advanced disease with good functional status [Eastern Cooperative Oncology Group- ECOG24 performance status score=1], the presence of advanced disease with poor func tional status (ECOG≥2), the presence of uncontrolled pain, the presence of any other uncontrolled symptom, the patient can no longer go/be taken to consultation, there are no more onco-specific treatment options, communication difficulties with patient/family members, or very demanding patient/fam ily. Those who exceptionally or never referred their patients to PC services were asked about the reasons. Options were: I can provide PC myself, a PC team/specialist that fulfills this role is not identified, referral process would take a long time, the patient would feel abandoned, a PC approach is not meaningful/beneficial/a priority, the patient cannot afford PC/ non-coverage by the health system, disagreement with the PC team/specialist, or I prefer to handle the patient personally. All oncologists were asked about the moment which they consid ered optimum for referring a patient with incurable cancer to PC, the main benefit/s provided by PC for a patient with ad vanced cancer, and which components of the WHO definition of PC25 they considered most important. These components were: “PC provides pain and other distressing symptoms re lief”, “it affirms life and regards dying as a normal process”, “it intends neither to hasten or postpone death”, “it integrates the psychological and spiritual aspects of patient care”, “it offers a support system to help patients live as actively as possible until death”, “it offers a support system to help the family co pe during the patient’s illness and in their own bereavement”, “it provides an interdisciplinary approach”, “it enhances QoL and may also positively influence the course of illness” or “it is applicable early in the course of illness, in conjunction with other therapies that are intended to prolong life”.
Data Analysis
Respondent characteristics and referral practices were summa rized by descriptive statistics using frequency and proportions. Pearson´s c2 or Fisher´s exact test was used for comparisons. A multiple correspondence analysis (MCA) analysis was used to spatially visualize probable associations among the oncologists’ characteristics, attitudes, and opinions. A multiple logistic re gression analysis was performed to determine the oncologist´s personal and daily practice characteristics that were indepen dently associated with the frequency of referral (frequently referred versus exceptionally/never referred). Results are shown as the level of significance (P), odds ratio (OR), and the lower and upper values for a confidence interval of 95%. P<0.05 was considered statistically significant. All analyses were conducted using Minitab 16 version 1.0 (2010) Minitab Inc. and IBM SPSS V25 (2017) software.
Results
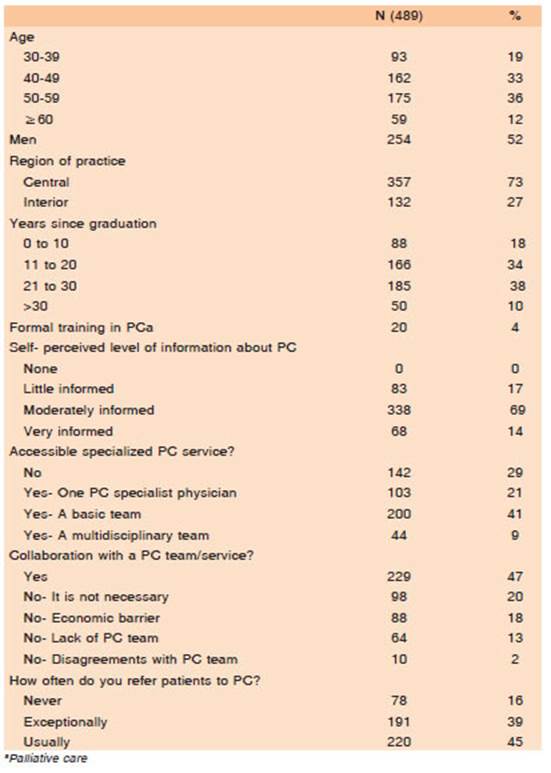
Participant flow chart is shown in Fig. 1. Four hundred eighty-nine medical oncologists completed the survey, representing a response rate of 59%. Demographics and other oncologists’ characteristics are shown in Table 1. Most practiced in the country’s most populated area (84% of the inhabitants), which includes Buenos Aires, the country’s capital. The majority said to be moderate to well-informed about the PC discipline (N = 406; 83%) and to have some level of accessible PC service (N = 347; 71%).
The oncologists who usually referred their patients to PC (N = 220; 45%) did so mainly due to uncontrolled pain, the impossibility of curative treatment, or advanced disease with poor performance status. Those who excep tionally referred their patients to PC (N = 191; 39%) did so mainly because of uncontrolled pain or other uncontrolled symptoms. Only 19% of the oncologists who usually re ferred their patients and none of those who exceptionally referred their patients did so early in the course of the disease (a metastatic disease with ECOG = 1) (Table 2). When asked for the reasons for exceptional or non-referral to PC, oncologists who exceptionally referred their patients argued that PC was not a priority or a valuable contribution, and/or that they could provide adequate care themselves. Those who never referred their patients (N = 78; 16%) mostly expressed that they did not identify an accessible PC service (Table 2).

Table 2 Criteria used for usual/exceptional referral and reasons for exceptional/no referral of patients with cancer to a specialized palliative care service
All oncologists were asked about the moment they considered optimum for referring a patient with incur able cancer to PC. One hundred seventy-eight (37%) answered “close to the end of life”, 128 (26%) “as early as possible after the diagnosis of incurable disease”, 64 (13%) “when there are no other therapeutic alternatives”, and 51 (10%) “at the onset of symptoms”. Twenty-nine (6%) expressed that they were not able to determine the proper time for referral, and the remaining 39 (8%) did not answer this question. Depending on the answer, they were grouped into two categories: using early-derivation or late-derivation criteria. Based on this classification, 179 (36%) of the participants chose early-derivation criteria and 242 (50%), late-derivation ones.
When asked about their beliefs regarding the primary benefit/s of PC for incurable cancer patients, 162 (33%) answered that PC addressed end-of-life, 156 (32%) that it improved the QoL of the patient and family, 122 (25%) that it improved patients’ symptom control, and 10 (2%) that it also addressed the psychological, social, and spiritual aspects. Thirty-nine (8%) said they did not have enough experience to determine the benefits of PC. Those oncologists with less experience (graduated ≤ 10 years ago) pointed out the improvement in QoL (65%) or were not able to determine the benefits (35%). Those with more experience (graduated > 30 years ago) prioritized end-of-life care (62%), and to a lesser extent, the improvement in QoL (19%) and symptom control (19%).
Finally, oncologists were asked which of the WHO statements about the scopes and benefits of PC for people with cancer25 they considered the most important. The most referred was “it provides relief from pain and other distressing symptoms” (43%). The least selected were “it is applicable early in the course of illness, in conjunction with other therapies that are intended to prolong life” (4%), “it integrates the psychological and spiritual aspects of patient care” (2%), and “it offers a support system to help the family cope during the patient´s illness and in their own bereavement” (N = 5; 1%).
In the MCA analysis, a frequent referral was associ ated with having received specific training in PC, referring the patient early or at the onset of symptoms, working in association with a PC team, in a multidisciplinary man ner, and highlighting the usefulness of PC for improving QoL. Non-referral was associated with not having enough experience with PC and not being able to determine the benefits of PC (Fig. 2a). Also, there was an association between exceptional referral, late-derivation criteria, and the oncologist´s younger or older age (Fig. 2b).

Fig. 2 Multiple correspondence analysis (MCA) showing spatial association among the referral frequency and the oncologists’ characteristics, attitudes, and opinions. A: Projection on the first and second factors. “Usually”: frequent referral, “Yes-PC”: the oncologist had specific training in PC, “Early”: early referral of the patient to PC, “Onset”: referral to PC at the onset of the symptoms, “f_a”: the oncologist worked in association with a PC team, “c_d”: the oncologist worked in a multidisciplinary manner, “QoL”: the oncologist highlighted the usefulness of PC for improving QoL, “No-experience”: the oncologist did not have enough experience about PC, “Not-determine”: the oncologist was not able to determine the benefits of PC. B: Pro jection on the third factor. “Exceptionally”: exceptional referral to PC, “Terminal” and “End-of-life”: the oncologist stated that the proper moment for referral was terminal disease or end of life, respectively, “30-34”: younger age, “>=65”: older age.
Oncologists who had specific training in PC (93% vs. 43%, P = 0.0007), those who stated that they were well informed about PC goals (96 vs. 41%, P = 0.0001), those who had an accessible PC service (60% vs. 8%, P = 0.0003), and those who had selected early-referral criteria (76% vs. 33%, P = 0.0001), were more likely to frequently refer their patients to PC. Oncologists who had more than 30 years from graduation (22% vs. 59%, P = 0.0015) were more likely to exceptionally or never refer their patients to PC. In multivariate analysis, factors positively associated with frequent referral were having an accessible PC service (OR = 2.944, CI = 1.250-6.935, P = 0.002) and being well informed about PC goals (OR = 6.331, CI = 4.022-17.939, P = 0.008), while having ≤ 10 years (OR = 0.117, CI = 0.047-0.290, P = 0.012) or > 30 years from graduation (OR = 0.111, CI = 0.020-0.621, P = 0.001) were associated with exceptional or no referral.
Discussion
This study aimed to examine the referral practices of on cologists to specialized PC in Argentina and to identify the characteristics and beliefs associated with the frequency of referral. Most oncologists surveyed considered that they were at least moderately informed about the scopes and principles of PC (83%) and expressed to have some level of accessible PC team/service in their practice (71%). Yet, more than half of them did not routinely work in collaboration with PC (53%) and exceptionally or never referred their patients (55%). The most frequent reasons for exceptional or non-referral were the oncologists’ mis trust about the necessity and advantages of PC inclusion and their perception that they could manage the patient´s requirement. Most of the criteria used for referral (proxim ity to death, uncontrolled symptoms, absence of curative treatment, poor functional status) suggest a late integra tion of PC. Moreover, while a considerable proportion of respondents thought that addressing end-of-life was the key benefit of PC for cancer patients (33%), only 4% remarked on the opportunity of its early inclusion in the course of cancer.
Studies from high-income countries, where palliative medicine is notably more developed than in Argentina, have similarly shown the lack of referral association with the oncologists’ lack of belief about the need for PC and their perception of self-efficacy. Also, they have shown the predominance of late referral with the prioritization of uncontrolled physical symptoms and terminal disease. Oncologists in Belgium pointed out “PC was not or not sufficiently meaningful for the patient” as the second most prevalent reason for not using PC services20. A survey in Australia found that the usual reasons for non-referral were the physicians’ confidence in their ability to manage patients’ symptoms and their belief that they could provide as good care as PC services17. A survey of oncologists in Canada found that over 80% of respondents referred their patients when survival prognosis was six months or less, and mainly due to the need for symptom control15. This suggests that widespread factors accounting for poor access to PC for patients with incurable cancer would be broadly related to preconceptions of the treating physi cians rather than the scarcity of PC resources. However, it should be noted that oncologists in Argentina do not receive training in PC, so their skills to manage PC needs are probably very limited. Similar to previous studies where psychosocial issues rarely triggered referral to PC17, we found that psychological and social wellbeing consid erations were non-prevalent reasons for referral. Only 1%-3% of oncologists stated an impact of PC upon the psychological, social, and spiritual fields, or upon family coping and grief. A former study in Argentina also showed poor detection of patients’ psychological morbidities by non-PC specialists. It evaluated differences between why oncologists demanded a PC consultation and the needs detected by the multi-disciplinary PC team at the time of the patient evaluation. Whereas consultations were pre dominantly due to uncontrolled symptoms and decline of the functional status, the PC team identified the need for intervention in the psychological, decision-making, com munication, and care planning areas22.
Potential associations between oncologists’ character istics, knowledge, and opinions about PC and the referral frequency were explored. As expected, the presence of available PC services and their level of information about PC were associated with a positive attitude towards refer ral. Surprisingly, an association was found with the age of the oncologist, being recent graduates and more senior practitioners more reluctant to refer their patients. One likely interpretation is that young doctors focus more on disease treatment and cure, with less attention paid to the patient´s comfort and symptom relief. On the other hand, senior oncologists, most of whom expressed that the most significant benefit of PC was providing end-of-life care, could remain attached to the old paradigm where PC was limited to people in terminal stages of the disease.
In the last decade, guidelines were established to over come the main barriers to access to PC for people with cancer. Among them, structural and procedural indicators for PC integration13,26, criteria for timely transfer of care27- 30, definitions of the appropriate time of PC contact13,29, and the notion of complexity for cancer patients31 were estab lished. Models were also designed to promote the inclu sion of quality PC in cancer care programs in resource-constrained settings32- 34. In developing countries in Latin America, an unacceptably small number of patients with cancer who need PC can currently access it9,10,23,35. This study is the first to provide local research-based evidence on human and health system-related factors possibly ac counting for this reality in Argentina. Insufficient availability of PC specialists in the place of practice does not seem to be a major obstacle. Results showed the lack of conviction of oncologists about the usefulness of incorporating PC into the care of their patients, the predominance of late referral criteria, and a worrying tendency not to consider the psychosocial needs of seriously ill people. Many other countries probably share these results in Latin America. A limitation of this study is the relatively low response rate, which represents approximately 60% of all oncologists practicing in Argentina. Although it is comparable to previ ous studies interviewing oncologists16,17,20, in this case it may be because doctors do not have enough resources and time available for research. In future studies, it would be interesting to follow up on referrals to explore whether the referral to PC is the end of the oncologist’s relationship with the patient, as well as to explore whether there are differences in criteria between public and private health care systems.
In conclusion, our study revealed deficiencies in the PC referral practices in Argentina. Most medical oncologists don´t refer their patients to PC even when PC services are largely accessible. The main reasons are oncolo gists’ belief that PC is not meaningful enough and their perceived self-sufficiency. Most of them use late-referral criteria and only a few consider the impact of PC on psy chological issues. Younger and older age are associated with exceptional or non-referral. More research is needed to understand ways to improve early access to PC for cancer patients and their families.