KEY POINTS
Current knowledge
• Right ventricular longitudinal longitudinal strain is fre quently used as a measure of right ventricular systolic function. Abnormal right ventricular (RV) strain values are associated with poor prognosis in patients with pulmo nary hypertension; however, the measure is not always easy to obtain in patients with poor apical acoustic window.
Contribution of the article to current knowledge
• Our study shows that subcostal right ventricular free wall strain can be reliably measured, with good agreement with traditional apical RV strain. It is a feasible and ac curate alternative to conventional right ventricular free wall strain from the apical view in patients with pulmonary hypertension and poor acoustic apical window.
Right ventricular (RV) systolic dysfunction is a strong predictor of mortality in patients with PH1,2. Several func tional parameters have been derived from two-dimension al RV assessment, but all have inherent strengths and weaknesses3. In patients with PH, with conditions such as chronic obstructive pulmonary disease, apical acoustic window are often suboptimal.
Speckle-tracking echocardiography (STE) allows to quantify RV systolic function without geometric assump tions4-6. RV longitudinal strain (RVLS) measurements can be obtained from both the apical and subcostal views; however we don´t know whether these two approaches are truly comparable. Hence, the aim of this study was to compare Right Ventricular Longitudinal Peak Systolic Strains (RV LPSS) obtained from both echocardiographic views.
Material and methods
This cross-sectional study analyzed 22 adult outpatients (≥18 years old), 81% female, mean age 49.9 ± 17.3 years, with a diagnosis of PH. According to the guidelines published by the European Society of Cardiology in 20157, PH was defined as a mean pulmonary artery pressure ≥ 25 mmHg in the right heart catheterization. The population was followed at Dr. Cosme Argerich Hospital from January 2016 to January 2020, and they were compared to a control group of 22 age- and sex-matched healthy subjects.
The control group was recruited by invitation from hos pital staff (mean age 49 ± 15 years) without any history of cardiovascular disease and normal clinical examination, chest X-ray, electrocardiogram, and two-dimensional echo cardiography.
The Research Ethics Committee of the Hospital Dr. Cosme Argerich approved this study.
All patients involved in this study provided written informed consent authorizing the use and disclosure of their protected health information.
According to the current clinical classification of pulmonary hypertension (PH) into five groups, based upon etiology and mechanism7-8, the most frequent causes of PH (Table 1) was included in Group I (Pulmonary Arterial Hypertension): Eisen mengers’s disease due to Congenital heart disease: 36.4%, Idiopathic: 18.2%, Connective tissue disease: 9.1%, HIV: 4.5%, Hereditary: 4.5%, portopulmonary hypertension: 4.5%), Group II (PH due to left side heart disease): 13.6%, Group III (PH due to chronic lung disease): COPD: 4.5% and Group V (PH due to multifactorial mechanism): Gaucher disease: 4.5%. None patient was in Group IV (PH due to chronic pulmonary thromboembolism).
All patients had been treated with PH-specific drugs (Ta ble 1), including intravenous/inhaled prostacyclin analogues (Iloprost: one patient intravenous and two patients inhaled, treprostinil: two patients), endothelin receptor antagonists (ERA: Bosentán: three patients, Ambrisentán: three patients), and phosphodiesterase 5-inhibitors (PDE-5: Sildenafil: eleven patients), either as a single drug or combined in concordance with current guidelines recommendations7.
All patients at the time of the study had to have a diagnosis of PH confirmed by right heart catheterization and defined as mean pulmonary artery pressure ≥ 25 mmHg.
Patients were excluded from the study for any of the follow ing: age less than 18 years, irregular heart rhythm, prolonged QRS duration, aortic or mitral regurgitation more significant than mild, coronary heart disease, RV outflow tract obstruction, RV pacing and RV myocardial infarction.
Patients with these comorbidities were excluded to avoid any possible influence on the results of RV strain measurement.
All two-dimensional echocardiogram was performed using a commercially available Vivid 7 ultrasound system (General Electric Medical Systems, Milwaukee, WI) with a phased ar ray 3.5 MHz transducer. Three cardiac cycles were recorded and saved in cine loop format in the machine’s hard drive to be analyzed offline later by two independent observers. For measuring left and right ventricular parameter the following views were used: left parasternal (long- and short axis), apical 4-chamber views, including RV focused apical view according to the guidelines of the American Society of Echocardiogra phy (ASE)8, with the patient in left decubitus position. The subcostal four-chamber view were obtained with the patient in the supine position.
The following parameters were measured using M-mode and two-dimensional echocardiography: left ventricular (LV) diameter and end-diastolic volume, LV diameter, and end-systolic volume, LV ejection fraction, right ventricular (RV) basal diameter, RV dimensions (end-systolic and end-diastolic areas), RV fractional area change (RV FAC), tricuspid annular plane systolic excursion (TAPSE), Pulmonary artery systolic pressure (PASP) and mean right atrial pressure3. In addition, the LV ejection fraction (EF) was estimated using Simpson’s method, and LV dysfunction was defined as a value below 55%.
All patients were examined using second-harmonic, adjust ing the sector size for adequate frame rate and optimal RV border visualization.
TAPSE was measured in the apical four-chamber view by aligning the M-mode cursor through the lateral tricuspid annu lus, calculating the total excursion of the tricuspid annulus from its highest position until its lowest descent during ventricular systole. A TAPSE < 16 mm indicates RV systolic dysfunction8.
RV FAC was calculated according to the ASE formula3 as: (RV end-diastolic area -RV end systolic area)/RV end-diastolic area) x 100. RV FAC < 35% indicates RV systolic dysfunction.
Pulmonary artery systolic pressure (PASP) was calculated from the tricuspid regurgitation jet’s peak velocity, using the modified Bernoulli equation plus right atrial pressure estimated by the inferior vena cava size and collapsibility3.
Standard, a commercially available software (EchoPac PC, Version 108.1.5; GE Medical System), was used to obtain two-dimensional STE, by a single experienced reader (OP), and the analysis was confirmed by a separate experienced reader (TFC). We use STE to evaluate the RVLS.
RVLS is defined as the percentage of shortening of the region of interest (ROI) relative to the original length and is conventionally presented as a negative value. The only images with a frame rate between 40 to 80 frames/sec were selected for reliable analysis.
The endocardial border of the RV free wall was manually traced out at an end-systolic, and the software displayed automatically an ROI, including the myocardial wall. This ROI can be manually adjusted to the thickness of the RV myocardium to ensure adequate tracking, and segments were excluded because of suboptimal visualization or if unable to be satisfactorily tracked.
For the lateral RV strain assessment, the images were ob tained from the apical 4-chamber RV dedicated view focusing on the lateral wall8 and from the four-chamber subcostal view. The frame rate used in 4-chamber RV dedicated view focusing on the free wall was higher (probably narrower interrogation sector) vs. subcostal (wider attempting to include apex to base RV, resulting in lower frame rate).
Peak systolic strain was measured in the basal, midven tricular, and apical segments of the RV free wall (obtained from the apical four-chamber and subcostal view), and averaged to obtain RVLS (Figs. 1 and 2).
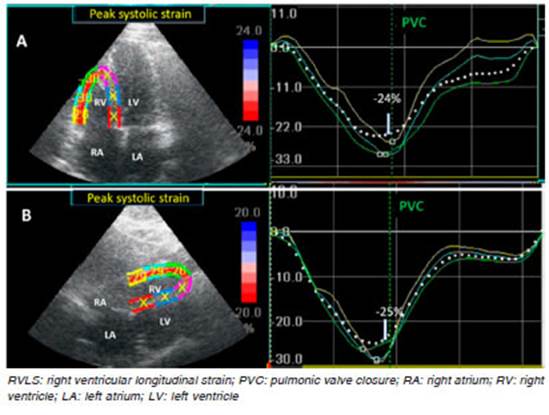
Fig. 1 RVLS free wall assessment by speckle tracking echocardiography in a normal subject. A: RVLS in the Apical four-chamber view (-24%). B: RVLS in the subcostal view (-25%). Note the good correlation between both views.
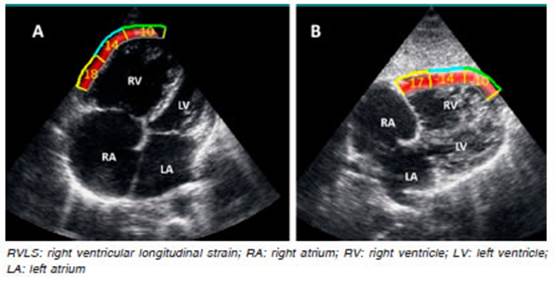
Fig. 2 RVLS free wall obtained from a patient with pulmonary hypertension, showing the impairment of myocardial strain: A: RVLS in the Apical four-chamber view: -14%. B: RVLS in the subcostal view: -13.66. Note the good correlation between both views.
We analyze the RV free wall separately, excluding the ventricular septum, and synchronize the analysis with the time of the pulmonary valve’s opening and closure (Fig. 1 and 3).

Fig. 3 Assessment of RVLS free wall. A: Normal subject (-24%). B: Patient with pulmonary hy pertension (-13.3%)
RVLS is depicted with a negative curve and a peak close to the pulmonary closure. These RVLS curves represent the maximum longitudinal myocardial shortening during contrac tion in the three segments of the lateral from 4-chamber and subcostal views.
Segments for which the automated acquisition of strain failed were corrected manually. Segments for which the ac quisition of strain failed again were excluded.
In accordance with Muraru et al9 the predefined cutoff for RV systolic dysfunction was a RVLS less than −23% (−22.5% for men and −23.3% for women)
Quantitative data with a normal distribution were expressed as mean ± standard deviation, and data with a non-Gaussian distribution were expressed as a median and interquartile interval.
To compare quantitative variables with a normal distribu tion, Student’s t-test for paired data was used; for variables with non-normal distribution, either Wilcoxon or Signed Rank’s test were used. All p values < 0.05 were considered to be statistically significant.
Categorical variables were described as number and percent; continuous variables were expressed as mean and standard deviation (SD) or median and interquartile interval (IQI) according to their distribution. To establish the distribution of quantitative variables, we used asym metry analysis (skewness) and Kurtosis, and the Shapiro- Wilk test.
Comparison of continuous variables between groups was performed with the t-test, or non-parametric tests (Wilcoxon or Signed Rank test) according to their distribution.
The intraclass correlation coefficient (ICC) was used to determine inter- and intraobserver reproducibility for RVLS from data for ten randomly selected patients using an identical cine loop for each view.
In patients with PH, Pearson’correlation was performed to evaluate the degree of agreement between RV LPSS mea surements in the apical and subcostal views.
The methods used to evaluate the agreement between the two variables were simple linear regression and the Bland & Altman concordance test.
A p-value < 0.05 was considered significant. All analyses were performed with Epi-info 2000 v. 3.5.1 and Statistics 7.0 software.
Results
In the present study, four patients with poor acoustic window were excluded because of inadequate tracking of two or more segments of the RV. These patients could not be measured RV strain with the RV focused view but could be evaluated with the subcostal view.
A total of 22 patients with a diagnosis of PH had ad equate apical and subcostal views, and these patients were included and analyzed.
The clinical and demographic characteristics data of the 22 patients diagnosis with PH and 22 control subjects are described in Table 1. This population’s demographic is similar in age and sex. Body mass index, heart rate, systolic blood pressure, and diastolic blood pressure were similar in both groups. Two patients (9%) with PH were in NYHA functional class I, six patients (27.3%) in class II, 11 patients (50%) in class III, and three patients (13.7%) in class IV.
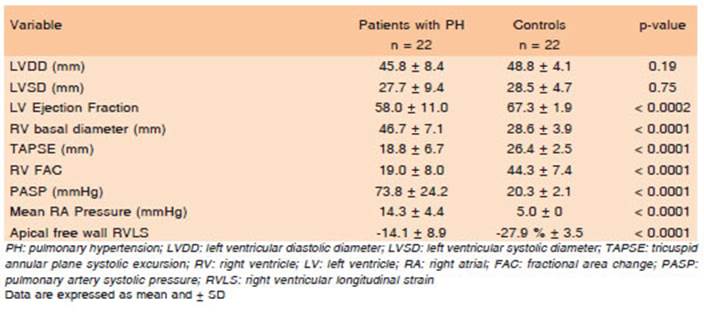
Table 2 summarizes the echocardiographic variables of both groups. There were no differences in LV dimensions between both groups. As expected, LV ejection fraction was significantly lower in patients with PH compared with the control group (p < 0.0002).
Patients with PH exhibited anatomic and functional impairment of the RV echocardiographic parameters. All echocardiographic-derived parameters (RV basal diam eter, TAPSE, and RV FAC) were significantly different between patients with PH and controls, consistent with RV dilatation and RV systolic dysfunction.
When patients with PH were compared to normal subjects, they exhibited, RV basal dilation (46.7 ± 7.1 mm vs. 28.6 ± 3.9 mm, p < 0.0001), decreased TAPSE (18.8 ± 6.7 mm vs. 26.4 ± 2.5 mm, p < 0.0001), decreased RV fractional area change (19.0 ± 8.0% vs. 44.3 ± 7.4%, p < 0.0001), increased pulmonary artery systolic pressure (73.8 ± 24.2 mmHg vs. 20.3 ± 2.1 mmHg, p < 0.006), and increased mean right atrial pressure (14.3 ± 4.4 mmHg vs. 5.0 ± 0 mmHg, p < 0.0001).
Global RVLS of the right ventricle’s free wall was de creased in patients with PH: -14.1% ± 8.9% vs. -27.9% ± 3.5% in control subjects (p < 0.0001).
Global RVLS measured in the RV free wall from the apical four-chamber view (Table 3) was -15% (-19% to -10%) vs. -14.5% (-18% to -11%) when measured from the subcostal view (p=0.99). Segment by segment analysis did not show significant differences either: basal four-chamber was -16.5% (-21% to -11%) vs. -15.5% (-20% to -11%) from the subcostal view (p = 0.99), mid four-chamber was -16.5% (-21% to -12%) vs. 16.5% (-20% to -12%) (p = 0.59), apical four-chamber view was -12% (-18% to -8%) vs. -13.5% (-19% to -10%) from the subcostal view (p = 0.93).

Table 3 Measurements of the right ventricle longitudinal strain from subcostal view and four-chamber view in patients with pulmonary hypertension
This study aimed to compare RVLS obtained from api cal and subcostal views in patients with PH.
The evaluation of Figure 1 was made on a normal sub ject, with a good correlation in of between RVLS obtained from apical and subcostal views. In controls subjets, we only perform RVLS from the 4-chamber view, but we do not use the subcostal view in this population.
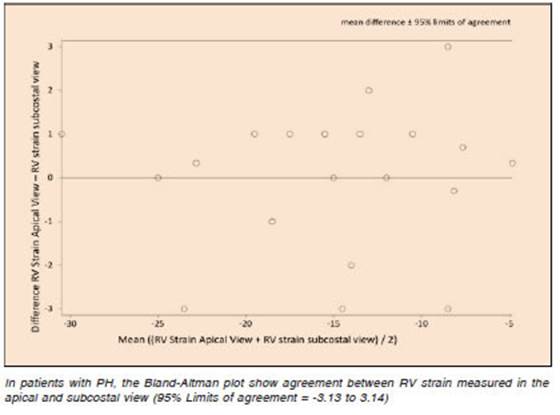
In patients with PH, simple linear regression (Fig. 4) and Bland & Altman concordance test (Fig. 5), showed good correlation between apical and subcostal views measurements of RVLS (r = 0.969; p < 0.0001, and 95% Limits of agreement = -3.13 to 3.14 respectively).
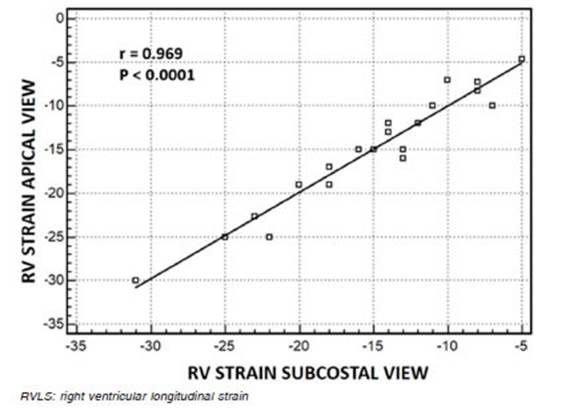
Fig. 4 Linear regression plot between RVLS measured in the apical and subcostal view. r = correlation coefficient by Pearson
The intraclass correlation coefficient (ICC) for in traobserver reproducibility for RVLS measured in the apical four-chamber view and subcostal view were 0.90 (95% CI, 0.75-0.95), and 0.95 (95% CI, 0.90-0.97), respectively. The corresponding ICC for interobserver reproducibility was 0.94 (95% CI 0.87-0.97) for the api cal four-chamber view and 0.88 (95% CI, 0.73-0.95) for the subcostal view.
Discussion
In patients with PH, the present study has shown an ex cellent correlation between the apical four-chamber view and the subcostal view for the measurement of global and regional RV LPSS (r = 0.969, p < 0.0001). The crucial find ing in this study is that the measurement of RVLS in the subcostal view allows to assess RV function in patients with poor apical echocardiographic window.
The RV systolic dysfunction is a strong predictor of mortality in PH. However, the assessment of RV systolic function, using two-dimensional echocardiography, entails several disadvantages.
While TAPSE is a robust and highly reproducible mea sure of RV systolic function, it is obtained only in specific views of the RV; additionally, it is angle-dependent and may be overestimated in patients with PH and apical clockwise rotation. TAPSE assumes that the longitudinal motion of the basal segment of the RV free wall represents the function of a complex RV geometry.
Other parameters are less reproducible than TAPSE, such as the RV FAC calculated from a single apical four-chamber view, which is obtained by tracing the RV endocardium both in systole and diastole from the annulus. Care must be taken to trace the free wall, excluding the trabeculations3. The RV FAC is dependent on the imaging plane, thus causing considerable inter and intraobserver variability in patients with suboptimal endocardial defini tion and limited by its assumptions regarding complex RV geometry. Both methods are reliable only when measured in the apical four-chamber view, and when such view is not available, an alternative measurement is required.
Recently, STE has been recommended as a superior method for the assessment of RV function, given its advantage of being angle-independent. Moreover, it can detect RV dysfunction more accurately and sensitively than TAPSE or RV FAC6,10.
Other authors have demonstrated that STE strain is simpler, more accurate, and faster than longitudinal strain assessed by cardiac magnetic resonance (CMR). The study concludes that STE is a good alternative to CMR, with a moderate degree of agreement11.
Inclusion of the interventricular septum is another issue12,13. Several authors showed that RVLS free wall correlated better than global RVLS with RV ejec tion fraction measured by CMR. In a recent recom mendation published by the European Association of Cardiovascular Imaging (EACVI)/American Society of Echocardiography (ASE)/Industry Task Force to standardize deformation imaging, using RVLS free wall is the default method for measurement of RV strain14. However, this recommendation stated that including the interventricular septum in the analysis was an option for the users. In our study, we measured RVLS excluding interventricular septum6. The RVLS free wall values are more frequently negative than RVLS values. Anatomically, the RV and LV share an interventricular septum. The RV free wall is composed of predominantly the transverse fibers, and the LV is encircled by oblique fibers. The interventricular septum consists primarily of oblique fibers that extend into the RV outflow tract. Consequently, the LV actively contributes to about 80% of the flow and to 2/3 of the pressure generated by the RV during systole. More over, measuring strain only in the the RV free wall is difficult for some algorithms because of the strict differentiation required between RV free wall and the interventricular septum.
In previous studies evaluating RV function in patients with PH, RVLS was measured from the apical four-chamber view, and patients with poor apical acoustic windows were excluded. Many of these patients had PH secondary to chronic obstructive pulmonary disease and were therefore underrepresented in those studies. Feasibility of measuring RVLS in the apical four-chamber view has been reported to range between 75% and 93%7. Alternatively, measuring RVLS from the subcostal view may overcome this limitation.
An advantage of using STE to calculate RV systolic deformation is the lack of angle dependence, since speckles are traced in two directions along the myo cardial wall, and not in the direction of the ultrasound beam6,15. The algorithm used by EchoPAC PC, Ver sion 203, does not take into account if the region of interest is parallel (4-chamber view) or perpendicular (subcostal view) to the transducer, so the workstation always measures the longitudinal shortening of the RV myocardial fibers from RV base to RV apex, regardless of the insonation angle.
Although prior studies have analyzed multiple RV views, they did not report results obtained from the sub costal approach16. A major strength of RVLS is its ability to assess the RV function without the limitations of other two-dimensional RV function parameters.
In agreement with Haeck et al.17, we demonstrated that RV strain obtained from the subcostal and apical four-chamber views were similar, but our population was different from theirs, because they studied patients with suspected pulmonary hypertension, excluded patients with congenital heart disease and did not perform right heart catheterization. In our study, we included patients with confirmed PH, defined as a mean pulmonary arterial pressure ≥ 25 mmHg assessed by right heart catheteriza tion, and the most frequent etiology of PH was congenital heart disease (36.4%).
In our study, the measurement of subcostal RVLS proved to be feasible and accurate, showing good correla tion and agreement with the standard apical four-chamber view. In patients with PH, with a dilated RV and poor RV function, RVLS showed a good correlation between both echocardiographic views. Therefore, RVLS obtained from the subcostal view could be an alternative to conventional RV strain obtained from the apical view in patients with pulmonary hypertension and poor echocardiographic apical window.
There are several limitations to this study. First, it was performed at a single center, therefore, we cannot reach definitive conclusions but can only formulate a hypothesis that will require confirmation by future multicenter trials.
Also, the study included a small number of patients with a PH of various etiologies, who were assessed in a non-randomized manner. Hence, a larger study, includ ing more patients with a single etiology of PH, would be required to validate our findings.
We compared RVLS from the apical and subcostal views in patients with PH, but we do not usually perform RVLS from the subcostal view in normal subjects. A control group was included in our study only to assess whether there were differences between the RVLS between both views.
The echocardiographic speckle-tracking technique is dependent on good image quality. However, this study has demonstrated that the technique has excellent in terobserver and intraobserver correlations.
In conclusion, subcostal right ventricular free wall strain can be reliably measured, and has shown good agreement with traditional apical RV strain. Hence, it represents a feasible and accurate alternative to apical right ventricular strain in patients with pulmonary hypertension and a poor apical acoustic window.