Coronary artery anomalies (CAA), an entity of growing presence, correspond to a varied group of cardiovascular congenital disorders, involving anatomical defects that can manifest in isolation or associated with other heart diseases. According to Angelini1, CAA can be defined as those coronary arteries with abnormal anatomical features observed in less than 1% of the population.
Among these defects and variations, one subgroup has a particular interest because of its clinical repercussion: Anomalous origination of a coronary artery from the op posite sinus (AOCAOS)2. Their clinical impact ranges from asymptomatic patients to sudden cardiac death (SCD), especially in young athletes2,3. There are no strict recom mendations validated by evidence or guidelines from the main scientific societies for their diagnosis, follow-up, or even for their treatment, which implies a medical challenge and requires and individualized management4,5.
The case of a patient diagnosed with anomalous origin of coronary arteries is presented below.
Clinical case
We describe the case of a 63-years-old man, with cardiovas cular risk factors (arterial hypertension, non-insulin-requiring type II diabetes involving polyneuropathy and retinopathy, overweighted - BMI 29 kg/m2) who consulted to our medical center with 1-week history of progressive dyspnea on exer tion, with clinical signs of heart failure. During anamnesis, the patient mentions the case of a twin brother who died of unknown causes, aged two months. Physical examination revealed jugular venous engorgement without inspiratory col lapse, crackles in both lung bases, and the presence of a third heart sound on cardiac auscultation. The electrocardiogram was in sinus rhythm, with a heart rate of 75 bpm, without major particularities. The chest X-ray revealed an increased cardio thoracic index, with a pulmonary hypertension pattern. These findings, together with an elevated NT-proBNP level (2000 pg/ml; normal value <150 pg/ml), confirmed the diagnosis of heart failure. The rest of the laboratory tests showed diabetes under regular control, with 148 mg/dL fasting glycemia and 7.5% glycosylated hemoglobin, without any other remarkable alterations.
Initial treatment with diuretics was established (Furosemide 20 mg IV q8hr), and the patient was subsequently studied with a Doppler echocardiogram that showed a dilated car diomyopathy with severe deterioration of the left ventricle systolic function (biatrial dilatation, severe dilatation of the left ventricle with an ejection fraction of 26%, pattern of global hypokinesia, and moderate mitral regurgitation with central jet). After treatment with diuretics and clinical improvements of the symptoms, a coronary angiography was performed in which an abnormal origin of the left main coronary artery (LMCA) from the right coronary sinus (RCS) was evidenced (Fig. 1A), with a proximal lesion nearing 50%. The left anterior descending and circumflex arteries both had moderate-mild lesions (Fig. 1B), while the right coronary artery was occluded in its posterior ventricular branch and received little collateral circulation. The rest of the vasculature of thin caliber showed diffuse lesions, none angiographically significant. With the finding of the LMCA anomalous origin, a coronary com puted tomography angiography was made to evaluate the anatomy and confirmed the presence of a common trunk originated in RCS (Fig. 2A) with an intramyocardial path at the level of the interventricular septum with moderate extrinsic compression (Fig. 2B and 2C). The right coronary artery originated from the common trunk, with a normal path and mild diffuse lesions.
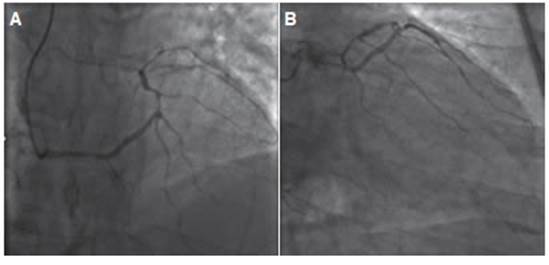
Fig. 1 Cardiac catheterization showing diffuse disease and fine-caliber vessels. A: It can be observed an abnormal origin of the left coronary artery from the right coronary sinus, with a moderate lesion in the proximal segment. B: Moderate-mild lesions can be seen in both left anterior descending artery and circumflex artery

Fig. 2 Coronary computed tomography angiography with tridimensional reconstruction showing: A) Left main coronary artery originating from right coronary sinus, with an intramyocardial path at the interventricular septum (red arrow), B) moderate extrinsic compression of the left main coronary artery. Circumflex artery shows a moderate/severe lesion with a calcified aspect. C) 3 -reconstruction showing the origin of the intramyocardial path of the left main coronary artery from the right coronary sinus (blue arrow)
To determine the degree of functional ischemia, a cardiac catheterization with fractional flow reserve was performed, resulting in 0.75 (>0.80 is a normal physiological value), which was considered significant and was followed by an angioplasty with drug-eluting (Everolimus) stent implantation to the target lesion. No complications were associate with the procedure. During hospitalization, the patient started guideline-directed medical therapy (angiotensin receptor/neprilysin inhibitors sa cubitril/valsartan; beta-blockers; sodium-glucose cotransporter 2 inhibitor and mineralocorticoid receptor antagonists) for heart failure with reduce ejection fraction with favorable tolerance.
The patient evolved favorably, with no recurrence of heart failure, asymptomatic at the time of discharge from the medi cal center, to continue outpatient follow-up and adjustment of medical treatment for heart failure. He remained asymp tomatic during clinical evaluation at 1-month and 6 months, with no presence of ischemia on a single-photon emission tomography control.
Discussion
The incidence of the CAA is quite variable, ranging between 0.1 and 5,7%2. The causes of this congenital anomaly are still controversial, yet several research show that part of its origin is due to alterations in com plex molecular and cellular mechanisms involved during coronary embryonic development6. The latest simplify classification proposed by a group of experts divides these anomalies into three groups: 1) origin and path anomalies (absent LMCA, ectopic location of the coronary sinus, and anomalous origin of coronary arteries in the op posite sinus - AOCAOS), 2) intrinsic coronary anomalies (stenosis, atresia, aneurysms, myocardial bridges), and 3) termination abnormalities (coronary fistulas, inappropriate branching)1,7. Within the group of AOCAOS, they present with a incidence that ranges between 0.28-1.74% , and the most frequent variation is the right coronary artery originating from the left coronary sinus, and secondly, the origin of the circumflex artery from the RCS.2,3,7,8. The clinical manifestation is highly variable: most patients do not develop any symptoms throughout their lives, whereas in others the most frequent clinical first manifestation (7-45%) could be syncope, dyspnea, acute myocardial infarction, chest pain on exertion, or even SCD1,7-9.
The presence of myocardial ischemia in these patients, considered the main mechanism of high-risk events, can be pathophysiologically explained through different paths that alter tissue perfusion (acute coronary angulation, extrinsic compression by intramural or interarterial path, vasospasm, or endothelial injury secondary to the turbu lent flow development)7,8. There is no strict evidence of an association between the presence of CAA - and AOCAOS - and the developement of atherosclerotic disease1,2,7. The presence of CAA in patients with symptoms related to myocardial ischemia does not necessary implies a linked between these two entities, particularly in older patients with cardiovascular risk factors and absence of the high-risk variants of CAA, where atherosclerotic disease should be discarded9. In a Chilean registry10 with 10 000 cardiac catheterizations performed in adults, the authors proved that patients with abnormal coronary arteries showed the same or lower levels of atherosclerosis than patients without an abnormal coronary origin.
The most feared manifestation is SCD3, especially between the second and third decade of life1,2. After hypertrophic cardiomyopathy, this entity ranks second as a cause of SCD in young patients, reaching up to 19% of sudden deaths in young athletes1-3. Among CAA, the AOCAOS with an interarterial course (e.g., between aorta and pulmonary arteries), ostial tightness, acute takeoff angle or intramural path, as well as the coronary arteries emerging from the pulmonary artery, are those involving a greater risk of SCD7-10. In certain cohorts, among the different anatomically variants of AOCAOS, the left coronary artery originating from the right sinus is consistently associated to SCD in 59% of cases, 81% of which occur after episodes of intense exercise, with no previous symptomatic manifestation8.
The diagnosis requires a high level of suspicion, but very frequently, it is made as a mere incidental finding dur ing the evaluation of ischemic heart disease. Many times, the ischemia-inducing functional tests are the first step to continue the study in greater depth as it is recommended by the guidelines of the European Society of Cardiology4, yet the evidence demonstrates that stress-testing are not likely to identify patients at high risk of developing ischemia due to CAA. A negative result does not rule out either the diagnosis or the severity of the prognosis3. Current guide lines recommend single-photon emission tomography as the first choice to detect ischemia in patients with CAA11.
The echocardiography has a role for detecting an ab normality in the coronary arteries in children population7. In adults, its precision to discriminate the type of abnor mality, the coronary ostia and the course of the vessels is low, being extremely operator-dependent12. Cardiac catheterization sensitivity and specificity are high, but lacks visualization of other structures as well as its invasiveness and lack of resolution1-4. However, its utility has been reconsidered, and its being studied, in certain scenarios due to the implementation of intravascular images7-10. Moreover, the association of cardiac catheterization with physiological evaluation and functional assessments, such as fractional flow reserve, is increasingly being used to determine coronary flow reserve in CAA and drive thera peutic choices13.
Nevertheless, the imaging study that offers greater spatial definition, and allows a clearer analysis of the relation of the anomalous coronary arteries with other vascular or muscular structures is the coronary com puted tomography angiography, currently considered the gold standard11,12. The cardiac magnetic resonance has emerged as an alternative for diagnosis of AOCAOS for not using iodinated intravenous contrast, but its high cost and lower precision place it on a secondary role12.
Regarding therapeutic approach, there is lack of evidence about the benefit of medical treatment. Beta-blockers have been proposed to prevent the onset of ischemia and arrhythmias, with a poor level of recom mendation, and limited only to the most benign varieties of AOCAOS4,5. Surgical or percutaneous treatments are aimed at correcting those variants with a higher risk of SCD. For AOCAOS with interarterial or intramural course (as well as hypoplasia cases, or variants in the charac teristics of the coronary orifice) associated to high-risk clinical manifestations such as aborted-SCD, evidence of myocardial ischemia, syncope or chest pain, the indica tion for invasive treatment becomes an unquestionable option4,5. Surgical treatment, using coronary artery bypass techniques, reimplantation of the coronary ostium, and unroofing methods with restoration of normal anatomy are the most recommended, and with the best results14. In experienced centers, mortality rates are comparable to those of conventional revascularization surgery, with favorable post-operative evolution, which can be explained due to the age of the patients who undergo surgery14. In patients older than 35 years, such as our patient, the risk of SCD is lower, but the risk of developing ischemia is not, so revascularization is usually chosen2-5. Percutaneous intervention has been successful in certain cases reported with symptomatic improvement, and a risk of 10% in-stent restenosis at 5 years, making it a suitable option in patients belonging to an older population, with evidence of ischemia, who should be revascularized15. Considering the scarce evidence of this pathology when selecting the best treatment and approach, the best strategy to address these cases will depend according to the individual, age, symptoms, the coronary anatomy, and the physiological alterations evaluated.
In conclusion, the diagnosis of the CAA, and particularly AOCAOS, requires a high level of suspicion, and its study implies a medical challenge. Imaging techniques are the most suitable studies for their visualization, being coronary computed tomography angiography the current gold stan dard. The knowledge of the pathology and its anatomical variants must be considered, due to the risk of SCD. In the absence of guidelines supported by strong scientific evidence, it is important to individualize each case in order to provide patient-tailored appropriate treatment in those with a greater risk of fatal complications.














