Oral tumors are a relatively common patholo gy that can present at different ages. Its clinical presentation is characterized by tumor mass, facial deformity and bone pain. In these cases, the differential diagnoses are multiple, from infectious diseases, malignant tumors such as lymphomas and soft tissue sarcomas. However, they occasionally may be the manifestation of advanced hyperparathyroidism1.
Primary hyperparathyroidism (PHPT) is cha racterized by elevated serum parathyroid hor mone (PTH) and calcium. PHPT is caused by a solitary or multiple parathyroid adenomas in 80- 85% of the cases2. In the last decades, given the advent of the routine measurement of serum calcium in periodic health examination, the classical manifestation of PHPT as nephrolithia sis and nephrocalcinosis or skeletal disease has nearly disappeared. Actually the PHPT is often diagnosed by mild symptoms of hypercalce mia or incidental finding of asymptomatic high serum calcium levels2.
The typical bone manifestation of PHPT is the osteitis fibrosa cystica. It is characterized clini cally by bone pain and radiographically by sub periosteal bone resorption, osteolysis of the dis tal clavicles, a “salt and pepper” appearance of the skull, bone cysts and brown tumors3. Brown tumors (BT) represent approximately 10% of all skeletal injuries caused by PHPT and typically affect ribs, clavicle, tibia, femur and pelvic girdle, being the jaw involvement of 0.1% to 4.5% of ca ses3,4. As BT are rare, they may be underdiagno sed or even be mistaken for malignant lesions5 and they are not included in the initial differen tial diagnosis of this manifestation of skeletal disease, especially when are present in atypical localizations.
Clinical case 1
A 44-year-old woman presented to the dentist with swelling over the central body of the jaw. She noticed the swelling 4 weeks earlier. The size of the mass had pro gressively increased, causing mobility of central incisor, canine and first premolar teeth and functional problems with chewing and speech. On initial intraorally exami nation an expansive, painful, hard, hyperpigmented and sessile lesion of 4 × 3 cm was noted (Fig. 1A). There was no cervical palpable lymphadenopathy. Her medical his tory revealed left nephrolithiasis diagnosed 1-year-ago. A maxillofacial computed tomography (CT) showed an osteolytic lesion (Fig. 1B). An incisional biopsy was done on the mandibular tumor and the result was reported as giant-cell tumor (Fig. 1C). 99mTc-Sestamibi bone scinti graphy showed no bone lesions except in the mandible. On the other hand, bone densitometry revealed low bone mass. The mass was removed before performing imaging of the neck. Serum biochemistry was compatible with PHPT (Table 1). Ultrasound (US) revealed a large solid le sion with a central cystic area on the right inferior parathyroid gland measuring 2.1 × 2.6 cm. 99mTc-Sestamibi scan of the parathyroid showed uptake at the inferior of the right thyroid lobe. The patient underwent right infe rior parathyroidectomy and histopathology of the lesion confirmed a parathyroid adenoma. The patient recovered without complications and normalized biochemical pa rameters (Table 1).
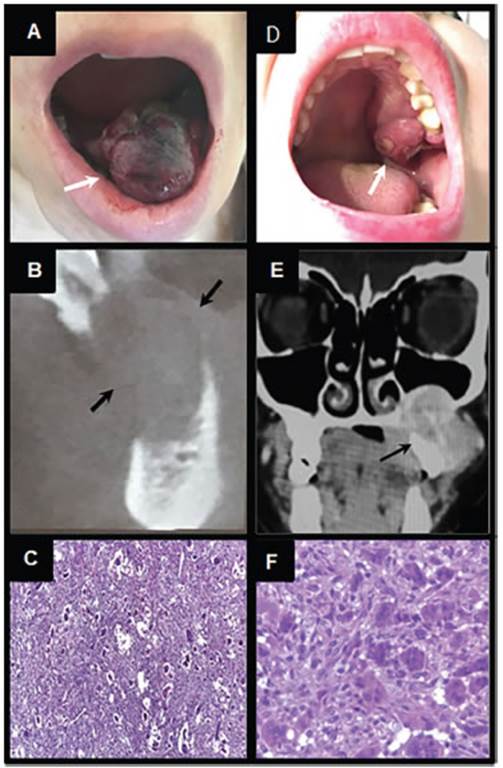
Figura 1 In intraoral photoghaphs white arrows show a solitary exophytic lesion arising from the mandible (A) and maxilla (D). CT scans show hypodense osteolytic lesions that infiltrate the jaw (B-E) as indicated by black arrows. Biopsy images of brown tumor: (C-F) staining shows a brown tumor with multinucleated giant cells in a hypervascular fibroblastic stroma (H&E; 100 x). (F) Numerous osteoclast-like multinucleated giant cells (H&E; 250 x)
Clinical case 2
A 23-year-old woman was referred to us by an otorhi nolaryngologist. She presented with a 3-month history of a painful mass in left maxilla bone. The size of the mass progressively increased. She complained about nocturnal episodes of gingival hemorrhage and bad breath. Her past medical history was unremarkable. Examination of oral cavity demonstrated a firm, non-fluctuant, ulcerated le sion of 2 cm arising from left maxilla (Fig. 1D). CT showed a well-defined osteolytic lesion of the left maxillary sinus and palatine bone (Fig. 1E). An incisional biopsy of the tumor resulted in a giant-cell tumor (Fig. 1F). Laboratory evaluation revealed that the patient had PHPT (Table 1). Calcitonin and prolactin were in normal range. Cervical US showed a large solid lesion with macrocalcifications on the right inferior parathyroid gland measuring 3.1 × 1.2 cm. 99mTc-Sestamibi scan of the parathyroid showed MIBI uptake at the inferior of the right thyroid lobe. Syste mic impact of hyperparathyroidism resulted in low bone mass, bilateral renal staghorn calculi and a 99mTc-ses tamibi bone scintigraphy, which showed hypermetabolic foci in the superior left maxilla, inferior right maxilla and skull. The patient underwent right inferior parathyroidec tomy and histopathology confirmed a parathyroid adeno ma. She recovered without complications and normali zed biochemical parameters (Table 1). Two weeks after surgery, she referred no pain on her oral lesion and a re duction of its size was evident. She was lost to follow up.
Both cases were solitary tumors with no evidence of palpable cervical lymphadenopathy.
Discussion
BT are slow-growing lesions that can be loca lly destructive resulting in significant bone pain and pathologic fractures6. The name BT refers to the brown appearance of the lesion as a conse quence of local hemorrhage produced by an im balance of osteoclastic and osteoblastic activity, causing high bone resorption with fibrous con nective tissue proliferation replacing the nor mal content of bone marrow and thinning the cortex6. It needs to be emphasized that BT are non-neoplastic lesions and represent a reparati ve cellular process.
The facial BT occur most frequently in the mandible whereas maxilla or both jaw bones are less commonly affected. The appearance of oral BT is more prevalent in the third decade of life and has a little female predominance7. As evi denced in our case series, BT generally appear as a hard and painful palpable swelling, with or without facial deformity7.
Typical radiological findings of BT are well-defined radiolucent lesions that do not affect the cortical layer and with no evidence of periosteal reaction or inflammatory signs8. On CT images, BT usually appear as a multiloculated lesion with “ground glass opacification”9. It is impor tant to remark that BT are frequently associated with other bone changes due to general bone compromise of PHPT such as demineralization or subperiosteal resorption, salt-and-pepper ra diographic appearance of skull bones10. In our patients, diffuse bone involvement was confir med by low bone mass in bone densitometry.
BT may be histologically indistinguishable from central giant cell granuloma and giant cell tumor11. Thus BT are only differentiated by a cli nical and biochemical context of PHPT as was evident in the cases described.
The first option in the management of the BT caused by PHPT is the parathyroidectomy12. Most bone lesions will regress with time after parathyroidectomy, therefore, surgical removal of the BT may not be necessary13. However, if the lesion continues to grow despite treatment, per sists for more than six months or is locally dis figuring, the surgical excision of the BT may be indicated14. The two cases presented illustrate these possible treatments. In case 1, surgical re moval of the mass was required due to the local symptoms she presented. On the other hand, in case 2 the parathyroidectomy resulted in impro vement of the size and symptoms of the BT.
In conclusion, PHPT is currently diagnosed more frequently by the coincident finding of as ymptomatic hypercalcemia in the laboratory. BT represent the terminal stage of bone remodeling processes in this disease. Although this type of clinical presentation has almost disappeared in the recent decades, these cases highlight the fact that BT should be considered in the diffe rential diagnosis of bone oral masses.















