Disc herniation is a frequent pathology that affects between 40 to 50 per 100 000 inhabitants. The exception to this is thoracic disc herniation (TDH) which affects 1 in 1 000 000 inhabitants. They usually affect the population between the third and fifth decade with equal distribution between genders. This pathology is relevant for the possibility of spinal cord compression, which transforms them into a surgical emer gency. Given its location and the risk of remove by a posterior approach, thoracic hernias are a major challenge for the surgeon. The surgical technique will be chosen based on the size, di rection of the hernia, the compromised levels and the experience of the surgeon1-3.
The objective is to report an atypical case with three levels of disc herniations in the thoracic spine with acute myelopathy treated by ante rior transthoracic approaches bilaterally with a lapse of 12 months between interventions
Clinical case
A 48-year-old female consulted the emergency room for 48 hrs. of epigastric abdominal pain radiating to the back, urinary retention, gait disturbance and paresthe sias in lower limbs. The patient was being followed up by the spinal team for back pain with radicular irradiation of long evolution. At that time, in the magnetic resonance imaging (MRI) she had the presence of three mild thoracic discs herniations in contact with the spinal cord without compromising it. She had refused the surgical treatment that was proposed at that time.
On physical examination the patient presented: Para paresis in the lower limbs with a greater predominance on the left side. Left femoral hyperreflexia, Babinski sign positive, Clonus exhaustible. Abolished abdominal skin reflex. Abolished muscle stretch reflex on the right lower limb. Sensory hemi level: T7-8 right and T8-9 left. Hypo tonic sphincters with urinary retention.
Due to suspicion of acute spinal cord syndrome, the patient was admitted to the hospital and a new MRI of the dorsolumbosacral spine was performed, which re vealed the progression of the extruded hernias at the level of T6-7 and T7-8 on the left side and T9-10 on the right side (Fig 1, A-D). For a better pre-surgical analysis a CT myelography with intrathecal contrast was requested (Fig 1, E-H).

Figure 1 MRI of the dorsal column, sagittal cut, T2 sequences (A), axial T2 cuts (B, C, D) and CT-Myelography sagittal cut (E), and axial (F, G, H). Disc extrusions in T6-7 and T7-8 ascending in a posterior, medial direction with laterality to the left. They occupy the anterior and left lateral epidural space with imprint and medullary compression. Voluminous T9-10 disc extrusion with ascending fragment behind the T9 vertebral body in a posterior, medial and bilateral direction. It occupies the anterior epidural space with imprint and medullary compression. Signs of myelomalacia are seen
Due to the greater involvement of the left side (ex haustible Clonus, Babinski, motor deficit), it was decided to perform a two-stage intervention with discectomy and arthrodesis, first in T6-7 and T7-8, through a left transthoracic approach and secondly in the opposite site at T9-10. Depending on the neurologic recovery after the first approach the lapse for the second were going to be decided. General anesthesia with selective bronchial intubation was performed. The patient was placed in the right lateral decubitus position. Intervertebral levels T6-7 and T7-8 were located using radioscopic guidance. Left video-assisted thoracoscopic surgery (VATS) was performed through three 12-mm trocars in anterior ax illary line with dissection of the parietal pleura. The 7th and 8th ribs and T6-7 and T7-8 spaces were located. The T7 segmental artery was clipped. Rib dissection was per formed. To have better access a MISS (minimal invasive spinal surgery) lateral approach through 6 cm accessory thoracotomy with rib resection was performed. Resec tion of the head of the 7th rib was performed plus partial resection of the lower/posterior left endplate of T6 and upper/posterior left endplate of T7 with the correspond ing disc. Then a lateral foraminotomy to expose the the cal sac was done. The spinal cord was released but not mobilized by a discectomy towards the ventral cavity previously generated. The same procedure was carried out on space T7-8. Finally, the rib structural grafts were placed in the intersomatic space for arthrodesis (Fig. 2). A pleural drainage was connected to a thoracic drainage system.
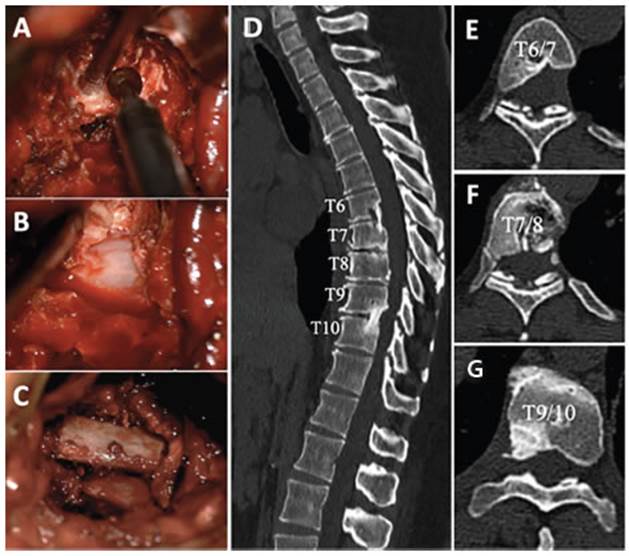
Figure 2 Partial resection of the lower left endplate of T6 with discectomy (A). Thecal sac released (B). Rib structural grafts placed in the intersomatic space (C). CT postoperative sagittal reconstruction (D) and axial cuts (E, F, G). 24 months from the first surgery with adequate intersomatic arthrodesis and no kyphotic angulation
Immediately after the surgery, the patient progressed favorably, recovering sensation below the left hemi level T8 and motor skills in both lower limbs gaining capac ity to walk, but she continued with paresthesias in her feet and lack of complete sphincter control. She was dis charged 10 days after surgery, continued with rehabilita tion and controlled periodically.
At 12 months after the first intervention the mo tor function was recovered almost completely but con tinued with paresthesias and sphincter disability and was decided to perform the second stage surgery. It was performed on the opposite site to decompress the right T9-10 level. Differently from the first decompression, a minimally invasive retropleural transthoracic approach was done without placing a pleural drainage and permit ting a rapid recovery and hospital discharge in time of COVID-19 pandemic. Subsequently, the patient recovered thermoalgesia and dorsiflexion of both feet, but she did not recover normal bladder function, so she continued treatment with tamsulosin and sphincter rehabilitation. Given that in the postoperative controls the patient did not present back pain or signs of spinal instability in ra diological studies, it was decided not to perform fixation of the thoracic spine through a posterior approach.
The patient has signed the informed consent where she authorizes the publication of photos of the surgery and the images of its studies in the scientific journal for academic purposes.
Discussion
Symptomatic TDH is a relatively uncommon pathology compared with symptomatic hernia tions of the cervical and lumbar spine. Its fre quency ranges from 0.15 to 1.7% of all spine discs herniations, of which surgical are only 0.15 - 4%1. More than 70% of the TDH are asymptom atic and when are symptomatic are not strongly associated with herniated disc position, level, composition, and size1. The incidence of TDH on imaging studies has been estimated at 11% to 37%2; 75% of TDH cases are located below T7-8 levels and can be central, lateral or posterolat eral. The disc between T11-12 is the most vul nerable place since it presents greater mobility than the upper segments with weakness of the posterior longitudinal ligament at that level l3-5. One of the peculiarities of TDH is the frequent presentation with calcification or ossification, which is estimated to be in around 42% of cases. When the disc is calcified, the risk of intrathe cal extension increases due to erosion and thin ning of the thecal sac6,7. TDH is considered gi ant, according to Hott et al., when it occupies more than 40% of the medullary canal on CT or MRI8. The onset of symptoms in the event of compression of the spinal cord can be gradual and includes pain, lack of strength in the lower limbs, numbness, paresthesias, and sphincter dysfunction6.
Multilevel TDH with symptoms is extremely rare. In the literature, the first case was reported in 1954 by Svien and Karavitis9. For the year 1995 worldwide, only 26 cases of dorsal hernias with simultaneous involvement of several levels were reported, of which 23 cases with 2 levels, 2 cases with 3 levels, as our case, and 1 case with 5 lev els10. The presence of multiple TDH in a symptom atic patient is a challenge for the surgeon since it is necessary to identify which one is responsible for the neurological symptoms. CT and MRI are essential to planning surgery. Occasionally a CT Myelography can be done to get a better under standing of the characteristics of the hernias8.
When the surgery is indicated, the approach depends on the localization of the hernia. When the hernia is central or posterolateral, the an terior transthoracic approach is recommended and can be performed by a minimally invasive transpleural (thoracoscopy or thoracotomy) or retropleural way. This approach allows direct vi sualization of the hernia without mobilization of the spine cord2. Based on cadaveric and clinical studies it doesn’t generate significant instabil ity in the spine, therefore instrumentation is not needed when only one level is affected11,12. When the hernia is lateral, the posterolateral approach can be done but should be added posterior instru mentation due to the instability generated (facetectomy, costotransversectomy). In our case, the transthoracic anterior approach was performed minimally invasive with parietal pleurectomy in the 1st stage in one side and retropleural in the 2nd stage in the other side. We observed better recovery in retropleural approach with shorter hospitalization probably because we didn´t need to use a pleural drainage and the pain was lower. Another advantage of the retropleural approach is that permits better control of the cerebrospinal fluid when a dural lesion occurs, avoiding the di rect drainage into the interpleural space.
In our case, the graft from the extracted rib was used to perform the intervertebral fusion but no fixation system was used, which could be controversial due to the 3-level discectomy that can generate more instability than a single level. We believe that having performed the surgery in 2 stages separated by 12 months, we gave the possibility of arthrodesis in the first 2 levels. In postoperative radiological control studies we observed a good intersomatic arthrodesis and the patient did not show any sign of instability or back pain.
This case allows us to demonstrate the good results of the transthoracic minimally invasive approach in a patient with multiple TDH. This technique offers the best chance for decompres sion with minimal manipulation of the spinal cord. We didn’t add instrumentation but should be considered if multiple levels at the same time will be done.














