Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Archivos argentinos de pediatría
Print version ISSN 0325-0075On-line version ISSN 1668-3501
Arch. argent. pediatr. vol.114 no.5 Buenos Aires Oct. 2016
http://dx.doi.org/10.5546/aap.2016.426
ORIGINAL ARTICLE
http://dx.doi.org/10.5546/aap.2016.eng.426
Perinatal factors associated with neonatal mortality in very low birth weight infants: A multicenter study
Carlos Grandi, M.D.a, Agustina González, M.D.b, José Zubizarreta, M.D.c, and NEOCOSUR Neonatal Network
a. Independent Researcher, Health Research Council, Maternidad Sardá, Buenos Aires, Argentina.
b. Hospital San José, Santiago, Chile.
c. Division of Decision, Risk and Operations, Affiliated Faculty, Statistics Department. Graduate School of Business, Columbia University, United States.
d. Members of the NEOCOSUR Neonatal Network (see Annex).
E-mail address: Carlos Grandi, M.D., cgrandi@intramed.net
Funding: This research study was conducted with the support of the Ramón Carrillo-Arturo Oñativia scholarship program, granted by the National Ministry of Health of Argentina through the National Health Research Committee (Comisión Nacional Salud Investiga).
Conflict of interests: None.
Received: 02-29-2016
Accepted: 05-09-2016
ABSTRACT
Introduction. Objectives. To assess risk factors associated withneonatal mortality in very low birth weight (VLBW) infants (< 1500 g) and the impact of the administration of antenatal corticosteroids.
Population and methods. Retrospective analysis of a VLBW infant cohort from 26 tertiary care and teaching sites member of the South American Neonatal Network (NEOCOSUR), which includes Argentina, Brazil, Chile, Paraguay, Peru, and Uruguay, conducted between 2000 and 2011 on 11 455 records. Maternal and neonatal characteristics and morbidity were compared between deceased VLBW infants and those who survived to discharge. Outcome measures associated with neonatal mortality were established by logistic regression. The effect of antenatal corticosteroids on neonatal morbidity and mortality was estimated using the matching method.
Results. The neonatal mortality rate was 22.3%, and variability among sites was elevated. Factors that were independently associated with a lower mortality of VLBW infants included the administration of antenatal corticosteroids (OR: 0.49, 95% CI: 0.43-0.54), a better birth weight Z-score (OR: 0.63, 0.61-0.65), arterial hypertension (OR: 0.67, 0.58-0.77), and C-section (OR: 0.75, 0.65-0.85). The matching method allowed reducing the risk of death by 38% in association with antenatal corticosteroids.
Conclusions. Major perinatal factors were identified in association with neonatal mortality in VLBW infants, and the impact of antenatal corticosteroid use in the NEOCOSUR Network was demonstrated.
Key words: Neonatal mortality; Very low birth weight infant; Preterm infant; Risk factors; Multicenter studies.
INTRODUCTION
Prematurity (gestational age [GA] < 37 + 0 weeks) is the main direct cause of death in newborn infants (NBIs), especially in very low birth weight (VLBW) babies (< 1500 g).1 Prematurity is also a major indirect cause of death, and poverty is strongly associated with a greater risk; therefore, almost 99% of neonatal deaths occurring worldwide take place in low- and middle-income countries.2
In addition, more than half of infants who survive to hospital discharge have severe complications, which are mostly chronic and have an impact on the subject's quality of life and that of his/her family, and which require a significant amount of medical resources.
Information is needed on which risk factors (RFs) lead to such outcomes in order to prioritize interventions and plan their development, assess the effectiveness of interventions aimed specifically at RFs, and assess national and international trends over time.3,4
Although results are available regarding VLBW infants from developed countries, few studies have assessed the morbidity and mortality of Latin American VLBW infants.5,6 A problem-solving strategy is for neonatal care sites to become members of specialized, collaborative, thematic networks; some of the benefits they provide include criteria standardization, resource enhancement, site comparison, and identification of the most beneficial medical practices (benchmarking).7
This study shows the consolidation of the South American Neonatal Network (NEOCOSUR), which has monitored, for the past 15 years, the neonatal intensive care units of six South American countries (Argentina, Brazil, Chile, Paraguay, Peru, and Uruguay).
For this reason, the goals of this study included investigating RFs independently associated with mortality in VLBW infants born in
the Neonatology units from the NEOCOSUR Network, and assess the impact of antenatal corticosteroids.
The hypothesis indicated that the administration of antenatal corticosteroids may reduce neonatal mortality and selected morbidities in NBIs < 1500 grams.
POPULATION AND METHODS
A retrospective analysis was done using a multicenter cohort of live NBIs with a birth weight (BW) between 500 g and 1500 g corresponding to the NEOCOSUR Network. Inclusion criteria were a GA equal to or greater than 24+0 weeks, and a BW between 500 g and 1500 g. Exclusion criteria were death in the delivery room, NBI referred to another facility, and no recording of mortality to discharge.
Data were collected in a prospective, systematic manner from 26 units between January 1st, 2000 and December 31st, 2011, and each event was strictly defined. Data regarding the mothers and the VLBW infants from each site were entered using the online electronic database established by the Database Unit.8
Outcome measures were neonatal mortality and morbidity at the time of hospital discharge. Independent outcome measures were maternal age at the time of delivery, level of education, antenatal care visits, twin pregnancy, diabetes, arterial hypertension, antenatal corticosteroids (complete, incomplete, or missing treatment), mode of delivery (vaginal, C-section with or without labor), gender (male/female), GA (completed weeks at the time of childbirth) by date of the last menstrual period (LMP) or early ultrasound scan (first trimester), BW (grams), BW Z-score9 , Apgar score at 5 minutes of 0-3, resuscitation in the delivery room, and type of facility (public/private). Morbidities included respiratory distress syndrome (RDS: hyaline membrane disease), assisted mechanical ventilation and duration in days, continuous positive airway pressure (CPAP) in days, surfactant (and number of doses), bronchopulmonary dysplasia (BPD: oxygen for more than 28 days), hemodynamically significant patent ductus arteriosus (PDA), early sepsis (< 72 h) with positive blood culture, necrotizing enterocolitis (NEC: grade 2 or higher, as per Bell), intracranial hemorrhage (ICH: grade 3 or 4, as per Papile), periventricular leukomalacia (PVL), major complications combined (MCC, two or more of the following: grade 3-4 BPD-ICH, grade 2-3 NEC), and length of stay (days).
Prematurity was defined as per the World Health Organization (WHO) and the International Statistical Classification of Diseases and Related Health Problems (ICD-10), and was classified into extremely preterm birth (< 28+0 weeks), very preterm birth (28+0 - 31+6 weeks), and moderate preterm birth (32+0 - 36+6 weeks).10
The BW Z-score was estimated using an Argentine population reference.9 Small for gestational age (SGA) and large for gestational age (LGA) were defined as per Gruenwald11 based on weight for GA and gender above or below two points of the median Z-score, respectively. A Z-score of +2 corresponds to the 97th percentile, whereas a Z-score of -2, to the 3rd percentile.
Z-scores corresponded to the overall population and NBIs born between 24+0 and 32+6 weeks. SGA and LGA were described only for NBIs born between 24+0 and 32+6 weeks in order to prevent over-representation of both conditions because the cut-off limit for entering the database is based on a birth weight < 1500 g.
Comparisons included the predictor score of mortality in VLBW infants developed by the NEOCOSUR Network.12 Briefly, the NEOCOSUR score estimates the probability of death of VLBW infants considering their BW, GA, Apgar score at 5 minutes, life-threatening congenital malformations, antenatal corticosteroids, and gender. The mortality tendency analysis was done using a linear regression model.
The length of stay was defined as days from birth to discharge. For analysis purposes, deaths were censored, similarly to what has been done in survival studies.
Central tendency measures (mean, median, and proportions) and dispersion measures (standard deviation, 95% confidence interval [CI], and interquartile range [IQR]) were estimated. The Mann-Whitney U test and Student's t test were used to compare continuous outcome measures. The %2 test with Yates' correction was used to compare categorical outcome measures.
A multiple logistic regression analysis was used to explore the independent effect of different conditions on neonatal mortality. Models were adjusted for public or private facilities, maternal age, multiple pregnancy, maternal hypertension, antenatal corticosteroids, mode of delivery, Apgar score at 5 minutes < 3, gender, GA, BW Z-score, and confirmed early sepsis. The group of survivors to discharge was established as the reference group. Results are described as adjusted odds ratio (aOR) with the corresponding 95% CI, and models were calibrated using the Hosmer-Lemeshow test, and their discriminatory power was established using ROC curves.
Matching by antenatal corticosteroid use
The effect of administering antenatal corticosteroids was estimated in relation to neonatal mortality and morbidity of VLBW infants using the matching method, which consists in having groups that are identical in everything except for treatment. Matching methods allow establishing two samples that are as likely as possible in terms of observed covariables, similar to a randomized experiment.13
A p-value below 0.05 was considered statistically significant. The following software programs were used: Statistica 9.0 (Statsoft, Tulsa, OK, USA), Stata 12 (College Station, Texas, USA), and EPIDAT 2.0 (PAHO/WHO and Government of Galicia).
The study was authorized by the Ethics Committee of Hospital Materno Infantil Ramon Sarda, and anonymity of both sites and patients was maintained given that only their codes were used.
RESULTS
Out of 11 991 VLBW infants entered into the database between 2000 and 2011 (12-year period), 11 455 met the eligibility criteria (Figure 1).
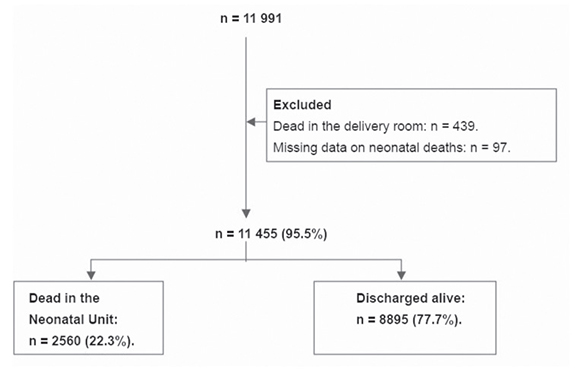
Figure 1. Flow chart of the studied population, NEOCOSUR, 2000-2011
The overall neonatal mortality rate (NMR) for the study period was 22.3% (95% CI: 21.6-23.1), and a growing trend was observed (p= 0.441, Figure 2). However, risk-adjusted mortality (NEOCOSUR score) decreased 60% over the study period, even though inter-site variability was high.
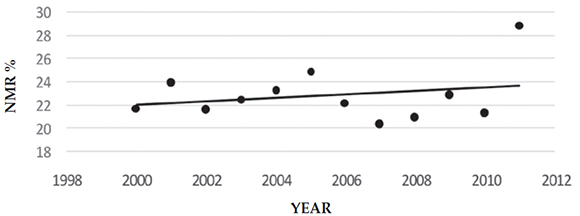
Figure 2. Trend in neonatal mortality rate (NEOCOSUR, 2000-2011)
NMR: neonatal mortality rate.
Overall survival to hospital discharge was 77.7%, whereas specific survival was directly related to GA: from 54% for extremely preterm infants, to 85.8% for very preterm infants, and to 90.6% for moderately preterm infants (p < 0.001).
The degree of variability of morbidity outcomes was the same as for mortality by site (data not shown).
The mothers of deceased infants were more frequently adolescents and had undergone a C-section with labor, compared to the mothers of survivors (p < 0.001) (Table 1).
Table 1. Comparison of demographic, pregnancy, and delivery characteristics between deceased and surviving infants (NEOCOSUR, 2000-2011; n= 11 455)

Male gender, a lower GA, BW and BW Z-score, and SGA predominated among deceased VLBW infants in comparison with survivors. In contrast, they had almost three times more chances of being extremely preterm, showed a greater respiratory depression at birth and, therefore, twice the need for resuscitation in the delivery room (p < 0.001) (Table 2).
Table 2. Comparison of neonatal characteristics between deceased and surviving infants (NEOCOSUR, 2000-2011; n= 11 455)

Table 3 shows that, compared to survivors, deceased VLBW infants had a mortality predictor score that was three times higher, a greater rate of RDS, mechanical ventilation requirement, surfactant requirement, BPD, intraventricular hemorrhage (IVH), NEC, PDA, and early sepsis, and twice the combined score (p < 0.001).
Table 3. Neonatal morbidities: deceased and surviving infants (NEOCOSUR, 2000-2011; n= 11 455)

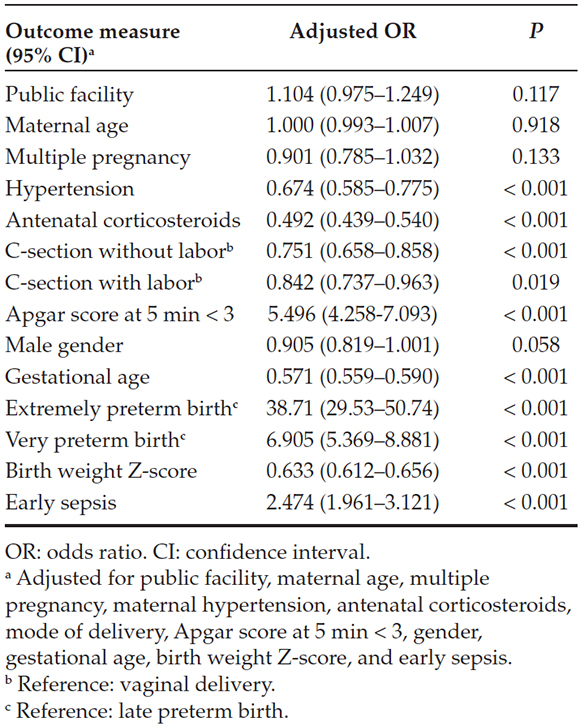
RFs that were independently associated with a greater mortality included GA of less than 32 weeks, an Apgar score at 5 min < 3, and early sepsis. RFs that were independently associated with a lower mortality included antenatal corticosteroid use, a better BW Z-score, hypertension in pregnancy, and C-section (Table 4). Model adjustment was successful (Hosmer-Lemeshow, p= 0.147), and the area under the ROC curve was 0.825.
Table 4. Factors associated with neonatal mortality in very low birth weight infants: multiple logistic regression analysis (NEOCOSUR, 2000-2011; n= 11 455)
No differences were observed in NMR by volume of hospitalized NBIs. The NMR in the public sector increased to 23.2%, whereas it reached 19.8% in the private sector (OR: 1.22, 95% CI: 1.10-1.36, p < 0.001).
The frequency of major complications combined (MCC) at the time of hospital discharge ranged between 42.8% and 74.3% across the 26 sites, with a median of 60.8% (95% CI: 5961). When analyzed by type of facility, MCC was 59.3% (58-60) in public facilities, and 57.7% (56-59) in private ones (p= 0.121).
The median length of stay was 47 days (IQR: 41 days), and significant differences were observed among sites, similar to those observed in terms of mortality and morbidity.
Matching: The final sample following matching included 4192 NBIs (2096 in each arm). VLBW infants whose mothers had received antenatal corticosteroids evidenced a 38% reduction in the risk of death compared to those whose mothers had not (p < 0.001). Similar effects were observed for asphyxia (OR: 0.49) and RDS (OR: 0.62). No association was identified between the other morbidities and antenatal corticosteroid use (Table 5).
Table 5. Risks for different perinatal adverse outcomes associated with the administration of antenatal corticosteroids (NEOCOSUR, 2000-2011; n= 4192 newborn infants)

DISCUSSION
This is the second multicenter study conducted in Latin America to explore RFs associated with neonatal mortality of VLBW infants and the impact of antenatal corticosteroids on the prevention of adverse perinatal outcomes. It is more updated, and its sample size is larger.14
It has been demonstrated that antenatal corticosteroid use, a better BW Z-score, arterial hypertension, and C-section were factors independently associated with a lower mortality in VLBW infants, together with the impact of antenatal corticosteroids on neonatal mortality and morbidity.
Overall NMR tended to increase over the study period, with a wide variability among sites, similar to what has been published.15 However, risk-adjusted mortality reduced remarkably, which highlights the need to adjust results when analyzing tendencies.
GA plays a major role in VLBW infants' prognosis, and survival was observed to increase progressively in association with an older GA.
The following four groups of factors independently associated with an unfavorable outcome were identified: factors associated with obstetric care (no exposure to antenatal corticosteroids, vaginal delivery), factors related to biological outcome measures (male gender, prematurity < 32 weeks, intrauterine growth restriction), factors related to childbirth care (Apgar score at 5 minutes < 3), and factors associated with intensive care (early sepsis).
The characteristics of mothers whose VLBW infants had died show the strong influence of the social component and access to care on perinatal outcomes, which is consistent with a recent systematic review.16
It is known that there is an association between hypertension during pregnancy and a small size at birth, which may speed fetal pulmonary development and, therefore, reduce neonatal mortality.17 Although this is a highly controversial topic, some retrospective studies indicate that the rate of prematurity-related complications may be reduced if the child is born via C-section.18,19 These results underline the need for an early screening of antenatal RFs and an adequate labor and NBI resuscitation in relation to mortality and GA, BW, intrauterine growth restriction, and neonatal asphyxia.
The wide inter-site variability has also been reported in other studies20,21 , and it may be accounted for by both each unit population characteristics and inherent risks, and the diagnostic and therapeutic interventions implemented in each site, especially professional conduct when providing care to preterm infants born at the threshold of viability. Another critical aspect to take into account is that there is a severe nurse shortage in Latin America, documented in a study conducted by the NEOCOSUR Network.22
The RFs observed here to be independently associated with mortality are consistent with those previously described in several prediction models.23,24
The information collected by epidemiological networks allows studying the best strategies to reduce neonatal mortality and morbidity, based on processes to improve perinatal care quality.25 Thus, VLBW infant mortality has been reported to range between 12.4% and 28% as per the neonatal networks of developed countries (the Euro Neo Net/Euro-Peristat Network26 , the Vermont-Oxford Network27 ,the Canadian Neonatal Network28 , the National Institute of Child Health and Human Development [NICHD]29 , the Spanish Neonatology Society).23 In contrast, the results obtained by the Brazilian Neonatal Research Network30 and the Neonatology Network of Public Hospitals from the City of Buenos Aires31 describe more unfavorable results, especially associated with a low use of antenatal corticosteroids. However, when analyzing such differences, it is necessary to consider the denominator used to estimate the mortality rate and the fact that inclusion criteria vary from one study to another32 , in addition to differences in population, perinatal practices, and resources.
The matching method has clearly demonstrated, in this wide and varied population, a maternal corticosteroid coverage of 76.5% (95% CI: 75-77), and its impact on neonatal mortality (p < 0.001). By restricting the analysis to NBIs < 35 + 0 weeks, which is at present the indication for corticosteroids, the protective effect increased slightly (aOR: 0.47; 95% CI: 0.42-0.53). During the study period, the percentage of antenatal corticosteroid use remained stable. This is similar to the findings of a Chilean study33 , but contrasts those of a Brazilian study34 , in which only 54% received at least one dose, whereas in the USA, 79% of pregnant women have received this drug for the past 15 years35 , a value very close to our study.
Differences in the length of stay of VLBW infants are not just the result of nosocomial complications, and it may be speculated that such differences may be attributed to varying discharge practices.
One of the limitations of this study is that it is a retrospective analysis, and its biases and confounding factors were not controlled (the final model accounted for 20% of variability in neonatal mortality), so our results may have been affected, to a certain extent, by residual confusion. The analyzed population accounts for 8% to 40% of VLBW infants at a national level, so results cannot be generalized to the entire population.
However, this multicenter study provides data on death and survival of preterm VLBW infants with the main morbidities observed in public and private hospital units that are considered national reference perinatal care centers.
The main strengths of this study are its sample size and multicenter nature, which allowed for a geographic distribution, prospective and systematic data collection, and an adequate calibration and discrimination of the final model.
CONCLUSIONS
The independent risk of different perinatal conditions associated with neonatal mortality in VLBW infants was estimated, and the hypothesis regarding the impact of antenatal corticosteroid use in the NEOCOSUR Network was demonstrated.
Acknowledgments
We would like to thank the NEOCOSUR Network member sites that participated in this study (see Annex) and the Database Unit for preparing the database (Ivonne D'Apremont, M.D.).
ANNEX
The following members of the NEOCOSUR Network collaborated with the study:
ARGENTINA
Guillermo Colantonio, Jorge Zapata, Gastón Pérez, Liliana Rochinotti, Inés Galíndez, Luis Prudent (Clínica y Maternidad Suizo Argentina, Buenos Aires); Gonzalo Mariani, José María Ceriani, Silvia Fernández, Pablo Brener, Carlos Fustiñana † (Hospital Italiano, Buenos Aires); Liliana Roldán, Héctor Sexer, Gladys Sáa, Débora Sabatelli, Elizabeth Lombardo, María Laura Gendra, Paula Molina, Jorge Tavosnaska (Hospital Juan Fernández, Buenos Aires); Daniel Agost, Gabriela Torres, Jorge Ríos, Augusto Fischetti, Mónica Rinaldi (Hospital Lagomaggiore, Mendoza); Claudio Solana, Elio Rojas, Ricardo Nieto, Javier Meritano, Miguel Larguia, Carlos Grandi (Maternidad Sardá, Buenos Aires); Marcelo Decaro, Lionel Cracco, Gustavo Bassi, Noemí Jacobi, Edith Martínez, María San Miguel, Andrea Brum, Néstor Vain (Sanatorio de la Trinidad, Buenos Aires).
CHILE
Jorge Fabres, Alberto Estay, Alvaro González, Mariela Quezada, Soledad Urzúa, Javier Kattan (Hospital Clínico Pontificia Universidad Católica de Chile, Santiago); Solange Rojas, Sandra Vignes, Guillermo Marshall, Luis villarroel (Unidad Base de Datos, Pontificia Universidad Católica, Santiago); Rodrigo Ramírez, María Eugenia Hübner, Jaime Burgos, Jorge Catalán (Hospital Clínico Universidad de Chile, Santiago); Lilia Campos, Roxana Aguilar, Sergio Treuer, Jimena Giaconi, Aldo Bancalari, Jorge León del Pedregal (Hospital Guillermo Grant, Concepción); Marisol Escobar, Viviana Veas, Daniela Sandino, Antonio Salvado, Alejandra Núñez, Jane Standen (Hospital Gustavo Fricke, Viña del Mar); Agustina González, Claudia Avila, Ana Luisa Candia (Hospital San José, Santiago); Claudia Toro, Beatriz Milet, Angélica Alegría, Patricia Mena (Hospital Dr. Sótero del Río, Santiago).
PARAGUAY
Elizabeth Céspedes, Ramón Mir, Elvira Mendieta, Larissa Genes, José Lacarruba (Departamento de Hospital de Clínicas de Asunción).
PERÚ
Verónica Webb, Fabiola Rivera, Enrique Bambaren, Marilú Rospigliosi, Margarita Llontop, Jaime Zegarra (Hospital Cayetano Heredia, Lima).
URUGUAY
Sandra Gugliucci, Ana Lain, Alicia Prieto, Cristina Hernández, Mariza Martínez, Gabriela Bazán, Daniel Borbonet, Rubén Panizza † (Facultad de Medicina, Hospital Pereira Rossell, Servicio de Recién Nacidos, Montevideo).
1. March of Dimes, PMNCH, Save the Children, WHO. Born too soon: The Global Action Report on Preterm Birth. Geneva: World Health Organization; 2012. [ Links ]
2. Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: When? Where? Why? Lancet 2005;365(9462):891-900. [ Links ]
3. Bryce J, Boschi-Pinto C, Shibuya K, Black R. wHo estimates of the causes of death in children. Lancet 2005;365(9465):1147-52. [ Links ]
4. Liu L, Johnson HL, Cousens S, Perin J, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 2012;379(9832):2151-61. [ Links ]
5. Belizán JM, Cafferata ML, Belizán M, Tomasso G, et al. Goals in maternal and perinatal care in Latin America and the Caribbean. Birth 2005;32(3):210-8. [ Links ]
6. De Almeida MF, Guinsburg R, Martinez FE, Procianoy RS, et al. Perinatal factors associated with early deaths of preterm infants born in Brazilian Network on Neonatal Research centers. J Pediatr (Rio J) 2008;84(4):300-7. [ Links ]
7. Hummler H. Benchmarking in neonatal intensive care: obstetrical and neonatal practices and registration policies may influence outcome data. Arch Dis Child Fetal Neonatal Ed 2013;98(2):F96-7. [ Links ]
8. Fernández R, D'Apremont I, Domínguez A, Tapia JL, ET al. Supervivencia y morbilidad en recién nacidos de muy bajo peso al nacer en una Red Neonatal sudamericana. Arch Argent Pediatr 2014;112(5):405-12. [ Links ]
9. Urquia ML, Alazraqui M, Spinelli HG, Frank JW. Referencias poblacionales argentinas de peso al nacer según multiplicad del parto, sexo y edad gestacional. Rev Panam Salud Publica 2011;29(2):108-19. [ Links ]
10. WHO: recommended definitions, terminology and format for statistical tables related to the perinatal period and use of a new certificate for cause of perinatal deaths. Modifications recommended by FIGO as amended October 14, 1976. Acta Obstet Gynecol Scand 1977;56(3):247-53. [ Links ]
11. Gruenwald P. Growth of the human fetus. I. Normal growth and its variation. Am J Obstet Gynecol 1966;94(8):1112-9. [ Links ]
12. Marshall G, Tapia JL, D'Apremont I, Grandi C, et al. A new score for predicting neonatal very low birth weight mortality risk in the NEOCOSUR South American Network. J Perinatol 2005;25(9):577-82. [ Links ]
13. Zubizarreta JR. Using mixed integer programming for matching in an observational study of acute kidney failure after surgery. J Am Stat Assoc 2012;107(500):1360-71. [ Links ]
14. Grupo Colaborativo Neocosur. Very-low-birth-weight infant outcomes in 11 South American NICUs. J Perinatol 2002;22(1):2-7. [ Links ]
15. Draper ES. Evaluating and comparing neonatal outcomes. Arch Dis Child Fetal Neonatal Ed 2010;95(3):F158-9. [ Links ]
16. Upadhyay RP, Krishnan A, Rai SK, Chinnakali P, et al. Need to focus beyond the medical causes: a systematic review of the social factors affecting neonatal deaths. Paediatr Perinat Epidemiol 2014;28(2):127-37. [ Links ]
17. Von Dadelszen P, Magee LA, Taylor EL, Muir JC, et al. Maternal hypertension and neonatal outcome among small for gestational age infants. Obstet Gynecol 2005;106(2):335-9. [ Links ]
18. Skupski DW, Greenough A, Donn SM, Arabin B, et al. Delivery mode for the extremely premature fetus: a statement of the prematurity working group of the World Association of Perinatal Medicine. J Perinat Med 2009;37(6):583-6. [ Links ]
19. Alfirevic Z, Milan SJ, Livio S. Caesarean section versus vaginal delivery for preterm birth in singletons. Cochrane Database Syst Rev 2012;6:CD000078. [ Links ]
20. Draper ES, Zeitlin J, Fenton AC, Weber T, et al. Investigating the variations in survival rates for very preterm infants in 10 European regions: the MOSAIC birth cohort. Arch Dis Child Fetal Neonatal Ed 2009;94(3):F158-63. [ Links ]
21. Field D, Smith L, Manktelow B, McParland P, et al. Interpretation of early life mortality rates. Arch Dis Child Fetal Neonatal Ed 2015;100(2):F99-100. [ Links ]
22. Grandi C, González A, Meritano J, Grupo Colaborativo Neocosur. Riesgo de morbimortalidad neonatal de recién nacidos menores de 1500 g asociado al volumen de pacientes, personal médico y de enfermería: una investigación multicéntrica latinoamericana. Arch Argent Pediatr 2010;108(6):499-510. [ Links ]
23. Moro M, Figueras-Aloy J, Fernández C, Doménech E, et al. Mortality for newborns of birthweight less than 1500 g in Spanish neonatal units (2002-2005). Am J Perinatol 2007;24(10):593-601. [ Links ]
24. Pollack MM, Koch MA, Bartel DA, Rapoport I, et al. A comparison of neonatal mortality risk prediction models in very low birth weight infants. Pediatrics 2000;105(5):1051-7. [ Links ]
25. Evans N, Hutchinson J, Simpson JM, Donoghue D, et al. Prenatal predictors of mortality in very preterm infants cared for in the Australian and New Zealand Neonatal Network. Arch Dis Child Fetal Neonatal Ed 2007;92(1):F34-40. [ Links ]
26. Euro Peristat. European Perinatal Health Report. Health and Care of Pregnant Women and Babies in Europe in 2010. [Acceso: 11 de mayo de 2016]. Disponible en: http://www.europeristat.com/images/doc/Peristat%202013%20v2.pdf. [ Links ]
27. Horbar JD, Carpenter JH, Badger GJ, Kenny MJ, et al. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics 2012;129(6):1019-26. [ Links ]
28. Shah PS, Sankaran K, Aziz K, Allen AC, et al. Outcomes of preterm infants 29 weeks gestation over 10-year period in Canada: a cause for concern? J Perinatol 2012;32(2):132-8. [ Links ]
29. Stoll BJ, Hansen NI, Bell EF, Shankaran S, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 2010;126(3):443-56. [ Links ]
30. Guinsburg R, de Almeida MF, de Castro JS, Silveira RC, et al. Death or survival with major morbidity in VLBW infants born at Brazilian neonatal research network centers. J Matern Fetal Neonatal Med 2016;29(6):1005-9. [ Links ]
31. Red de Neonatología de los Hospitales Públicos de la Ciudad Autónoma de Buenos Aires. Morbimortalidad de recién nacidos con menos de 1500 gramos asistidos en hospitales públicos de la ciudad de Buenos Aires. Arch Argent Pediatr 2012;110(5):394-403. [ Links ]
32. Guillen Ú, DeMauro S, Ma L, Zupancic J, et al. Survival rates in extremely low birthweight infants depend on the denominator: avoiding potential for bias by specifying denominators. Am J Obstet Gynecol 2011;205(4):329.e1-7. [ Links ]
33. Gonzalez R, Merialdi M, Lincetto O, Lauer J, et al. Reduction in neonatal mortality in Chile between 1990 and 2000. Pediatrics 2006;117(5):e949-54. [ Links ]
34. Azeredo Cardoso RC, Guimaraes Flores PV, Lima Vieira C, vergetti Bloch K, et al. Infant mortality in a very low birth weight cohort from a public hospital in Rio de Janeiro, RJ, Brazil. Rev Bras Saude Mater Infant 2013;13(3):237-46. [ Links ]
35. Fanaroff AA, Stoll BJ, Wright LL, Carlo Wa, et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol 2007;196(2):147.e1-8. [ Links ]











 text in
text in 


