Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Archivos argentinos de pediatría
Print version ISSN 0325-0075On-line version ISSN 1668-3501
Arch. argent. pediatr. vol.114 no.6 Buenos Aires Dec. 2016
http://dx.doi.org/10.5546/aap.2016.514
ORIGINAL ARTICLE
http://dx.doi.org/10.5546/aap.2016.eng.514
Knowledge level, attitude and own experience of health professionals about breastfeeding and breast milk in a city of Turkey: Cross-sectional study
Aylin Baydar Artantas, M.D.a, Burcu Kayhan Tetik, M.D.b, Melek Kılıc, Nursec, İrep Karatas Eray, M.D.a, Nazan Cetin, Dieticiand, Sinem Güney, Midwifee, Dogan Akdogan, M.D.d, Umut Domac, M.D.d, Yusuf Ustu, Associate Professorf and Mehmet Ugurlu, Associate Professorf
a. Ankara Ataturk Training and Research Hospital, Department of Family Medicine.
b. Inonu University Faculty of Medicine, Department of Family Medicine.
c. Ministry of Health of Turkey.
d. Directorate of Public Health of Ankara.
e. Zekai Tahir Training and Research Hospital.
f. Yildmm Beyazit University Faculty of Medicine, Department of Family Medicine.
E-mail address: Aylin Baydar Artantas, M.D.: draylinbaydar@yahoo.com
Funding: None.
Conflict of interest: None.
Received: 3-30-2016
Accepted: 8-19-2016
ABSTRACT
Introduction: Worldwide consensus about breastfeeding is that the infant should exclusively be breastfed until six months of life. Despite this, the rate of exclusive breastfeeding for the first six months of age is low in so many countries including Turkey. The aim of this study was to evaluate the knowledge, the attitudes and the own experiences of health professionals about breastfeeding and breast milk, in a metropolitan city in Turkey.
Materials and methods: This study was performed between July 2012 and December 2013. Study subjects included healthprofessionals working in the university hospitals, research and training hospitals, public and private hospitals; child, adolescent, women and reproductive health services centers, family health centers, and community health centers located in Ankara. A questionnaire was used to collect data. SPSS 11.5 package program was used for statistical analysis.
Results: A total of 715 people participated in this study. From those who had children themselves 3.4% (n= 16) had not breastfed their babies at all, and 7.6% (n= 36) had breastfed their baby until second year of age. It was found that 28.4% of the participants had poor, 43.1% had average and 28.5% had good knowledge level about breastfeeding and breast milk.
Conclusion: This study reflects the lack of knowledge about breastfeeding and breast milk among the health professionals in Turkey. Although a great majority of participants agree the recommendation of WHO about the duration ofbreastfeeding, the percentage ofbreastfeeding of health care professionals during recommended period was very low.
Keywords: Breast milk; Breastfeeding; Health care professionals; Turkey.
INTRODUCTION
World health organization(WHO) and the United Nations International Children's Emergency Fund(UNICEF) recommend that the infants will exclusively be fed with breast milk until six months of life.1 These recommendations are also accepted and supported in Turkey.
Studies performed in developing countries have shown that the mortality risk among the infants who have not consumed breast milk, is 6 to 10 times higher than those who have consumed breast milk.2,3 Pneumonia and diarrhoea, which are two of the most frequent causes of under-five mortality rate, have higher rates and with more fatal prognosis in infants who have not taken breast milk.4,5 Regarding to the long term effects of breast milk, infants fed with breast milk have low risk of obesity and have higher scores of cognitive function.6
WHO and UNICEF recommend breastfeeding in the first hour after birth.7 Colostrum doesn't only protects the infant from infections, but also regulates the functions of gastrointestinal system of the baby.6 Additionally, it provides mother to get in contact with her baby as early as possible, which helps strengthen the bond between the mother and the baby.
Despite all the benefits of breastfeeding, the rate of exclusively breastfed infants between 0-6 months is around 36%.7 In 2012 World Health Assembly it has been declared as one of the six global targets to increase the rate of exclusive breastfeeding in the first six months up to at least 50% by year 2025. Actually, the rate of exclusive breastfeeding has been elevated from around 14% to 38% between the years 1985-1995, but it has later decreased in many regions of the world.8,9 Breastfeeding is common in Turkey, but exclusive breastfeeding
rate decreases from 68.9% to 23.6% in 4-6 months of age. Additionally, only 39% of infants are breastfed in the first hour after birth, and 27% of the infants aren't breastfed at all in the first 24 hours after birth.10 Incorrect knowledge and beliefs about breastfeeding, inadequate access to health services and professionals, and little support from health care providers could be the causes of such unfavourable results.
This study was performed to assess the knowledge level, attitudes and the own experiences of health care professionals about breast milk and breastfeeding in a metropolitan city in Turkey.
MATERIALS AND METHODS
This cross-sectional study has been performed between 1st July 2012-31st December 2013 in the hospitals, primary health care (PHC) centers in Ankara, the capital city of Turkey.
It has been planned to include health professionals who more frequently accessed women before and after delivery. Specialists and residents of gynecology-obstetrics, pediatrics, family medicine departments; general practitioners (GP), nurses and midwives were included in this study. 29 hospitals were selected among a total of 90 hospitals in Ankara. The number of delivery in each hospital was taken into consideration and "more than 500 deliveries in average monthly" was determined as selection criteria. The number of health professionals (gynecologists-obstetricians, pediatricians, family physicians, GPs, nurses and midwives) who work at those 29 hospitals and at the PHC centers in Ankara was obtained from the personel unit of Ministry of Health. According to data of Ministry of Health of Turkey, the scale of the study was determined as 4985 people. It was aimed to reach 10% of the universe but, by taking into consideration the missing data, approximately 750 people were selected to participate in the study. Inclusion criteria of the study were: to be a health care professional, to be actively working in those health care institutions and to fill in the questionnaire completely.
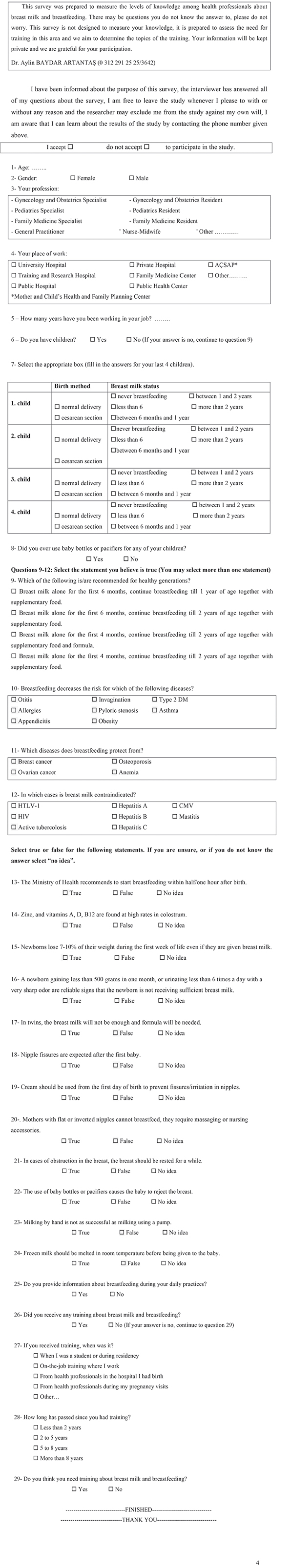
A questionnaire which consisted of 29 questions, was used for collecting data; 8 questions about sociodemographic features; 16 questions were concerning the level of knowledge about breast milk and breastfeeding, 1 question was about information given during daily practice and 4 questions were about training background on breastfeeding (Annex). The participants were categorized into three groups of having "poor", "average" and "good" level of knowledge. These groups were categorized according to the number of correct answers. The questionnaire were reviewed and finalized after a prestudy of 92 people. All of the questionnaires were filled in by the participants under direct observation at their workplaces.
Approval of Ethics Committee for Non-Drug Clinical Trials of Ataturk Training and Research Hospital was obtained.
Statistical analysis
Descriptive discrete numerical variables were shown as mean ± standard deviation or median (minimum-maximum). Categorical variables were shown as number of the participants and percentages. Categorical variables were evaluated by Pearson's Chi-Squared and Fisher's exact test. Results with a p <0.05 value were considered as statistically significant. Data were analysed using SPSS 11.5 Package Software for M.S. Windows.
RESULTS
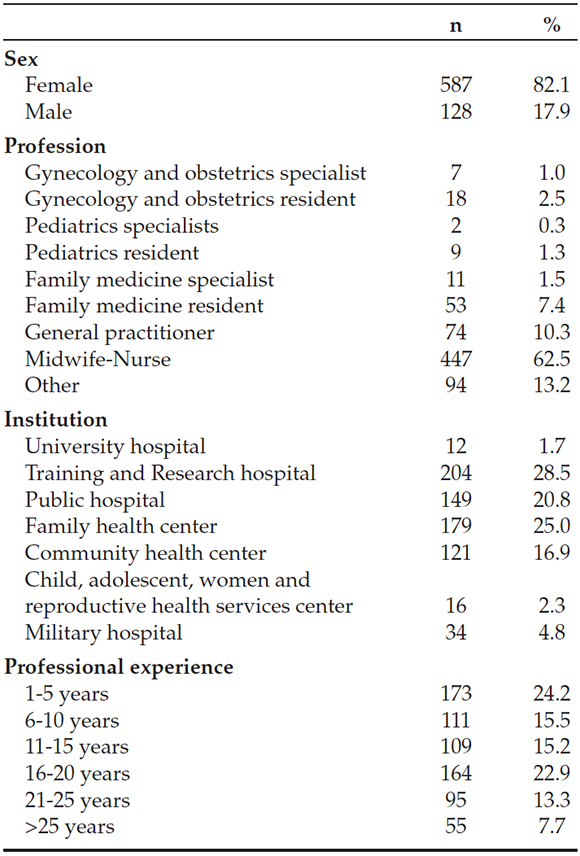
A total of 715 health professionals participated in the study. Age of the participants ranged between 17-62 years, the mean age was 35.6 ± 7.8 years. Other characteristics of the participants are presented in Table 1.
Table 1. Characteristics of the health care professionals participating in the study (n= 715)
Of those who participated, 70.1% (n= 501) had at least one child. The median duration for breastfeeding was one year. Besides, 3.2% (n= 16) of the participants who had children, had never breastfed their infant.
Most participants (94.9%) recommended exclusive breastfeeding for the first 6 months of age. For the period after the initiation of complementary food, 84.8% were suggesting the continuation of breastfeeding until 2nd year of age and 10.1% suggested breastfeeding until one year of age. Almost all participants (97.5%) suggested that the infant should be breastfed in the first 30 minutes after birth.
Of those who participated, 3.6% had an exact knowledge about the disease whose risks are decreased by breast milk in the neonatal period. Allergy and obesity were the two conditions about which participants had exact knowledge (79% and 75% respectively); 96.6% of the participants declared that breastfeeding had a preventive effect on breast cancer.
More than half of the participants inaccurately thought that some conditions related to breast and nipples were inconvenience for breastfeeding; 59.9% of the participants declared that breast milk wouldn't be enough for twin babies and formula shall be used.
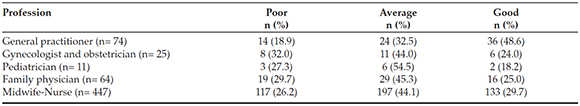
Generally, 28.4% of the participants had "poor", 43.1% "average" and 28.5% "good" knowledge level about breast milk and breastfeeding (Table 2).
Table 2. The knowledge level of health care professionals about breast milk and breastfeeding
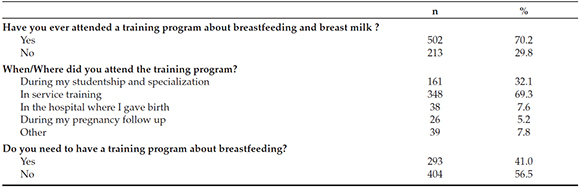
Of the professionals included in the study, 60.7% declared that they were actively providing guidance to mothers about the breast milk and breastfeeding on daily practice. It was found that 76.3% of nurses and midwives, 73% of GPs, 72% of gynecology-obstetricians, 63.6% of pediatricians, and 51.6% of family physicians had gotten a training about breastfeeding in any period of their professional life. General training background of participants are presented in Table 3.
Table 3. Participants' training background about breastfeeding and breast milk
DISCUSSION
Breast milk is the main source of food for infants as it contains important nutritional substances.11 Unfortunately, breast milk isn't provided adequately to many infants in most countries. Despite the recommendations about breastfeeding, apart from countries such as Germany, Norway and Scandinavia, the rate of breastfeeding is low worldwide12-14 The mother's decision isn't only factor in early termination of breastfeeding, nipple soreness, breast engorgement, infant's restlessness, doubts about the insufficiency of breast milk and beliefs regarding early termination in the society are the other factors. Lack of knowledge of health care providers in approaching the problems related to breastfeeding is also one of the main issues.15 This study which was designed to find the knowledge level of health professionals about breast milk and breastfeeding, is the first of its kind in Turkey.
Researches have found that the most frequent problem regarding to exclusive breastfeeding is maternal employment. The other factors include maternal or infants' health problems, different beliefs about child's nutrition and sociocultural factors.16 In a study, in Uganda, it has been found that the babies aren't well fed with neither breast milk nor complementary foods. The main factor of the problem was cited as lack of knowledge. Also strenuous working conditions at home or outside were found to be the main problem related to exclusive breastfeeding in the first 6 months. It has also been cited that health care providers have missed so many opportunities to pass on the correct information related to infant and child nutrition to the mothers.17
In studies performed in different countries on health care providers, it has been found that WHO recommendations regarding the duration of breastfeeding is less practiced and supported. 21% of participants in a study, performed on nurses and midwives, have supported that infants shall receive breast milk in the first 6 months, 33% have supported breastfeeding until 24 months of age.18 In different studies, 35% of participants supported exclusive breastfeeding in the first 6 months of life, 27.5% and 36% supported continuation of breastfeeding until 2nd year of age.19,20 Ramakrishnan et al. has found that 32.7% of mothers receiving service from obstetricians and 44.8% of mothers receiving care from pediatricians had a perception that their care giver recommended exclusive breastfeeding for the first month of life only.21 In our study it was found that most of the participants (94.9%) supported exclusive breastfeeding in the first 6 months of age and 84.8% supported continuation of breastfeeding until second year of age. Although most of the participants seemed to support the breastfeeding policies of WHO, it was found that only 7.6% had continued to breastfeed their babies until the second year of life. In a different study, it has been found that although physicians support breastfeeding, they couldn't remember the duration of time in which they had breastfed their own babies. And again, the main factor which prevented them from continuing breastfeeding was declared to be their jobs.22
There are many studies performed on physicians to evaluate their level of knowledge about breast milk and breastfeeding. In a study, the rate of correct answers to the questions related to the issue was 67.8% for pediatricians, 64.3% for family physicians (FP), 72.7% for pediatric residents and 66.8% for family medicine residents.23 In our study those who gave the most correct answers to the questions evaluating their knowledge about breast milk and breastfeeding, were the GPs and GPs were found to be the group that mostly provided breastfeeding guidance in daily practice. But unfortunately it is not possible to comment about the knowledge level of the other professionals especially pediatricians and obstetrician-gynecologists because of the limited participation. In different studies, the rate of breastfeeding guidance among physicians was found 20% and 39%.24,25 The result of a study in Australia has shown that during antenatal care, 32.6% of the patients have received guidance from gynecologist and obstetrician and 18.4% of patients has received guidance from FPs about breastfeeding.26 A study in Turkey, has cited that of those women with child, 62.2% has received information from a health professional.27 Of those who had participated in our study, 63.3% has declared that they were actively providing guidance during their daily practice. In another study performed in Turkey, the rate was found similar.28 Although the rate of providing guidance seems to be high in Turkey, the effectiveness of the guidance services shall be discussed. Especially, initiation of the guidance in antenatal period and continuing it after the childbirth may be effective on both initiation and continuation of breastfeeding. It has been stated in Cochrane review that professional guidance elongates both the overall duration of breastfeeding and the duration of exclusive breastfeeding. Social support shall be provided routinely in health care centers according to the necessities of the people living in the area. It has also been declared that face-to-face contacts are much more effective than phone-call contacts in providing the guidance.15
In Turkey, training programs about breastfeeding and breast milk are organized for health care professionals by the Ministry of Health. Because of the programs' limited number of human resources, it isn't received by adequate number of health professionals. In another study in Turkey, it has been found that 44% of health professionals have participated in such a training.29 In our study, this rate was found higher. A cause of the high rate can be the location in which our study was performed. Ankara is the capital city of the country, so it is easier to get access to a training program. As such, the location of the study can be mentioned as a limitation.
To promote a correct and adequate breastfeeding practice, current and accurate knowledge shall be transferred to the community firstly. After which the knowledge can be implemented into the practice. This cascade of the knowledge transferring and practical implementation needs a good service of guidance and community training. Thus, it is crucially important that health service providers which have the most frequent contact with the women in pre and postnatal period, shall receive a proper training about the issue. In a study performed in Ireland, it has been found that the number of health service providers who have received training about breastfeeding and breast milk, are inadequate and also health professionals are not able to provide guidance and support due to the lack of time. Thus, alternative methods such as "peer support" shall be spread among women.30 Physicians must try to use every opportunity to provide guidance and assistance to women and community. In this regard, PHC centres are excellent places where health care providers have good opportunity to provide the services. PHC centres are different from secondary and tertiary institutions in such that not only patients refer to them, but also healthy individuals apply to. In this study, it has been found that GPs, who are care providers in PHC centres, take more responsibility towards the issue, in comparison to other physicians. Nevertheless, some studies have shown different results. In Canada, half of the physicians thought that evaluation of breastfeeding isn't a responsibility of the physicians who work in the PHC centres.23
Most of the studies about this issue have been performed to evaluate the attitude and approach of certain groups of professionals like gynecologists-obstetricians, pediatricians, FPs, nurses and midwives. This can be a result of a worldwide acceptance that professionals in these groups are the ones who are most frequently in contact with women in pre and postnatal period.
Early initiation of breastfeeding, exclusive breastfeeding in the first 6 months of age, and continuation of breastfeeding together with complementary food until the second year of age are the goals regarding breastfeeding in most countries including Turkey. Training the community and increasing guidance services given by the health professionals, are obviously the main tools of reaching the goals.
In addition, barriers for breastfeeding should be investigated in every aspect. In Turkey the maternity leave involves only the period of 16 weeks (8 weeks before delivery, 8 weeks after delivery). There is an option to transfer 5 weeks after delivery.31 It means a mother is able to extend her maternity leave to only 3 months. So it's hard for a mother to breastfeed her baby exclusively during first 6 months.
Rights of employees in a country, including the leaves of those working in public or private institutions, are regulated by and in cooperation of many institutions such as ministries, social security or assistant institutes, and syndicates. As such these rights are directly related to the economic situation and level of development of the country. Nevertheless, this issue shall be taken into consideration with a common sense that breast milk is the main source of nutrition for a newborn and it can be provided only if mother is with her baby.
Although there are many limitations such as self reporting of attitudes about breastfeeding guidance, limited participation of pediatricians and obstetrician-gynecologists, this study gives a point of view about the status of health professionals about breastfeeding. In order to make contribution in reshaping the policies and plans regarding this issue, more comprehensive studies should be carried out and the barriers and facilitators about breastfeeding and breastfeeding guidance should be explicitly determined.
CONCLUSION
This study reflects the lack of knowledge about breastfeeding and breast milk among health professionals in a city of Turkey. The percentage of breastfeeding of health care professionals during the recommended period was very low.
2. Effect of breastfeeding on infant and childhood mortality due to infectious diseases in less developed countries: a pooled analysis. WHO Collaborative Study Team on the Role of Breastfeeding on the Prevention of Infant Mortality. Lancet 2000;355(9202):451-5. [ Links ]
3. Bahl R, Frost C, Kirkwood BR, Edmond K. et al. Infant feding patterns and risks of death and hospitalization in the first half of infancy: multicentre cohort study. Bull World Health Organ 2005;83(6):418-26. [ Links ]
4. De Zoysa I, Rea M, Martines J. Why promote breastfeeding in diarrhoeal disease control programmes? Health Policy Plan 1991;6(4):371-9. [ Links ]
5. Bachrach VR, Schwarz E, Bachrach LR. Breastfeeding and the risk of hospitalization for respiratory diseases in infancy: a meta-analysis. Arch Pediatr Adolesc Med 2003;157(3): 237-43. [ Links ]
6. World Health Organization. Media Centre. Infant and young childfeeding. [Acceso: 23 de agosto 2016] Disponible en: http://www.who.int/mediacentre/factsheets/fs342/en/
7. Samur G. Anne sutu. Ankara: Klasmat Press; 2008.P.9. [ Links ]
8. World Health Organization. Nutrition. WHA65/6. Comprehensive implementation plan on maternal, infant and young child nutrition. [Acceso: 28 de junio de 2014] Disponible en: http://www.who.int/nutrition/topics/wha_65_6/en/
9. UNICEF. Progress for Children. A World Fit for Children Statistical Review. New York, USA: UNICEF, 2007. [Acceso: 23 de agosto 2016] Disponible en: http://www.unicef.org/publications/files/Progress_for_Children_No_6_revised.pdf
10. Children's and women's nutritional status. En: Turkey Demographic and Health Survey 2008. Ankara, Turkey: Hacettepe University Institute of Population Studies, 2009:177-86. [Acceso: 23 de agosto 2016] Disponible en: http://www.hips.hacettepe.edu.tr/eng/tdhs08/TDHS-2008_Main_Report.pdf
11. Cope MB, Allison DB. Critical review of the World Health Organization's (WHO) 2007 report on 'evidence of the long term effects of breastfeeding: systematic reviews and metaanalysis' with respect to obesity. Obes Rev 2008;9(6):594-605. [ Links ]
12. Cattaneo A, Yngve A, Koletzko G, Guzman LR. Protection, promotion and support of breastfeeding in Europe: current situation. Public Health Nutr 2005;8(1):31-46. [ Links ]
13. Cattaneo A. Protection, promotion and support of breastfeeding in Europe: a blueprint for action. Luxembourg: European Commission, Directorate Public Health and Risk Assesstment, 2004. [Acceso: 23 de agosto 2016] Disponible en: http://ec.europa.eu/health/ph_projects/2002/promotion/fp_promotion_2002_frep_18_en.pdf
14. Nicoll A, Thayaparan B, Newell ML, Rundall P. Breast feeding policy, promotion and practice in Europe. Resultsof a survey with non-governmental organizations. J Nutr Environ Med 2002;12(3):255-64. [ Links ]
15. Renfrew MJ, McCormick FM, Wade A, Quinn B. et al. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst Rev 2012;(5):CD001141. [ Links ]
16. Balogun OO, Dagvadorj A, Anigo KM, Ota E, et al. Factors influencing breastfeeding exclusivity during the first 6 months of life in developing countries: a quantitative and qualitative systematic review. Matern Child Nutr 2015;11(4):433-51. [ Links ]
17. Nankumbi J, Muliira JK. Barriers to Infant and Child-feeding Practices: A Qualitative Study of Primary Care givers in Rural Uganda. J Health Popul Nutr 2015;33(1):106-16. [ Links ]
18. Dachew BA, Bifftu BB. Breastfeeding practice and associated factors among female nurses and midwives at North Gondar Zone, Northwest Ethiopia: a crosssectional institution based study. Int Breastfeed J 2014;9:11. [ Links ]
19. Leviniene G, Petrauskiene A, Tamilevicience E, Kudzyte J, et al. The evaluation of knowledge and activities of primary health care professionals on promoting breastfeeding. Medicina (Kaunas) 2009;45(3):238-47. [ Links ]
20. Okolo SN, Ogbonna C. Knowledge, attitude and practice of health workers in keffi local government hospitals regarding Baby-friendly hospital initiative (BFHI) practices. Eur J Clin Nutr 2002;56(2):438-41. [ Links ]
21. Ramakrishnan R, Oberg CN,Kirby RS. The Association between Maternal Perception of Obstetric and Pediatric Care Providers' Attitudes and Exclusive Breastfeeding Outcomes. J Hum Lact 2014;30(1):80-7. [ Links ]
22. Anchondo I, Berkeley L, Mulla ZD, Byrd T, et al. Pediatricians', Obstetricians', Gynecologists', and Family Medicine Physicians' Experiences with and Attitudes about Breast-Feeding. South Med J 2012;105(5):243-8. [ Links ]
23. Pound CM, Williams K, Grenon R, Aglipay M, et al. Breastfeeding Knowledge, Confidence, Beliefs, and Attitudes of Canadian Physicians. J Hum Lact 2014;11;30(3):298-309. [ Links ]
24. Nakar S, Peretz O, Hoffman R, Grossman Z, et al. Attitudes and knowledge on breastfeeding among pediatricians, family physicians, and gynecologists in Israel. Acta Pædiatr 2007;96(6):848-51. [ Links ]
25. DiGirolamo AM, Grummer-Strawn LM, Fein SB. Do Perceived Attitudes of Physicians and Hospital Staff Affect Breastfeeding Decisions? Birth 2003;30(2):94-100. [ Links ]
26. Walsh AD, Pincombe J, Henderson A. An Examination of Maternity Staff Attitudes Towards. Implementing Baby Friendly Health Initiative (BFHI) Accreditation in Australia. Matern Child Health J 2011;15(5):597-609. [ Links ]
27. Ünsal H, Atlıhan F, Özkan H, Targan X, et al. Toplumda anne sutu verme e ilimi ve buna etki eden faktorler. Qocuk Sa li i ve Hastaliklari Dergisi 2005;48:226-33.
28. Kaya D, ve Pirinçci E. 0-24 Aylık Çocuğu Olan Annelerin Anne Sütü Emzirme ve İle İlgili Bilgi ve Uygulamaları. TAF Prev Med Bull 2009;8(6):479-84.
29. Gonener HD, Balat A, Aydin N. Cocuk Sağlığı İle İlgili Alanlarda Calışmayan Hekim ve Hemşirelerin Anne Sutune Yonelik Bilgi Durumları. ÜFN Hem Derg 2010;18 (3):128-35.
30. Whelan B, Kearney JM. Breast-feeding support in Ireland: a qualitative study of health-careprofessionals' and women's views. Public Health Nutr 2015;18(12):2274-82. [ Links ]











 text in
text in 


