Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Archivos argentinos de pediatría
versión impresa ISSN 0325-0075versión On-line ISSN 1668-3501
Arch. argent. pediatr. vol.116 no.2 Buenos Aires abr. 2018
http://dx.doi.org/10.5546/aap.2018.93
ORIGINAL ARTICLE
http://dx.doi.org/10.5546/aap.2018.eng.93
Impact of a program aimed at reducing catheter-related infections implemented in nine pediatric intensive care units in Argentina
Ana M. Lenz, M.D.a, Elena Andion, B.S.a, Silvina Ruvinsky, M.D.a, Clarisa Aguirre, M.D.b, Julieta Álvarez Parma, M.D.c, Facundo Jorro, M.D.d, Gabriela López Cruz, M.D.e, Martín Pascutto, M.D.a, Matías Penazzi, M.D.f, Silvia Santos, M.D.g, Marcela Zuázaga, M.D.a, Norma Aquino, B.S.a, Juan C. Vassallo, M.D.a, Guillermo Moreno, M.D.a, Ricardo Magliola, M.D.a, Aldo Haimovich, M.D.a, Luis Landry, M.D.a and Rosa Bologna, M.D.a
a. Hospital de Pediatría "J. P. Garrahan," Autonomous City of Buenos Aires.
b. Hospital Juan Pablo II, Corrientes.
c. Hospital Interzonal de Ninos "Eva Perón," Catamarca.
d. Hospital de Ninos "Pedro de Elizalde", Autonomous City of Buenos Aires.
e. Provincial Center of Pediatric Health, "Eva Perón," Santiago del Estero.
f. Hospital de Ninos de San Justo, Province of Buenos Aires.
g. Hospital Regional de Agudos "Eva Perón" (formerly Castex), San Martín, Province of Buenos Aires.
E-mail address: Ana M. Lenz, M.D.: lenzanamiriam@gmail.com
Funding: This study was partially funded through the Ramón Carrillo-Arturo Onativia scholarship (2011).
Conflict of interest: None.
Received: 1-31-2017
Accepted: 8-22-2017
ABSTRACT
Catheter-related infections (CRIs) cause a high level of morbidity and mortality with the increasing use of hospital resources.
Objective. To describe the outcomes of a program implemented to reduce the rate of CRIs in pediatric intensive care units in Argentina.
Population and methods. Collaborative, multi center, clinical-epidemiological, quasiexperimental, before-and-after intervention study. Children who had a central venous catheter during hospitalization in 9 pediatric intensive care units in the Autonomous City of Buenos Aires, Greater Buenos Aires, and other provinces between June 2011 and April 2012 were included. A bundle of measures based on health care staff training on catheter insertion, hand hygiene, and checklists was put into practice and implemented measures were monitored. The number and annual rate of CRIs and the rate of central venous catheter use before and after the program implementation were compared (Stata 8.0).
Results. The total number of CRIs was 117 and 74 before and after the intervention, respectively. The rate of CRIs was 8.6/1000 days of central venous catheter use and 5.8/1000 days before and after the intervention, respectively; RR: 0.82 (95% confidence interval: 0.68-0.98), p= 0.015. The rate of central venous catheter use decreased from 54% to 49%, a non-significant difference.
Conclusions. The program achieved a significant reduction in CRI rates. Based on the program, CRI surveillance was implemented in all participating pediatric intensive care units. Training and continuous surveillance are necessary to maintain and improve the outcomes accomplished with the program.
Key words: Catheter-related infections; Central venous catheters; Pediatric intensive care units.
INTRODUCTION
Intravascular catheters are safe devices routinely used in critical patients because they enable the administration of inotropes, highdose drugs, and blood products, and help with hemodynamic monitoring. Unfortunately, their use is not without risks, especially in young children, who usually meet all risk factor criteria. Bloodstream infections associated with central venous catheters (CVCs) are a significant health problem; they account for an increased morbidity and mortality in the pediatric intensive care unit, extending the length of stay from 10 to 40 days and, thus, health care-related costs. CVC use is one of the most common causes of hospital-acquired bacteremia, which ranges from 4 to 8 infections per 1000 catheter days or from 1% to 13%, with a higher rate of infection in the most commonly used sites.1-3 Catheter-related infections (CRIs) should be considered a patients' safety concern. The systematic implementation of a series of interventions as part of a Program for the Prevention of Catheter-Related Infections4,5 in pediatric intensive care units (PICUs) (MultiCOMBO) has therefore become a strategy aimed at improving health care quality.6 These "MultiCOMBO" programs are bundles of measures that are implemented together in order to accomplish the intended outcome, because it has been observed that interventions with a high level of impact and evidence that have been implemented separately have failed to reduce the rate of infections.7 This systematic intervention has been successfully put into practice in many hospitals worldwide.6,8
The proposal is to implement a multidisciplinary bundle of simple measures with a high level of evidence9 and with recognized impact to effectively reduce CRIs. Significant among these measures are health care staff training10 and the introduction of new monitoring and information feedback techniques.11-13
In the 2008-2009 period, the incidence of CRIs at the PICUs of Hospital Garrahan ranged from 9 to 12 per 1000 CVC days.14,15 The Multidisciplinary Program for the Prevention of Catheter-Related Infections was first implemented in July 2010 and resulted in a reduction of the CRI rate to 5.7 per 1000 CVC days.16 Considering that this problem is common to all PICUs, it was proposed to extend the program to other PICUs across Argentina to disseminate health care quality improvement processes and optimize health care provision.
The objective of this study was to compare the incidence of CRIs before and after the implementation of a bundle of measures designed to this end at each participating PICU.
PATIENTS AND METHODS
This was a multicenter study with a before-and-after, quasi-experimental design that assessed the impact on the incidence of CRIs before and after the implementation of a bundle of measures aimed at reducing CRIs.
Argentina has 132 PICUs, 24% of which are located in public hospitals. PICUs were selected from public hospitals based on their prior participation in a quality improvement program that had been implemented within 3 years earlier and their compliance with implementation and recording feasibility requirements, as well as on the approval from jurisdictional authorities and health care providers responsible for the unit.
A total of 9 PICUs from 7 hospitals participated: Hospital de Pediatría "Juan P. Garrahan," Hospital General de Ninos "Pedro de Elizalde," Hospital de Ninos de San Justo, Hospital Regional de Agudos "Eva Perón" (formerly Castex), Hospital Interzonal de Ninos "Eva Perón" from Catamarca, Hospital Pediátrico "Juan Pablo II" from Corrientes, and Provincial Center of Pediatric Health (Centro Provincial de Salud Infantil, CEPSI) "Eva Perón" from Santiago del Estero. The protocol was approved by the Research Committee of Hospital Garrahan (coordinating site for the multicenter study) and the research committees of each participating hospital. The informed consent was not requested because interventions done on patients are not different from everyday practice.
All children who had a CVC during hospitalization in the PICU of a participating hospital between June 1st, 2011 and April 30th, 2012 were included. The following outcome measures were recorded: CRI rate per 1000 CVC days as defined by the epidemiological surveillance of the Centers for Disease Control and Prevention (CDC) (see definitions in Annex 1), CVC use rate, adherence to hand washing (Annex 2), and adherence to CVC insertion control (Annex 3). To assess the program's effectiveness, the preintervention period was defined as that between August 1st, 2010 and May 31st, 2011 and the postintervention period was that between June 1st, 2011 and March 31st, 2012.
Monthly workshops were carried out on hand hygiene and the implementation of the five moments at the point of patient care and on the prevention of hospital-acquired infections inside the PICU. Progress and outcomes were shared with all health care staff members on a monthly basis. Through personal meetings with the execution team and virtual meetings with the participating sites, potential solutions were discussed and agreed upon and doubts were cleared as they appeared during the program implementation. The referral and counter-referral system currently valid at Hospital Garrahan was used in the framework of the Subprogram for Teaching-Health Care Collaboration with the PICUs of CEPSI from Santiago del Estero and the "Eva Perón" hospital from Catamarca.
Annex 4 describes the program and the implementation stages at the different participating sites.
Statistical analysis
In this study, dependent outcome measures were identified as indicators of interventions (CVC use rate, CRI rate per 1000 catheter days, percentage of CRIs, absolute number of CRIs, percentage of adherence to measures [globally or disaggregated by bundle]), considering the intervention in the bundle of measures as a whole and comparing selected indicators before and after the intervention. Continuous outcome measures were summarized using position and dispersion measures as per distribution; categorical data were described using frequency tables and charts. The bivariate analysis of outcome measures was done using the t test, the Wilcoxon test or the χ2 test, as applicable. The significance level was established at < 0.05 and the statistical package for data processing was Stata 8.0.
RESULTS
Table 1 details the data collected from each participating PICU before the intervention. Table 2 shows the impact of the program in the reduction of the number of CVC-related infections, the rate of catheter use, and the rate of CVC-related infections. At the PICUs from the hospitals that started their first year of the program, a significant reduction was observed in the rate of CRIs, together with a reduction in the total number of CRIs compared to the year prior the program implementation. This was not observed at the 3 PICUs from the coordinating site that had started the program 1 year before, where rates remained stable. The total number of CRIs was 117 and 74 before and after the intervention, respectively (see Table 2), and the total rate of CRIs was 8.6 per 1000 CVC days and 5.78 per 1000 CVC days before and after the intervention, respectively; RR: 0.82 (95% confidence interval [CI]: 0.68-0.98), p= 0.015. The rate of CVC use decreased from 54% to 49%. Only 5 PICUs reported data on adherence to hand hygiene, so the analysis of this outcome measure was not considered useful.
Table 1. Baseline characteristics of each participating pediatric intensive care unit in the pre-intervention period
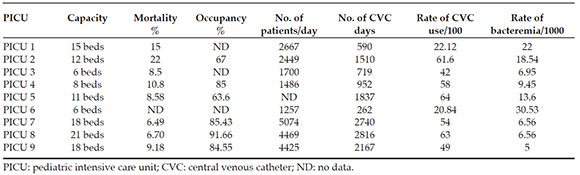
Table 2. Analysis of program impact before and after the intervention

DISCUSSION
The importance of this multicenter study was that it demonstrated that the implementation of programs aimed at reducing the rate of hospital-acquired infections accomplished significant outcomes based on simple measures available for health care staff. The foundation of these outcomes lies in the extent of involvement of the institution to carry out the program, ongoing education, a change in behavior, and awareness that it is not necessary to have better technology to achieve successful results. It is worth noting that all staff members involved in patient care participated in the program, including technicians and cleaning staff, not only physicians and nurses. In addition, it is necessary to strictly monitor the outcomes using statistics, as well as to compare them over time within the hospital and, in turn, against national and international epidemiological surveillance organizations.15,17
Health care staff training on the prevention of hospital-acquired infections started gaining importance more than a decade ago. Coopersmith et al., in 2002,10 achieved a 66% reduction in CRIs (from 10.8 to 3.7); their study included a pre- and post-test for nurses from an adult ICU on infection prevention knowledge; then, they were given a 10-page document on the topic and received training at the ICU. Berenholtz et al., in 2004,7 complemented training with a catheter insertion checklist, and authorized nurses to interrupt the procedure in case of antisepsis breakdown and to do a daily assessment of patient's ongoing CVC requirement. This group reduced the rate of infections from 11.5/1000 to 0/1000 catheter days, thus demonstrating the great impact of implementing several evidence-based measures at the same time. In this study, Berenholtz included a control group at a different surgical care unit, where the only intervention was training health care staff without any other control measure. The rate of infections was reduced by 75%, compared to the group that introduced several measures at the same time, which achieve a 100% reduction.7 These bundles of measures were replicated in many sites with adequate outcomes and achieved a reduction in hospital-acquired infections.18,19
Most sites in the program lacked an active surveillance system to record hospital-acquired infections at the different PICUs, so staff was trained on how to record data and prepare statistics. The implementation of hand washing and catheter insertion checklists basically had an educational impact and allowed to provide training on the good practices for hospital-acquired infections.
One of the most important contributions of this program was starting an active hospital-acquired infection surveillance system, initially for CVC-related bacteremias, one of the most common diseases in the pediatric population.
In the post-intervention period, it was observed that the 6 sites that started their first year in the program achieved a reduction in the number of CRIs, together with a reduction in the rate of CVC use, which meant that, probably, at this point, some sites accomplished a greater level of monitoring of patient CVC requirement beyond what was strictly necessary. In addition, very high reductions were observed in the rate of CRIs. In some cases, such reduction was statistically significant; in others, the significance showed a trend but as a consequence of a reduction in CVC days, the numerator was probably overestimated and thus, the result of this rate did not achieve the expected statistical significance.
In the 3 PICUs from the coordinating site, a reduction of approximately 50% had been observed in the first year of the program (2010).14,16 This study (2011) did not find a reduction from baseline but stable rates. However, it is worth considering that the study corresponded to the second year of the program in that site so there was probably resistance against implemented measures or a lower level of adherence by health care staff. It has been described that when surveillance and strategies to maintain such measures reduce, adherence decreases and the rate of infections rises again.20-22 The high staff turnover, frequent in critical care units, adds to the difficulties of this collective challenge and calls for searching new ongoing encouraging strategies in order to achieve a greater level of adherence. The main change consists in accomplishing changes in the culture of health care staff on the importance of hand hygiene and compliance with all program moments by all members so as to achieve a sustained reduction in hospital-acquired infections and continue reducing current CRI rates.
One of the limitations of this study was that it was not a controlled clinical trial but had a before-and-after design.
It has been considered that the evidence of the program outcomes is sufficient to continue its implementation and replication in the different PlCUs of Argentina.
CONCLUSION
The implementation of this program accomplished a statistically significant reduction in the rate of CVC-related bacteremia among children hospitalized in the PICU.
ANNEX 1
Definitions

ANNEX 2
Observation form of hand hygiene.
Implementation of the five moments at the point of patient care. Checklist

ANNEX 3
CVC bundle of measures. CVC insertion checklist

ANNEX 4
Activities done during the program













 texto en
texto en 
