Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Archivos argentinos de pediatría
Print version ISSN 0325-0075On-line version ISSN 1668-3501
Arch. argent. pediatr. vol.116 no.2 Buenos Aires Apr. 2018
http://dx.doi.org/10.5546/aap.2018.e315
CASE REPORT
http://dx.doi.org/10.5546/aap.2018.eng.e315
Massive hemorrhage: a late complication of replacement percutaneous endoscopic gastrostomy: case report
Tamer Sekmenli, M.D., Assistant Professora, Metin Gunduz, M.D., Assistant Professora, Hikmet Akbulut, M.D., Assistant Doctorb, H. Haldun Emiroglu, M.D., Associate Professorc, Mustafa Koplay, M.D., Associate Professord and Ilhan Ciftci, M.D. Associate Professora
a. Selcuk University Faculty of Medicine Department of Pediatric Surgery.
b. Selcuk University School of Medicine Department of Pediatric.
c. Selcuk University School of Medicine Department of Pediatric Gastroenterology.
d. Selcuk University School of Medicine Department of Radiology. Turkey.
E-mail address: Tamer Sekmenli, M.D.: dr_sekmenli@hotmail.com
Funding: None.
Conflict of interest: None.
Received: 7-1-2017
Accepted: 9-19-2017
ABSTRACT
Percutaneous endoscopic gastrostomy (PEG) is used as an alternative to enteral/nasoenteral feeding in situations where long-term oral feeding is ineffective or not tolerated. It is mostly preferred in patients with neurological conditions and also to support nutrition in patients with congenital heart diseases, cystic fibrosis, inflammatory bowel disease, and various oropharyngeal diseases. Although it is easily applicable compared to many invasive procedures, it has complications ranging from wound infection to death.
PEG requires experienced medical personnel, appropriate prophylactic antibiotics and exhaustive information to the patients or their families about the procedure and subsequent care. We present a rare but important complication during the replacement of the gastrostomy tube subsequent to the "cut and push" method. The bumper portions, which should move to the distal end of the stomach, moved upwards to the proximal esophagus, caused a deep ulcer in the esophageal mucosa and a massive hemorrhage.
Key words: Percutaneous endoscopic gastrostomy; Gastrointestinal hemorrage; Cut and push technique.
INTRODUCTION
Patients with deficient or impaired nutrition are more prone to deterioration of immune system, wound healing, and psychological status.1 Starting enteral feeding in due time has the advantages of reducing mucosal atrophy, protecting barrier function of the intestine, and decreasing intestinal bacterial translocation.2 Therefore, when oral feeding is insufficient for prolonged periods, 4-8 weeks, enterostomy have utmost importance for nutritional support of the patients with a functional gastrointestinal system. Amongst enterostomy applications, gastrostomy is the most appropriate one for the digestive physiology and can be inserted under percutaneous endoscopy, surgical or interventional radiology methods.3
Percutaneous endoscopic gastrostomy (PEG), first described by Gauderer et al., in the 1980's, is a method used when the gastrointestinal system is intact; however, oral feeding is not possible for an extended period.4 Although it is commonly used in children with neurological sequelae, it is also preferred in metabolic and oncological diseases, and anatomical and functional disorders of the upper digestive system.5 As in any invasive procedure, complications can emerge during and after the PEG procedure. These include peristomal infection and leakage, peritonitis, pneumoperitoneum, hemorrhage, tube obstruction and fistulization. PEG, easily inserted by experienced medical personnel, has averted surgical gastrostomy.6
Even though commonly preferred in patients with neurological problems, it can be used to support nutrition in patients with congenital heart diseases, cystic fibrosis, inflammatory bowel diseases, and various oropharyngeal diseases. PEG is a feasible and minimal invasive technique, however there are some inherent minor and major complication risks ranging from wound infection to death.7 In order to avoid those complications, PEG requires experienced medical personnel, appropriate prophylactic antibiotics and exhaustive information to the patients or their families about the procedure and subsequent care.
We present a rare but important complication occurring during the replacement of the gastrostomy tube subsequent to the "cut and push" method.8-10 The bumper portions, which should move to the distal end of the stomach, moved upwards to the proximal esophagus, penetrated to esophageal mucosa, caused a deep ulcer and subsequent massive hemorrhage.
CASE
A three and half years old boy with gastrostomy was admitted to intensive care unit (ICU) with respiratory failure following pulmonary aspiration during administration of his medications, and subsequent respiratory arrest. He was one of the triplets born with cesarean section with 24 weeks gestational age and 500 grams birth weight. He was under follow-up with cerebral palsy, epilepsy, gastroesophageal reflux, and bronchopulmonary dysplasia diagnoses. By 8 months of age first PEG procedure was applied, and two months before current admission the PEG tube was replaced by "cut and push" technique, and had been fed through PEG tube without any problem.
The general condition of the patient at ICU admission was fair, and on physical examination the patient had 36.5 C° body temperature, 20 per min respiratory rate, 110 per min heart rate, 10 kg (25thP) body weight, 84 cm (25thP) body height, and 41.5 cm (25thP) head circumference. Auscultation of the thorax revealed course lung sounds. There was a PEG tube placed on the left side of the epigastrium and any disruption around the stoma was observed. Abdomen was soft and non-tender on palpation. Neurological examination of the patient revealed increased tonus of upper and lower extremities along with positive Babinski and clonus. As soon as the patient was stabilized, intravenous fluid support and ampicillin- sulbactam treatment was started with the diagnosis of aspiration pneumonia.
When the general condition of the patient improved, and respiratory complaints decreased, enteral feeding started through PEG tube, however, feeding was stopped following a projectile bloody vomiting. A nasogastric tube was inserted, saline solution irrigation was administered via gastrostomy tube, and ranitidine treatment was started. Subsequent free nasogastric and PEG tube drainages were clear. Since the control hemoglobin value was 7 g/dl, erythrocyte suspension (10 mL/kg) was transfused. Ultrasonography guided central venous catheter was inserted through right subclavian vein, and during the X-Ray control of catheter placement, a mass-like lesion at the level of proximal esophagus was noticed. Hemorrhage was attributed to this mass; subsequent thorax computed tomography revealed an embedded foreign body located at the 1/3 proximal part of the esophagus without any fistulization with the main vessels. Subsequently, upper gastrointestinal endoscopy was performed; the foreign body was composed of bump portions of previous PEG tube. Endoscopic removal of the foreign body was achieved without any complications. (Figure 1,2a.b). After the procedure the integrity of the esophagus was controlled with water-soluble contrast enhanced upper gastrointestinal X-Ray study, and no leakage was observed. However patient had three more intermittent moderate hemorrhage episodes, which were stabilized with conservative medical support. Finally, patient was lost following an abundant hemorrhagic episode.
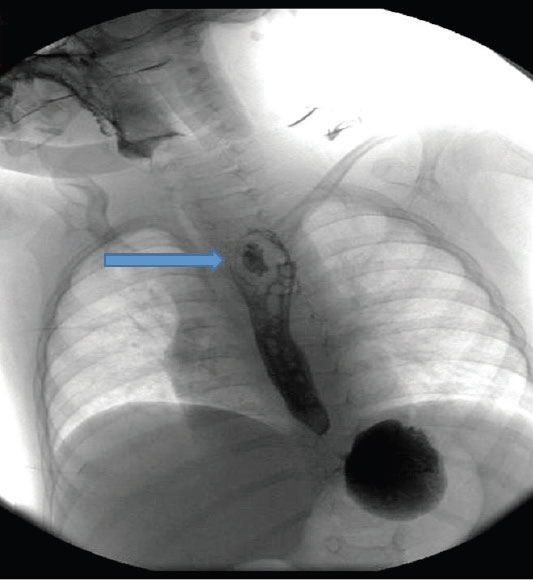
Figure 1. Appearance of foreign body, contrast-enhanced
esophagography

Figure 2. Foreign body removed from the esophagus
DISCUSSION
Balanced and adequate diet beginning from the birth is necessary for a healthy life.
Inadequate nutrition leads to various diseases and disease related complications. Particularly in children, besides failure to thrive, neuromotor development is also impaired Hence, in order to prevent malnutrition if oral feeding is insufficient or inadequate, enteral/parenteral methods are used. Since it is easier to apply, cost-effective, physiological, and preserves intestinal flora and mucosa, enteral feeding is the preferred way of nutrition.6
Nasogastric, nasoduodenal, or nasojejunal methods can be employed for enteral feeding. However, in patients with long-term enteral nutritional requirements those may have many disadvantages such as nasopharyngeal disturbances and tissue erosions, upper respiratory tract infections, esophagitis, gastric erosion and ulceration, and esophageal variceal rupture.11 Therefore, gastrostomy is considered as an option when oral feeding is not possible for prolonged periods longer than 4 - 8 weeks. Today, PEG is widely performed by pediatric surgeons and gastroenterologists as an easily applicable, safe and minimal invasive procedure.4,12 When performed by experienced medical personnel, PEG has low complication rates, and is a convenient procedure both for the patients and their caregivers. PEG is most frequently applied for the patients with neurological disorders, followed by metabolic diseases, congenital heart diseases, cystic fibrosis, oncologic diseases, and various oropharyngeal disorders, where oral feeding is inadequate.13
Although PEG is widely accepted as a simple and reliable method, complications may emerge during and after the procedure.6 These complications are classified as major, and minor complications. The major complications of PEG include gastric perforation, gastric hemorrhage and hematoma, fistulization, aspiration pneumonia, subcutaneous abscess, buried boomer syndrome, necrotizing fasciitis, acute pancreatitis, whereas minor complications are wound infections, peristomal leakage, hemorrhage, pneumoperitoneum, ulceration, tube obstruction, and gastric outlet obstruction.4-6,13 The wound infection is the most frequent complication, when antisepsis, and antibio-prophylaxis are neglected. In a series of Gauderer et al. 8% of major complications was encountered in a total of 224 PEG procedures.5
During PEG, pull or push techniques are used for placement, depending on the medical staff's choice, and there is no significant difference between both techniques in terms of applicability and complication rates.11 However, as demonstrated in our case, the distal portion of the PEG tube may move to esophagus with the use of "cut and push" technique in neurologically disabled patients probably due to fixed limb posture as contrary to general expectation that the bumpers of the PEG tube moves to distal stomach. Regardless of which method is used, regular patient follow-up, especially enabling PEG bumpers passage, and if necessary radiologic imaging of disposed bumper presence is necessary to determine and prevent complications. PEG tubes should be anti-allergic and flexible. Therefore, silicone or polyurethane tubes are more suitable than polyvinyl tubes.11 Although the PEG tube in our patient was made of silicone material, long term stay in the esophagus resulted in embedding and tissue damage. Since feeding the patient though a replaced PEG tube do not compromise regular enteral feeding, presence of a foreign body in the esophagus may be obscured, and may not be noticed until the tissue damage and hemorrhage has occurred. Therefore imaging studies should be utilized during the replacement of PEG tubes.
In the present case, after the replacement of the PEG catheter by the cut-and-push method, the remaining bumpers moved to esophagus, embedded in the mucosa, and caused erosion, ulcer, and massive hemorrhage. Although PEG is an easy and safe method, post- procedure radiologic or endoscopic imaging is crucial in order to reduce the risk of such rare complications presented in this case.











 text in
text in 
