Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO  uBio
uBio
Compartir
Revista argentina de microbiología
versión impresa ISSN 0325-7541versión On-line ISSN 1851-7617
Rev. argent. microbiol. vol.50 no.3 Ciudad Autónoma de Buenos Aires set. 2018
http://dx.doi.org/10.1016/j.ram.2017.10.006
SPECIAL ARTICLE
https://doi.org/10.1016/j.ram.2017.10.006
Carbapenemases in Acinetobacter baumannii. Review of their dissemination in Latin America
Carbapenemasas en Acinetobacter baumannii. Revisión de su diseminación en América Latina
Carlos Hernán Rodrígueza,*, Marcela Nastroa, Angela Famigliettia
a Hospital de Clínicas José de San Martín, Departamento de Bioquímica Clínica, Córdoba 2351, 1120 Buenos Aires, Argentina
Received 5 June 2017; accepted 27 October 2017
Available online 13 March 2018
*Corresponding author.
E-mail address: carlos-hemanrodriguez@hotmail.com (C.H. Rodríguez).
0325-7541/© 2017 Asociacion Argentina de Microbiología. Published by Elsevier Espana, S.L.U. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abstract
Carbapenem resistance in gram-negative bacteria by production of carbapenemases is one of the most challenging issues regarding healthcare worldwide. We review the epidemiology and prevalence of carbapenemases in carbapenem-resistant Acinetobacter baumannii isolates from Latin American countries. High resistance rates to antimicrobial agents, particularly to carbapenems, are observed in this region. OXA-23 is the most widely disseminated class D-carbapenemase; it is present in all the countries of the region and is frequently associated to endemic clones CC113/CC79, CC104/CC15, CC110/ST25 and CC109/CC1. The emergence of OXA-72 and NDM-1 represents a novel finding which is observed simultaneously and without clonal relatedness in different countries, some of which are distant from one another, whereas OXA-143 is only present in Brazil. Further collaborative intraregional studies would provide a better understanding of these issues in most of the countries and thus, policies to control the spread of these isolates could be implemented.
KEYWORDS
Acinetobacter baumannii; Latin America; Carbapenemases; Carbapenemhydrolyzing class D β-lactamases; NDM-1
Resumen
En bacilos gram negativos, la resistencia a carbapenemes por producción de carbapenemasas es uno de los mayores problemas en la atención de la salud a nivel mundial. Reseñamos en este artículo la epidemiologia y la prevalencia de las carbapenemasas descritas en aislamientos de Acinetobacter baumannii recuperados en América Latina. En esta región se ha observado un alto porcentaje de resistencia a los antimicrobianos, particularmente a los carbapenemes. La carbapenemasa más frecuentemente descrita es OXA-23, que ha sido recuperada en todos los países de la región y fue asociada a los clones endémicos CC113/CC79, CC104/CC15, CC110/ST25 y CC109/CC1. La emergencia de OXA-72 y NDM-1 representa un nuevo hallazgo en varios países, algunos de los cuales se encuentran muy distantes entre sí. Por el momento, OXA-143 solo se recuperó de aislamientos obtenidos en Brasil. Serían necesarios estudios colaborativos dentro de la región para lograr una mejor comprensión de la resistencia a carbapenemes en Acinetobacter baumannii, a fin de poder instaurar medidas de control que eviten una mayor diseminación de esta bacteria.
PALABRAS CLAVE
Acinetobacter baumannii; América Latina; Carbapenemasas;Clase D carbapenemasas; NDM-1
Introduction
The genus Acinetobacter, as currently defined, comprises gram-negative, strictly aerobic, nonfermenting, nonfastidious, nonmotile, catalase-positive, oxidase-negative bacteria with a DNA G+C content of 39-47%24.
Implementation of molecular techniques and mass spectrometry such as matrix-assisted laser desorption ionization-time and flight mass spectrometry (MALDI-TOF MS) in clinical microbiology laboratories has greatly improved the identification of Acinetobacter species.Acinetobacter baumannii is the most important in the clinical context. This is the genospecies which is most frequently associated with hospital outbreaks24. The ability to survive on inanimate surfaces and resistance to disinfectants or antimicrobials are crucial to this behavior24.
Carbapenems are currently the antibiotics of choice against multidrug-resistant Acinetobacter infections. However, carbapenem-resistance (CR) is increasingly being reported, leaving few therapeutic options available24,37,38.
The aim of this review is to analyze the prevalence and molecular epidemiology of carbapenem-resistant A. baumannii (CR-Ab) isolates in Latin American countries.
Literature associated with CR-Ab in Latin America (LA) was included. The articles in English and Spanish language were accessed through PubMed and Scientific Electronic Library Online (SciELO). Pan American Health Organization (PAHO) documents were also consulted19-23. It is important to mention that a heterogeneous distribution of molecular epidemiology studies performed in the region was noticed; although 60% of the countries in LA have presented data, more than 50% of these correspond to Brazil and Argentina.
Prevalence of carbapenem-resistant A. baumannii
Rates of carbapenem resistance in LA appear to be among the highest in the world. A wide range of resistance has been reported among the different countries (1-90%), the lowest values belong to Central America and the highest ones to some studies in Argentina and Brazil12. In addition, reports of the Latin American Antimicrobial Resistance Surveillance Network (ReLAVRA-PAHO) showed a progressive increase in the percentages of resistance reported during the period 2000-201319-23 (Table 1). Even though statistics do not show discrimination among genospecies, some studies conducted in the area evidence a participation of A. baumannii in nosocomial infections higher than 90%27. Therefore, it could be affirmed that resistance rates would not vary significantly if only A. baumannii isolates had been considered in the analysis27.
Table 1 Evolution of carbapenem resistance in Acinetobacter spp. isolates recovered in several Latin American countries. Annual reports by ReLAVRA-PAHO

Carbapenem resistance
Acquired carbapenem resistance in Acinetobacter spp. is often associated with acquired carbapenemase production. The most frequent ones are carbapenem-hydrolyzing class D β-lactamases (CHDLs) and secondly, metalloenzymes (MBL) such as VIM, IMP and NDM37,38.
OXA-type carbapenemases
Currently, there are six subclasses of CHDLs associated with A. baumannii: intrinsic chromosomal OXA-51-like enzymes and acquired OXA-23-like, OXA-24-like, OXA-58-like, OXA-143-like and OXA-235-like. CHDLs exhibit weak carbapenem hydrolysis; however, they can confer resistance mediated by the combination of natural low permeability and ISAba elements located upstream of the gene. The blaOXA-51-like gene codes for the intrinsic carbapenemase found in A. baumannii although clinically significant resistance to carbapenems mediated by blaOXA-51-like has only been observed in isolates with the insertion sequence ISAbai located immediately upstream of the gene. However, plasmids harboring ISAba1-blaOXA-51-like have been detected in A. baumannii, Acineto-bacter nosocomia/is and Acinetobacter pittii, as well. This affects the accuracy of using blaOXA-51-like detection as a tool for differentiating A. baumannii from other Acinetobacter species.
The first reported OXA-type enzyme was a plasmid-encoded β-lactamase described in 1985 that was initially named ARI-1 and later OXA-2 324,37. The blaOXA-23 gene can be located either on the chromosome or on plasmids37. This carbapenemase was the first described in LA in addition to being the most frequently reported and geographically most disseminated in LA. Its presence has been reported in all the Latin American countries where molecular epidemiology studies have been published (Table 2 and Fig. 1).
Table 2 Reports of epidemiological and microbiological features of carbapenemase-producing A. baumannii in Latin America
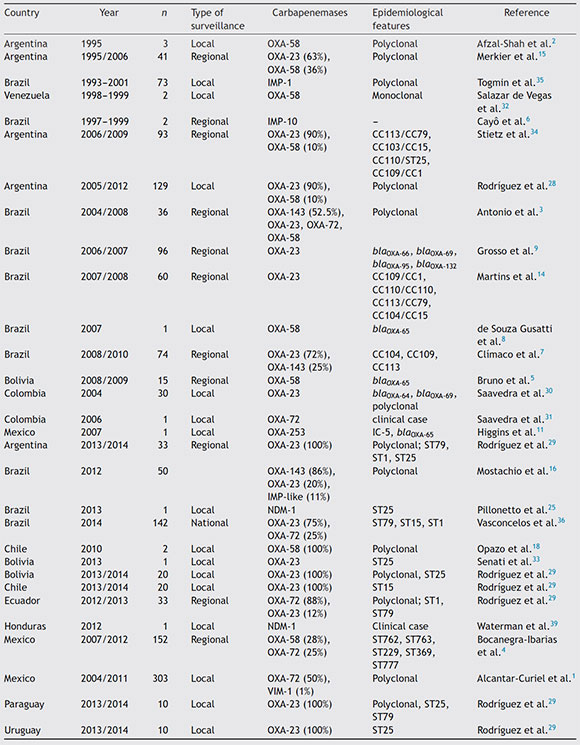
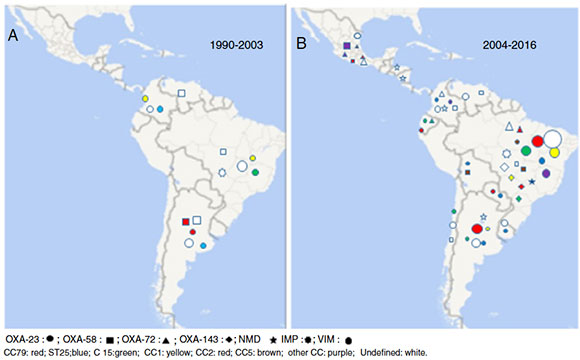
Figure 1 Comparative analysis of the carbapenemase distribution in A. baumannii isolates in Latin America (periods 1990-2003 and 2004-2016) and clonal relatedness.
The worldwide dissemination of blaOXA-23 would be related to International clones I or II. In South America (SA) this carbapenemase has been commonly associated with CC113/CC79; however, it has also been detected in clones recovered in a lower proportion (CC104/CC15, CC110/ST25, CC109/CC1) and in many sporadic isolates3,6,9,14,17,28,30,34,36. Some OXA-23 allelic variants, such as OXA-239, have been described, which showed a major presence in studies conducted in the south of Mexico in the year 20141.
As it can be observed in Figure 1, OXA-23 predominates in all the countries of the region, it is the most frequently detected carbapenemase in the CR-Ab population, except for some studies carried out in the south of Mexico1,4.
In the mid-1990s, blaOXA-58 was reported in Argentina and Venezuela2,32. Ten years later, outbreaks by CR-Ab have shown the presence of OXA-58 as the main carbapenem-resistance mechanism in Bolivia and Chile5,18. Coincidentally to what has been detected in other regions in recent years, a total displacement of blaOXA-58 by blaOXA-23 was observed in LA. In Argentina, the presence of OXA-58 in the resistant population has gradually declined from 36% in 1995 to 0% in studies conducted after the year 201428. It is also noteworthy to mention the low presence of this carbapen-emase in Brazil, where the first isolate harboring OXA-58 was recovered in the year 2007, and so far, has only been detected sporadically8,36. In Brazil and Bolivia blaOXA-58-producing isolates belonged to CC113/CC79, reaffirming its important presence in the CR-Ab population of LA, whereas in Argentina some strains were found to be associated to CC109/CC15,8,28.
The fact that both carbapenemases have been described in the same STs suggests that the prevalence of one enzyme over another does not only depend exclusively on the clone, but also on the ability to acquire resistance through horizontal gene transfer and the impact on the MIC value of the antimicrobial agents affected, among other factors5,9,14,29,30,34,36.
Earlier, Opazo et al.18 reported the presence of CR-Ab isolates belonging to the 24/40 group in LA, however, unfortunately, they were not sequenced. This carbapene-mase, often plasmid-mediated, has been reported to cause hospital outbreaks in many Intensive Care Units (ICUs) worldwide37. In LA sporadic isolates were described in Brazil and Colombia in the middle of the last decade3,31. Since 2010 the first outbreaks have been detected in Guayaquil, Ecuador (2012) and in Brazil (2014). These isolates belonged to ST15 and CC113/CC79 in Ecuador and Brazil, respectively17,36. In Mexico, on the other hand, OXA-72 seems to be the most important contributor to carbapenem resistance in A. baumannii in several studies conducted in different cities in the north and center of the country1,4.
Two new CHDL variants, OXA-143 and OXA-235, have been described in the last 10 years in LA; OXA-143, of plasmid encoding, possesses 40% similarity with OXA-40; there are two variants of this enzyme: OXA-231 and OXA-25311. As the blaOXA-143 gene is undetectable using the current multiplex PCR assay available, Higgins et al. showed a modified multiplex PCR which can help to monitor the spread of this carbapenemase20.
OXA-143 was detected for the first time in 2004 and to date, it has only been isolated in Brazil, its presence in the south of that country reaching about 70%. blaOXA-143 like genes mainly belong to clonal complexes CC104/CC15, CC109/CC1 and CC113/CC793 7 10 16.
On the other hand, OXA-235 hydrolyzes penicillins and carbapenems but it does not show activity against extended-spectrum cephalosporins. Only one strain was isolated in Mexico in 201611.
Metallo-β-lactamase carbapenemases
Metallo-β-lactamases are divided into six families; of these, only IMP, VIM, SIM and NDM enzymes have been detected in A. baumannii38. We can differentiate 2 periods regarding the presence of MBLs in LA. The first period started in the mid-1990s, with the detection of IMP1 in Brazil35. Even though more than 15 years have passed and that more allelic variants have been detected (IMP10), these isolates have been restricted to a few hospitals located in e Sao Pablo State6. Apart from Brazil, sporadic isolates harboring blaIMP, blavIM-1 and blaVIM-4 have been described in Mexico1,4. The second period started with the detection of the blaNDM-1 gene almost simultaneously in Honduras (2012) and Brazil (2013) in A. baumannii isolates belonging to ST2 525,39. Later in the following years, its presence was communicated in Argentina, Colombia, Nicaragua and Paraguay21,23. Moreover, this enzyme was also detected in other genospecies different from A. baumannii as well as in Enterobacteri-aceae.
Other carbapenemases
Carbapenemases different from CHDLs and MBLs are rare in A. baumannii24. However, it is noteworthy to mention the importance of the presence of KPC in A. baumannii isolates recovered in Puerto Rico13,26. The possibility of transmission of multidrug-resistant A. baumannii by tourism and/or human migration is a widely described phenomenon in A. baumannii. Therefore, the important interrelationship between the Caribbean country and SA would imply the need to implement measures to detect this enzyme in A. bauman-nii.
In the comparative analysis of the 2 symmetric periods shown in Figure 1, it can be observed that OXA-23 is the carbapenemase/oxacillinase mostly present in both periods (1990-2003 and 2006-2016), whereas OXA-58 was mainly detected in the first period and OXA-72; OXA-143 and NDM in the second one.
Clonal dissemination
Different tools have been proposed to investigate the epidemiology of A. baumannii outbreaks. Pulsed-field electrophoresis (PFGE) has been considered the gold-standard technique for fine-scale typing of A. baumannii isolates. The presence of multiple clones has been detected in most of the studies conducted in one hospital unit, which evidences endemic features in the CR-Ab population in LA. Conversely, the multilocus sequence typing technique (MLST) has a better ability to group isolates during large-sized epidemiological analyses. blaOXA-51-like sequence-based typing and 3-locus sequence typing represent economic and rapid methodologies which show a discriminatory power similar to MLST. Most recently, MALDI-TOF has shown to behave less effectively to perform A. baumannii clonal discrimination24.
Despite the widely-accepted idea that a few genotypic groups are responsible for a large proportion of A. bauman-nii infections, particular characteristics of each region have been reported. Contrary to what was reported in Europe and other countries worldwide, in LA, the presence of the international clones II and III represented a minority in the year 2016 7,8,14,24,29,30,34,36.
Research performed in SA has shown a predominance of CC113/CC79. Stietz et al.34 evidenced its presence in isolates recovered before the year 2000 in a retrospective study. Subsequent studies carried out mainly in Brazil, but also in Argentina and Colombia, confirmed the predominance of CC113/CC79 together with CC103/CC15 and CC109/CC1 in CR-Ab isolates7,8,14,30,34,36. In the year 2014 the first plurinational study performed in LA, which involved 9 hospitals belonging to 6 countries, evidenced that its predominance was also extended to countries such as Chile, Uruguay, Paraguay and Ecuador29. The spread of ST25 was also highlighted in the mentioned study in different LA countries, similarly to what was observed in other regions12,29,30,34.
Summary
The main findings and recent changes in the molecular epidemiology of carbapenem-resistant A. baumannii clinical isolates in LA were revised in the present study. Among them, we have observed common features with other regions: (1) A. baumanii represents the predominant genospecies; (2) the main presence of A. baumanii in nosocomial infections and the progressive increase in car-bapenem resistance rates; (3) the high prevalence of the blaOXA-23 gene; (4) the emergence of OXA-72 and NDM-1, and other features such as the low predominance of international clones I, II and III. Therefore, we believe that being able to obtain our own results and figures will lead to the elaboration of a regional casuistic report, which would guide the implementation of the adequate policies to prevent and/or control the spread of multidrug-resistant A. baumannii isolates.
Conflict of interest
The authors declare that they have no conflicts of interest.
1. Alcantar-Curiel MD, Garcia-Torres LF, Gonzalez-Chavez MI, Morfin-Otero R, Gayoso-Vazquez C, Jarillo-Quijada MD, Fernandez-Vazquez JL, Giono-Cerezo S, Rodriguez-Noriega E, Santos-Precieado JI. Molecular mechanisms associated with nosocomial carbapenem-resistant Acinetobacter baumannii in Mexico. Arch Med Res. 2014;45:553-60. [ Links ]
2. Afzal-Shah M, Villar HE, Livermore DM. Biochemical characteristics of a carbapenemase from an Acinetobacter baumannii isolate collected in Buenos Aires, Argentina. J Antimicrob Chemother. 1999;43:127-31. [ Links ]
3. Antonio CS, Neves PR, Medeiros M, Mamizuka EM, Elmor de Araújo MR, Lincopan N. High prevalence of carbapenem-resistant Acinetobacter baumannii carrying the blaOXA-143 gene in Brazilian hospitals. Antimicrob Agents Chemother. 2011;55:1322-3. [ Links ]
4. Bocanegra-Ibarias P, Pena-LopezC, Camacho-OrtizA, Llaca-Diaz J, Silva-Sanchez J, Barrios H, Garza-Ramos U, Rodriguez-Flores AM, Garza-Gonzalez E. Genetic characterisation of drug resistance and clonal dynamics of Acinetobacter baumannii in a hospital setting in Mexico. Int J Antimicrob Agents. 2015;45:309-13. [ Links ]
5. Bruno LS, Gallego L, Amyes SGB. Multi-drug resistance profiles and the genetic features of Acinetobacter baumannii isolates from Bolivia. J Infect Dev Ctries. 2013;7:323-8. [ Links ]
6. Cayo R, Rodrigues-Costa F Matos AP, Carvalhaes CG, Jové T, Gales AC. Identification of a new integron harboring bla(IMP10) in carbapenem-resistant Acinetobacter baumannii clinical isolates. Antimicrob Agents Chemother. 2015;59:3687-9. [ Links ]
7. Clímaco EC, Oliveira ML, Pitondo-Silva A, Oliveira MG, Medeiros M, Lincopan N, da Costa Darini AL. Clonal complexes 104, 109 and 113 playing a major role in the dissemination of OXA-carbapenemase-producing Acinetobacter baumannii in Southeast Brazil. Infect Genet Evol. 2013;19:127-33. [ Links ]
8. de Souza Gusatti C, Martins Bertholdo L, Muner Otton L, Padilha Marchetti D, Alessandra Ferreira E, Corcao G. First occurrence of blaoxa-58 in Acinetobacter baumannii isolated from a clinical sample in Southern Brazil. Braz J Microbiol. 2012;43:243-6. [ Links ]
9. Grosso F, Carvalho KR, Quinteira S, Ramos A, D'Alincourt Carvalho-Assef AP, Asensi MD, Peixe L. OXA-23-producing Acine-tobacter baumannii: a new hotspot of diversity in Rio de Janeiro. J Antimicrob Chemother. 2011;66:62-5. [ Links ]
10. Higgins PG, Poirel L, Lehmann M, Nordman P Seifert H. OXA-143 a novel carbapenem-hydrolyzing class D ß-lactamase in Acinetobacter baumannii. Antimicrob Agents Chemother. 2009;53:5035-8. [ Links ]
11. Higgins PG, Perez-Llarena FJ, Zander E, Fernandez A, Bou G, Seifert H. OXA-235, a novel class D ß-lactamase involved in resistance to carbapenems in Acinetobacter baumannii. Antimicrob Agents Chemother. 2013;57:2121-6. [ Links ]
12. Labarca JÁ, Salles MJ, Seas C, Guzman-Blanco M. Carbapenem resistance in Pseudomonas aeruginosa and Acinetobacter bau-mannii in the nosocomial setting in Latin America. Crit Rev Microbiol. 2016;42:276-92. [ Links ]
13. Martinez T, Martinez I, Vazquez GJ, Aquino EE, Robledo IE. Genetic environment of the KPC gene in Acinetobacter baumanni ST2 clone from Puerto Rico and genomics insights into drugs resistance. J Med Microbiol. 2016;65:92. [ Links ]
14. Martins AF, Kuchenbecker R, Sukiennik T, Boff R, Reiter KC, Lutz L, Machado AB, Barth AL. Carbapenem-resistant Acinetobac-ter baumannii producing the OXA-23 enzyme: dissemination in Southern Brazil. Infection. 2009;37:474-6. [ Links ]
15. Merkier AK, Catalano M, Ramirez MS, Quiroga C, Orman B, Ratier L, Famiglietti A, Vay C, Matino AD, Cetron D. Polyclonal spread of blaOXA-23 and blaoxa-58 in Acinetobacter baumannii isolates from Argentina. J Infect Dev Ctries. 2008;2:235-40. [ Links ]
16. Mostachio AK, Levin AS, Rizek FR, Zerbini J, Costa SF. High prevalence of OXA-143 and alteration of outer membrane proteins in carbapenem- resistant Acinetobacter spp. isolates in Brazil. Int J Antimicrob Agents. 2012;39:396-401. [ Links ]
17. Nunez Quezada T, Rodríguez CH, Castro Canarte G, Nastro M, Balderrama Yarhui N, Dabos L, Acosta Mosquera Y, Plaza Moreira N, Famiglietti A. Outbreak of blaOXA-72-producing Acinetobacter baumannii in South America. J Chemother. 2016;13:1-4. [ Links ]
18. Opazo A, Dominguez M, Bello H, Amyes SGB, Gonzales GR. OXA-type carbapenemases in Acinetobacter baummannii in South America. J Infect Dev Ctries. 2012;6:311-6. [ Links ]
19. Organización, Panamericana de la Salud. Organización Mundial de la Salud. Informe Anual de la Red de Monitoreo/Vigilancia de la Resistencia a los Antibióticos, 2000 Asunción, Paraguay, 31/1 al 2/2; 2000. [ Links ]
20. Organización, Panamericana de la Salud. Organización Mundial de la Salud. Informe Anual de la Red de Monitoreo/Vigilancia de la Resistencia a los Antibióticos, 2002 Buenos Aires, Argentina, 10 al 13 de mayo; 2003. [ Links ]
21. Organización, Panamericana de la Salud. Organización Mundial de la Salud. Informe Anual de la Red de Monitoreo/Vigilancia de la Resistencia a los Antibióticos, 2005 Montevideo, Uruguay, 14 al 16 noviembre 2006. [ Links ]
22. Organización, Panamericana de la Salud. Organización Mundial de la Salud. Informe Anual de la Red de Monitoreo/Vigilancia de la Resistencia a los Antibióticos, 2009 Lima, Perú, 3 y 4 de diciembre; 2009. [ Links ]
23. Organización, Panamericana de la Salud. Organización Mundial de la Salud. Informe anual de la red de monitoreo de la resistencia a los antimicrobianos y vigilancia de las infecciones asociadas a la atención de la salud. Rev Patol Trop. 2014;43:1-108. [ Links ]
24. Peleg AY, Seifert H, Paterson DL. Acinetobacter bauman-nii: emergence of a successful pathogen. Clin Microbiol Rev. 2008;21:538-82. [ Links ]
25. Pillonetto M, Arend L, Vespero EC, Pelisson M, Chagas TP, Carvalho-Assef AP, Asensi MD. First report of NDM-1-producing Acinetobacter baumannii sequence type 25 in Brazil. Antimi-crob Agents Chemother. 2014;58:7592-4. [ Links ]
26. Robledo IE, Aquino EE, Sante MI, Santana JL, Otero DM, León CF, Vásquez GJ. Detection of KPC in Acinetobacter spp. in Puerto Rico. Antimicrob Agents Chemother. 2010;54:1354. [ Links ]
27. Rodríguez CH, Nastro M, Dabos L, Vay C, Famiglietti A. Frecuencia de aislamiento y resistencia a los antimicrobianos en Acinetobacter spp. en un Hospital Universitario de la Ciudad de Buenos Aires. Rev Argent Microbiol. 2014;46:320-4. [ Links ]
28. Rodríguez CH, Nastro M, Fiorilli G, Dabos L, Lopez Calvo J, Farina ME, Vay C, Famiglietti A. Trends in the resistance profiles of Acinetobacter baumannii endemics clones in a university hospital of Argentina. J Chemother. 2014;30:25-7. [ Links ]
29. Rodríguez CH, Balderrama Yarhui N, Nastro M, Nunez Quezada T, Castro Cañarte G, Magne Ventura R, Ugarte Cuba T, Valenzuela N, Roach F, Mota MI, Burger N, Velázquez Aguayo G, Ortellado-Canese J, Bruni G, Pandolfo C, Bastyas N, Famiglietti A. Molecular epidemiology of carbapenem-resistant Acinetobacter baumannii in South America. JMed Microbiol. 2016;65:1088-91. [ Links ]
30. Saavedra SY, Nunez JC, Pulido IY, Gonzalez EB, Valenzuela EM, Reguero MT, Mantilla JR, Arango AI, Bravo P Characterisation of carbapenem-resistant Acinetobacter calcoaceticus-baumannii complex isolates in a third-level hospital in Bogotá Colombia. Int J Antimicrob Agents. 2008;31:389-91. [ Links ]
31. Saavedra SY, Cayo R, Gales AC, Leal AL, Saavedra CH. Early dissemination of OXA-72-producing Acinetobacter baumannii strain in Colombia: a case report. Braz J Infect Dis. 2014;18:678-80. [ Links ]
32. Salazar De Vegas EZ, Nievesm B, Ruiz M, Ruíz J Vila J, María A, Elsa V. Molecular epidemiology and characterization of resistance mechanisms to various antimicrobial agents in Acinetobacter baumannii isolated in Mérida Venezuela. Med Sci Monit. 2007;13:89-94. [ Links ]
33. Senati S, Vilagran AL, Bartoloini A, Rossolini GM, Pollecchi L. OXA-23 producing ST Acinetobacter baumannii: first report in Bolivia. J Glob Antimicrob Resist. 2016;4:70-1. [ Links ]
34. Stietz MS, Ramírez MS, Vilacoba E, Merkier AK, Limansky AS, Centrón D, Catalano M. Acinetobacter baumannii extensively drug resistant lineages in Buenos Aires hospitals differ from the international clones I-III. Infect Genet Evol. 2013;14: 294-301. [ Links ]
35. Togmin M, Gales A, Penteado A, Silbert S, Sader H. Dissemination of IMP1 metallo-beta-lactamase-producing Acinetobacter species in a Brazilian teaching hospital. Infect Control Hosp Epidemiol. 2006;27:742-7. [ Links ]
36. Vasconcelos AT, Barth AL, Zavascki AP, Gales AC, Levin AS, Lucarevschi BR, Cabral BG, Brasiliense DM, Rossi F Furtado GH, Carneiro IC, da Silva JO, Ribeiro J, Lima KV, Correa L, Britto MH, Silva MT, da Conceicäo ML, Moreira M, Martino MD, de Freitas MR, Oliveira MS, Dalben MF, Guzman RD, Cayo R, Morais R, Santos SA, Martins WM. The changing epidemiology of Acinetobacter spp. producing OXA carbapenemases causing bloodstream infections in Brazil: a BrasNet report. Diagn Microbiol Infect Dis. 2015;83:382-5. [ Links ]
37. Walther-Rasmussen J, Hoiby N. OXA-type carbapenemases. J Antimicrob Chemother. 2006;57:373-83. [ Links ]
38. Walsh T, Toleman M, Poirel L, Nordmann P, Metallo-ß-lactamases: the quiet before the storm? Clin Microbiol Rev. 2005;18:306-25. [ Links ]
39. Waterman PE, McGann P Snersud E, Clifford RJ, Kwak YI, Munoz-Urbizo IP, Tabora-Castellanos J, Milillo M, Preston L, Aviles R, Sutter DE, Lesho EP. Bacterial peritonitis due to Acinetobacter baumannii type ST25 with plasmid-borne New Delhi metallo-ß-lactamase in Honduras. Antimicrob Agents Chemother. 2013;57:4584-6. [ Links ]














