Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista argentina de cardiología
versión On-line ISSN 1850-3748
Rev. argent. cardiol. vol.83 no.3 Ciudad Autónoma de Buenos Aires jun. 2015
ORIGINAL ARTICLE
Impact of a Meditation Program on Pulse-Wave Velocity, C-reactive Protein and Quality of life
Impacto de un programa de meditación sobre la velocidad de onda de pulso, la proteína C-reactiva y la calidad de vida
MELINA HUERINmtsaC, 1, 2, WALTER MASON JUÁREZmtsaC, 2, MART ÍN LOBOmtsaC, 2, JULIETA RODRÍGUEZ1, NOEMÍ LAGOmtsaC, 2, MARÍA ROSTAN 2, ÁLVARO SOSA LIPRANDIMTSAC, 1
Received: 08/06/2014 Accepted: 10/21/2014
Address for reprints: Dra. Melina Huerin - Instituto Cardiovascular Lezica, Cardiología - Martín Lezica 3021 - (1642) Lomas de San Isidro, Pcia.de Buenos Aires - e-mail: mhuerin@lezicacardio.com
MTSAC Full Member of the Argentine Society of Cardiology
1 Instituto Cardiovascular Lezica
2 “Mario Ciruzzi” Epidemiology and Cardiovascular Prevention Council
ABSTRACT
background: Although various studies refer to the effect of meditation on blood pressure (BP), its impact on other cardiovascular clinical variables is unknown.
Objective: The aim of this study was to evaluate the effects of a meditation program on pulse wave velocity (PWV), quality of life and ultrasensitive C-reactive protein (us-CRP) in patients with ischemic heart disease or chronic heart failure.
Methods: This was a randomized study with two groups of patients: a meditation group (M) and an active control group (AC) with cardiovascular health education, evaluating the difference between initial and final values at 12 weeks of B P, PWV, quality of life (assessed by the SF-36 questionnaire) and us-CRP.
results: Thirty-five patients were included in the M group and 35 in the AC group; mean age was 61 years and 80% were men. Both groups had similar baseline characteristics, except for higher number of smokers and triglyceride levels in the M group. At 12 weeks, no significant differences were found for ∆PWV: +0.51 (±1.40) in AC and +0.19 (±1.53) in M (p=0.37). Conversely, ∆SF-36 was +0.79 (±7.58) in AC vs. +5.40 (±9.69) (p=0.03) in M, and ∆us-PCR was +1.17 (±2.9) in AC vs. -0.69 (±0.89) in M (p=0.02).
Conclusions: A meditation program did not significantly modify PWV at 12 weeks. However, patients allocated to this intervention improved their quality of life and us-PCR was significantly reduced. Larger studies are required to confirm these findings and explore the mechanisms involved in this improvement.
Key words: Meditation - Pulse Wave Analysis - Quality of Life - C-Reactive Protein
RESUMEN
introducción: Si bien existen publicaciones referentes al efecto de la meditación en la presión arterial (PA), su impacto en otras variables clínicas cardiovasculares, se desconoce.
Objetivos: Evaluar el impacto de un programa de meditación (M) en la velocidad de onda de pulso (VOP), la calidad de vida y la proteína C reactiva ultrasensible (PCRu) en pacientes con cardiopatía isquémica o insuficiencia cardíaca estable.
Métodos: Se realizó un estudio aleatorizado, randomizando en dos grupos de pacientes: M, basada en meditación y control activo (CA) de educación cardiovascular. Se evaluaron diferencias entre valores iniciales y finales a 12 semanas de PA, VOP, calidad de vida (valorado por SF 36) y PCRu.
resultados: Se incluyeron 35 pacientes en M y 35 en CA, edad media: 61 años, 80% hombres. Las características basales de ambos grupos fueron similares a excepción del mayor número de tabaquistas y triglicéridos más elevados en el grupo de M. Al cabo de 12 semanas, el Delta VOP no tuvo diferencias significativas: + 0,51 (±1,40) en CA y de + 0,19 (± 1,53) en M (p=0,37). El Delta SF 36 fue de + 0,79 (±7,58) vs + 5,40 (±9,69) (p=0,03) en CA y M, respectivamente y el Delta de PCRu fue de + 1,17 (+-2,9) en CA vs -0,69 (+-0,89)en M (p=0,02).
Conclusiones: Un programa de M no modificó significativamente la VOP a 12 semanas. Sin embargo, los pacientes asignados a esta intervención mejoraron su calidad de vida y redujeron su PCRu en forma significativa. Se requieren estudios de mayor tamaño que confirmen estos hallazgos y exploren los mecanismos involucrados en esta mejoría.
Palabras clave: Meditación - Análisis de Onda de pulso - Calidad de vida - Proteína C Reactiva
AC Active control
BMI Body mass index
BP Blood pressure
CBP Central blood pressure
M Meditation
PWV Pulse wave velocity
PPA Pituitary Pineal Activation
TM Transcendental meditation
us-CRP Ultrasensitive C-reactive protein
INTRODUCTION
Cardiovascular disease is a major cause of death, mainly due to coronary heart disease and stroke, (1) that equally affects both men and women. It also pre-sents high risk of new cardiovascular events. (2) In this scenario, numerous lifestyle and pharmacological therapeutic options are used to reduce the risk of new events in patients with established cardiovascular dis-ease. Among the non-pharmacological strategies, dif-ferent studies report the benefits of meditation (M) programs in controlled designs, with significant improvement in blood pressure (BP) levels (3-8) and in the development of atherosclerosis assessed through carotid intima-media thickness. (9) Although most of these studies employed transcendental medita-tion (TM), (7, 8) there are few published studies on the effects of other types of M, as the one called APP. The aims of this study were: 1) to verify whether an APP-based M program was able to reduce pulse wave velocity (PWV) in patients with established cardiovascular disease, and 2) to analyze the program impact on an inflammatory marker [ultrasensitive C-reactive protein (us-CRP)], other arterial stiffness parameters and quality of life. (10, 11)
METHODS
A prospective, open-label, randomized, controlled study of M versus active control (AC) with cardiovascular education was performed between January and October 2013. It en-rolled men and women >21 years, referred from different centers in CABA and Buenos Aires outskirts, with history (more than 3 months) of acute myocardial infarction, percutaneous coronary intervention, coronary artery bypass graft surgery, stable chronic angina or dilated cardiomyopa-thy/chronic heart failure. In these patients, clinical history, PWV, B P, systolic central blood pressure (CBP), lipid panel, us-CRP and quality of life testing (SF-36) were recorded. Patients were randomized in a simple fashion to M or AC. At week 12, the patients completed again all the measure-ments. Adherence to the allocated group was evaluated by telephone contact at 4, 8 and 12 weeks.
The primary endpoint was the difference between ini-tial and final PWV (∆PWV) at week-12 between the two study groups, measured in meters/second (m/s). The second-ary endpoints were the difference between initial and final values (∆) of the following variables: quality of life (SF-36 score), us-CRP in mg/L, CBP in mmHg and BP in mmHg.
M Group
Patients assigned to this group were taken to a facility in Capilla del Señor, Buenos Aires, where they were trained during two days by Alkymia Global instructors specialized in APP meditation (Figure 1). APP meditation is an intervention technique different from TM, based upon activations and connections of the subject with images associated to his/her health, in this case, focused on cardiovascular health. Patients had to practice M twice a day during 20 minutes. After finish-ing their training period, patients received a CD with a guide of exercises to be performed during the subsequent 12 weeks. Six follow-up group sessions were carried out bimonthly in charge of the Alkymia team to reinforce and go over the tech-niques. The intervention did not imply any type of patient renunciation to beliefs, creed or religion they held.
aC Group
Patients had to attend health education and cardiovascular prevention workshops lasting 2 hours each, where they re-ceived information on cardiovascular risk factors and cardiovascular prevention measures. Six bimonthly educational lectures were given by doctors, emphasizing care concerning healthy habits.
Evaluation of arterial stiffness
All parameters were assessed using TensioMedTM Arterio-graph, a validated device of non-invasive medicine. (12-14)
Measurementsare obtained from oscillometric data by occlusion of the brachial artery with a balloon inflated to suprasystolic pressure. Pulse wave velocity indicates the ra-tio between the distance traveled by the pulse wave (along the arterial wall) between two points of the arterial tree and transit time; its value is directly associated with arterial stiffness, so the higher the PWV, the greater the stiffness. Measurements were performed with the following require-ments: (15) patient at rest for at least 5 minutes, in recum-bent position, similar time of day to perform the different measurements and interruption of smoking and caffeine-rich beverages at least 3 hours prior to taking measure-ments. Each arteriograph measurement provided PWV, BP and CBP values. To assess final B P, two BP measurements were performed with mercury sphygmomanometer (in each arm), according to the European guidelines on BP manage-ment, (16) which were averaged with the BP values reported by the arteriograph. Measurements were taken in a single center by one operator.
Quality of life test
The SF-36 health survey questionnaire (Argentine adap-tation validated from the Spanish version of the test) was used. (17) This is a self-administered questionnaire that cov-ers the perception of an individual on different aspects of his/her health. The final test result provides two scores cor-responding to physical and mental health which are added to obtain an overall result. (18, 19) The better the perceived health status, the higher the final score. (20) Each of the two components has a value ranging from 30 (worse) to 70 (bet-ter). The mean score for the general population is 50.
laboratory
Lab testing was centralized and blood samples were with-drawn in the morning after 12-hour fasting. Hematocrit, hemoglobin, platelet count, GOT, GPT, creatinine, urea, so-dium, potassium, total cholesterol, HDL-cholesterol, triglycerides, blood glucose, and CPK were measured. LDL-cho-lesterol was estimated with the Freedwald formula, except for patients with triglycerides >3000 mg/dL, in which case LDL-cholesterol was directly assayed. In two-third of pa-tients, us-CRP was measured by immunoturbidimetry assay.

Fig. 1. Meditation training with Alkymia Global instructors
statistical analysis
Sample size was established to obtain a difference in PWV variation of 1.5 m/s with±2.2 m/s standard deviation. With these premises 70 patients (35 per group) were required, with p<0.05 (α=5%) and 80% power. Ten % additional pa-tients were included to account for possible loses. Simple randomization, 1:1 to AAP or AC, was used. The "intention to treat" analysis was employed. Normal distribution of variables was explored analyzing the mean, standard deviation, skewness, kurtosis and histogram, and using the Shapiro-Wilk test. Continuous data were compared with Student´s t test for normal distribution or the Mann-Whitney-Wilcoxon test for non-normal distribution.
The chi-square test was used to analyze categorical data. Continuous data were expressed as mean±SD and categori-cal variables as percentages. Blinded statistical analysis was performed by professionals from the Argentine Society of Cardiology, independent from Alkymia Global.
Ethical considerations
The study was approved by the Ethics Committee of the Ar-gentine Society of Cardiology and was performed following the recommendations in medical research suggested by the Helsinki Declaration (21), good clinical practice guidelines and valid ethical regulations.
RESULTS
From a total of 77 patients included in the program, 70 (91%) completed the study. Seven patients aban-doned the study before starting any intervention, 4 from the M group and 3 from the AC group. Baseline characteristics (Table 1) were similar for both groups, except for a higher number of smokers and elevated triglyceride levels in the M group (4 patients in M vs. none in AC). The difference in parameter values be-tween both groups is detailed in Table 2.
The primary endpoint, ∆PWV, was not significantly different between the two groups. Baseline PWV val-ues varied from 9.32 m/s (±1.24) to 9.82 m/s (±1.56) at 12 weeks in the AC group (p=0.06) and from 9.91 m/s (±1.85) to 10.01 m/s (±1.72) in the APP group (p=0.45), with ∆PWV of 0.51 m/s (±1.40) and 0.19 m/s (±1.53) in each group, respectively (p=0.37). SF-36 re-sults are detailed in Figure 2. ∆SF-36 was significantly lower in the AC group compared to the M group: +0.79 (±7.58) vs. +5.40 (±9.69), (p=0.03). Ultrasensitive-CRP results are illustrated in Figure 3. Baseline and 12-week CBP values in the AC group were 127.43 mmHg (±17.50) and 132.59 mmHg (±15.99), respec-tively (p=0.15), and 136.70 mmHg (±28.32) and 133.63 mmHg (±37.10) (p=0.57) in the M group, with ∆CBP of +5.15 mmHg (±20) and -3.07 mmHg (±32) in each group, respectively (p=0.09). No significant differences were found between both groups for BP and the re-maining parameters over the 12-week period. Median patient adherence was 75% in the M group and 78% in the AC group.
DISCUSSION
Numerous interventions are designed to reduce cardiovascular risk in patients with prior cardiovascular disease. (2) This scenario includes strategies oriented to improve surrogate indicators or variables which have shown to be associated with the risk of clinical events, as PWV, quality of life and us-CRP, among oth-ers. (10, 11) Several publications refer to the impact of M programs on cardiovascular manifestations, es-pecially on the practice of TM in the area of hyperten-sion. (3-6) Interesting results from recent randomized studies and meta-analyses compare the practice of M with the use of antihypertensive drugs, and even the American Heart Association released a consensus document, with IIB recommendation and level of evi-dence B, for different alternative practices and their impact on B P. (7, 8) Our study used an intervention strategy different from TM, based on activations and connections of the subject with images referred to his/ her cardiovascular health, and analyzed whether this intervention could reduce parameters associated with arterial stiffness and produce some impact on quality of life and us-CRP. We chose PWV as primary endpoint, as it is an indicator with growing evidence of its association with risk (11) and because up to the pre-sent, there are no publications that have investigated the impact of M on this parameter. The literature in-dicates that PWV and CBP increase with acute and chronic stress, (22) In this framework, a M strategy, able to modulate stress, could reduce these param-eters. Since our result was negative, we postulate as possible explanation lack of M efficacy on PWV and insufficient power of our study to demonstrate an im-pact on this variable. A similar study explored the effect of a TM program in 103 patients with metabolic syndrome. (23) Even though the authors reported sev-eral improved clinical and laboratory indicators, TM did not have a favorable impact on endothelial func-tion, a parameter associated to PWV.
Regarding the secondary endpoints of our study, the M group improved their quality of life assessed through the SF-36 questionnaire. (17-20) The overall test score improved in the M and not in the AC group, and the mental component was the main reason for the improvement.
Additionally, patients in the M group significantly reduced us-CRP, a parameter repeatedly associated with the risk of new cardiovascular events. (24, 25) Since during the time of the study there was no change in the drug regimen, body weight or lipid panel in ei-ther group, us-CRP reduction in the M group cannot be explained by these factors. A study with a smaller sample size and "before-after" design obtained similar results on the association between improved quality of life assessed with the SF-36 and us-CRP reduction in 24 subjects after 8 weeks of meditation. (26)
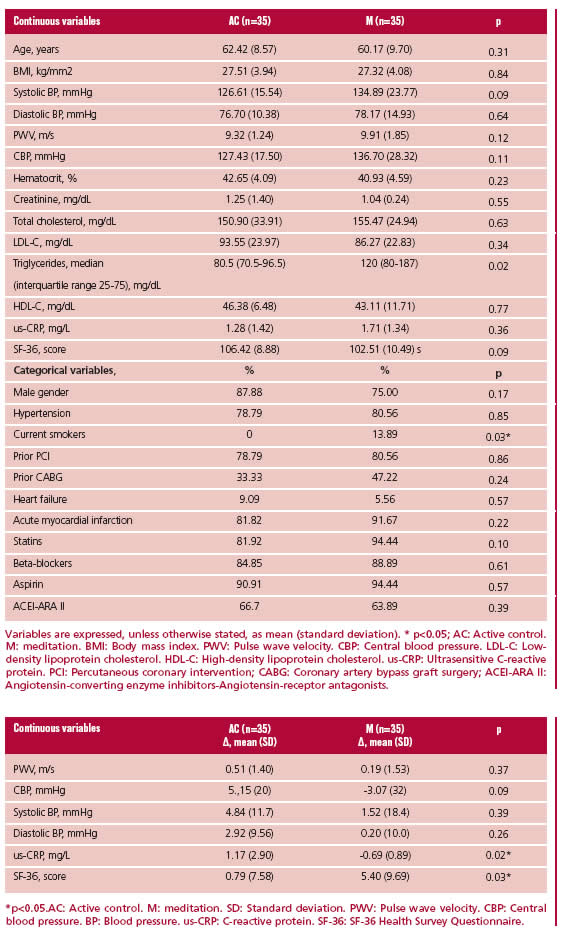
Variables are expressed, unless otherwise stated, as mean (standard deviation). * p<0.05; AC: Active control. M: meditation. BMI: Body mass index. PWV: Pulse wave velocity. CBP: Central blood pressure. LDL-C: Low-density lipoprotein cholesterol. HDL-C: High-density lipoprotein cholesterol. us-CRP: Ultrasensitive C-reactive protein. PCI: Percutaneous coronary intervention; CABG: Coronary artery bypass graft surgery; ACEI-ARA II: Angiotensin-converting enzyme inhibitors-Angiotensin-receptor antagonists.
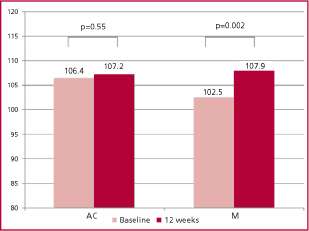
Fig. 2. Quality of life assessed by the SF-36 health survey ques-tionnaire. AC: Active control. M: Meditation
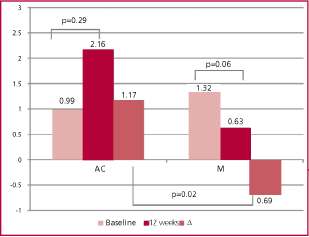
Fig. 3. Comparison of ultrasensitive C reactive protein in both groups. AC: Active control. M: Meditation.
lar context, particularly in TM publications. We believe that the characteristics of our population, with 100% of patients presenting with previous cardiovascular dis-ease, elevated drug use (more than 80% were receiving beta-blockers, nearly 65% ACEI or ARAII agents and more than 90% statins or aspirin) and very low lev-els of total cholesterol and LDL-cholesterol, may have played a role in the scarce variation of this parameter, since studies evidencing MT-associated BP reduction mainly included patients without prior cardiovascular disease and lower use of cardiovascular drugs. Prob-ably, the patients included in our study, with optimal standards of care and pharmacological regimen, had less margin to additionally improve B P. (28)
Regarding CBP, which in addition to its association with cardiovascular mortality (14) has been recently identified as a more stringent indicator of antihyper-tensive therapy, (29) it was significantly reduced in the M group (p=0.09)
As the intervention required training in a specific practice which the patients had to keep for 12 weeks, we decided to evaluate treatment adherence through telephone contact at prespecified intervals. Adherence above 75% was similar in both groups and was consid-ered adequate.
Different publications in the international litera-ture have evaluated the effect of meditation-based programs on clinical events. A study by Blumenthal et al. (30) reported that patients randomized to M had lower recurrence of coronary events at 5 years than those assigned to conventional treatment. Data from three randomized studies evaluating the impact of M on "hard" events reported between 30% and 48% rela-tive risk reduction for overall mortality, cardiovascular death and infarction in patients assigned to an in-tervention group versus those receiving conventional care or education, as in our study. (31, 33)
LIMITATIONS
The main limitation of the study is its relatively small size. Moreover, the sample might also have low pow-er to yield significant differences in patient baseline characteristics, considering that some variables (sta-tin use, B P, CBP, male gender, infarction or prior sur-gery) might reach statistical significance with a larger sample size. Also, other confounders might affect the comparison between interventions; for example, the M program required a 70 Km trip to a natural envi-ronment that could have created different expecta-tions than in those attending healthcare educational workshops. On the other hand, the degree of participant belief or confidence in the M technique might help or not the intervention placebo effect. Finally, the reproducibility of the M technique could be a limitation for routine use of this intervention.
CONCLUSIONS
A meditation program did not significantly modify PWV at 12 weeks in patients with previous cardiovascular disease. However, patients assigned to this inter-vention improved their quality of life and significantly reduced us-CRP levels. The incorporation of a simple practice, able to optimize parameters associated with the risk of new clinical events, could represent an al-ternative strategy to be recommended in patients with established cardiovascular disease. Further studies are necessary to confirm these findings, explore the mechanisms involved in this improvement and correct the limitations of this work.
acknowledgements
To Martín Fritzler and Oscar Gaona, who as many other patients teach us the true meaning of trust in medical knowledge, a balance of science, art and love. To the master, Lita Donosos Ocampo.
Financial support
The only economical support received were the expenses of lodging, meals and transfer to the training location of patients assigned to the APP group, and the wages of a physician trained in data loading, pa-tient evaluation for inclusion and measurements at the onset of the study and at 12 weeks. These expenses were financed by Alkymia Global, a company that did not participate in the results of the research.
Conficts of interest
The authors received partial financial support to perform the study from Alkymia Global in charge of the meditation program.
REFERENCES
1. Alwan A, editor. Global status report on non communicable diseases 2010. World Health Organization, 2011. p. 162. [ Links ]
2. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation 2002;106:3143-421.
3. Goldstein CM, Josephson R, Xie S, Hughes J W. Current perspec-tives on the use of meditation to reduce blood pressure. Int J Hyper-tens 2012;2012:578397. http://doi.org/2vk
4. Schneider R, Alexander C, Staggers F, Rainforth M, Salerno J, Hartz A, et al. Long-term effects of stress reduction on mortality in persons ≥55 years of age with systemic hypertension. Am J Cardiol 2005;95:1060-4. http://doi.org/b3hcv6
5. Rainforth M, Schneider R, Nidich S, Gaylord-King C, Salerno J, An-derson J. Stress Reduction Programs in patients with elevated blood pressure: a systematic review and meta-analysis. Curr Hypertens Rep 2007;9:520-8. http://doi.org/ccdgqb
6. Anderson J, Liu C, Kryscio R. Blood pressure response to transcendental meditation: a meta-analysis. Am J Hypertens 2008;21:310-6. http://doi.org/cmhxhk
7. Brook R, Appel L, Rubenfire M, Ogedegbe G, Bisognano J, Elliott W, et al. American Heart Association Professional Education Committee of the Council for High Blood Pressure Research, Council on Cardiovascular and Stroke Nursing, Council on Epidemiology and Preven-tion, and Council on Nutrition, Physical Activity and Metabolism. Beyond Medications and Diet: Alternative Approaches to Lowering Blood Pressure. A Scientific Statement From the American Heart As-sociation. Hypertension 2013;61:1360-383. http://doi.org/2vm
8. Schneider R. Evidence for Upgrading the Ratings for Transcendental Meditation: Response to AHA Scientific Statement on Alternative Methods and B P. Hypertension 2013;62:e42-e43. http://doi.org/2vn
9. Castillo-Richmond A, Schneider R, Alexander C, Cook R, Myers H, Nidich S, et al. Effects of stress reduction on carotid atherosclerosis in hypertensive African Americans. Stroke 2000;31:568-73. http://doi. org/dn36t7
10. Willum-Hansen T, Staessen JA, Torp-Pedersen C, Rasmussen S, Thijs L, Ibsen H, et al. Prognostic value of aortic pulse wave veloc-ity as index of arterial stiffness in the general population. Circulation 2006;113:664-70. http://doi.org/cfq9qd
11. Helfand M, Buckley D, Freeman M, Fu R, Rogers K, Fleming C, et al. Emerging risk factors for coronary heart disease: A summary of systematic reviews conducted for the U.S. Preventive Services Task Force. Ann Intern Med 2009;151:496-507. http://doi.org/2vp
12. Horvath I, Nemeth A, Lenkey Z, Alessandri N, Tufano F, Kis P, et al. Invasive validation of a new oscillometric device (Arteriograph) for measuring augmentation index, central blood pressure and aor-tic pulse wave velocity. J Hypertens 2010;28:2068-75. http://doi.org/ fnm9zz
13. Rajzer M W, Wojciechowska W, Klocek M, Palka I, Brzozowska-Kiszka M, KaweckaJaszcz K. Comparison of aortic pulse wave veloc-ity measured by threetechniques: Complior, sphygmocor and arterio-graph. J Hypertens 2008;26:2001-7. http://doi.org/ckd3t2
14. Stoner L, Young JM, Fryer S. Assessments of arterial stiffness and endothelial functionusing pulse wave analysis. Int J Vasc Med 2012;2012:903107. http://doi.org/2vq
15. Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, et al. Expert consensus document on arterial stiff-ness: methodological issues and clinical applications. Eur Heart J 2006;27:2588-605. http://doi.org/c74t3h
16. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G. ESH-ESC Practice Guidelines for the Management of Arterial Hypertension: ESH-ESC Task Force on the Management of Arterial Hypertension. J Hypertens 2007;25:1751-62. http://doi.org/fgxp5m
17. Augustovski F, Lewin G, García EE, Rubinstein A. The Argentine-Spanish SF-36 Health Survey was successfully validated for local out-come research. J Clin Epidemiol 2008;61:1279-84. http://doi.org/fdtbbd
18. Vilagut G, Ferrer M, Rajmilb L, Rebollo P, Permanyer-Miralda G, Quintana J, et al. El Cuestionario de Salud SF-36 español: una década de experiencia y nuevos desarrollos. Gac Sanit 2005;19:135-50. http:// doi.org/ctn247
19. McHorney C, Ware J, Raczek A. The MOS 36-Item Short-Form Health Survey (SF-36) (II). Psychometric and clinical tests of valid-ity in measuring physical and mental health constructs. Med Care 1993;31:247-63. http://doi.org/cch366
20. Ware J, Snow K, Kosinski M, Gandek B. SF-36 Health Survey: manual and interpretation guide. Boston: New England Medical Cen-ter, 1993.
21. 59th WMA General Assembly. Declaration of Helsinki, Seoul, Korea, October 2008. Disponible en: http://www.wma.net/en/30 publications/10policies/b3/, Last access september, 2014.
22. Tomlinson L, Cockcroft J. Post-traumatic stress disorder: breaking hearts. Eur Heart J 2011;32:668-9.http://doi.org/bhsnmg
23. Paul-Labrador M, Polk D, Dwyer J, Velasquez I, Nidich S, Rain-forth M, et al. Effects of a randomized controlled trial of transcendental meditation on components of the metabolic syndrome in sub-jects with coronary heart disease. Arch Intern Med 2006;166:1218-24. http://doi.org/d3swzf
24. Schnell-Inderst P, Schwarzer R, Göhler A. Prognostic value, clini-cal effectiveness, and cost-effectiveness of high-sensitivity C-reactive protein as a marker for major cardiac events in asymptomatic indi-viduals: a health technology assessment report. Int J Technol Assess Health Care 2010;26:30-9. http://doi.org/cfw6vc
25. Goff D, Lloyd-Jones D, Bennett G, Coady C, D'Agostino R, Gibbons R, et al. 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk:A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129:S49-S73. http://doi.org/2vr
26. Fang C, Reibel D, Longacre M, Rosenzweig S, Campbell D, Douglas S. Enhanced psychosocial well-being following participation in a Mind-fulness-based stress reduction program is associated with increased natural killer cell activity. J Altern Complement Med 2010;16:531-8. http://doi.org/d7dw4c
27. Steptoe A, Hamer M, Chida Y. The effects of acute psychological stress on circulating inflammatory factors in humans: A review and meta-analysis. Brain Behav Immun 2007;21:901-12. http://doi.org/ bd52gd
28. Sivasankaran S, Pollard-Quintner S, Sachdeva R, Pugeda J, Hoq J, Zarich S. The effect of a six-week program of yoga and meditation on brachial artery reactivity: Do psychosocial interventions affect vascular tone? Clin Cardiol 2006;29:393-8. http://doi.org/dq3bjs
29. Sharman J, Marwick T, Gilroy D, Otahal P, Abhayaratna W, Stowas-ser M. Randomized trial of guiding hypertension management using central aortic blood pressure compared with best-practice care: principal findings of the BP GUIDE study. Hypertension 2013;62:1138-45. http://doi.org/2vs
30. Blumenthal J, Babyak M, Wei J, O'Connor C, Waugh R, Eisen-stein E, et al. Usefulness of psychosocial treatment of mental stress-induced myocardial ischemia in men. Am J Cardiol 2002;89:164-8. http://doi.org/cgv45n
31. Walton KG, Schneider RH, Nidich S. Review of controlled research on the transcendental meditation program and cardiovascular dis-ease: risk factors, morbidity,and mortality. Cardiol Rev 2004;12:262-6. http://doi.org/frhwwv
32. Schneider R, Grim C, Rainforth M, Kotchen T, Nidich S, Gaylord-King C, et al. Stress Reduction in the Secondary Prevention of Cardiovascular Disease Randomized, Controlled Trial of Transcendental Meditation and Health Education in Blacks. Circ Cardiovasc Qual Outcomes 2012;5:750-8. http://doi.org/2vt
33. Prasad K, Sharma V, Lackore K, Jenkins S, Prasad A, Sood A. Use of complementary therapies in cardiovascular disease. Am J Cardiol 2013;111:339-45. http://doi.org/2vv














