INTRODUCTION
Cardiovascular diseases, particularly acute myocardial infarction (AMI), are the first mortality cause in our country and worldwide. Its acknowledgement and the standardization of treatment has a great effect on reducing associated morbimortality. 1-4
In 2015, the Argentine Society of Cardiology (SAC) and the Argentine Federation of Cardiology (FAC) launched ARGEN-IAM-ST, the National Registry of ST elevation myocardial infarction (STEMI) to reveal the delays in the diagnosis and treatment of this disease, and the treatment modalities.
Published analysis show that 88.5% of STEMI patients received reperfusion therapy, but the administration time is far from ideal. 5 Only 35% of patients underwent primary percutaneous coronary intervention (PPCI) with a door-to-balloon time lower than 90 minutes. 6
Some possible causes are the transfer to centers with hemodynamic services, the large distances to those centers, the lack of networks for diagnosis and treatment of STEMI and the lack of diffusion of warning guidance in population, all of which lead to consultation delays. At the same time, AMI diagnosis is a challenge in centers without on-call cardiologists.
In this context, the pharmacoinvasive (PI) strategy, defined as that in which a PCI is performed within the first 24 hours in patients who received fibrinolytic treatment and progressed with positive reperfusion criteria, has shown benefits in the STREAM 7 study on the prevention of reinfarction and recurrent ischemia, and reduction of infarction size, but no decrease in mortality in relation to PPCI at 30 days and 1 year. 8,9 In recent European registries with a longer follow-up period (3-5 years), a difference in mortality in favor of the PI strategy has been established compared to patients who waited more than 120 minutes to access to a PPCI. The longer the door-to-balloon time for these patients, the better the observed benefit on mortality in favor of the PI strategy. 10,11
Therefore, the PI strategy may be considered valid in the context of large distances and multiple centers without hemodynamic resources to decrease reperfusion times using coordinated care networks.
The difference between door-to-needle and door-to-balloon times is a key factor to determine the success of the PI strategy, 12,13 as observed in said European registries.
However, the usage rate of this strategy in our country is low, 5 despite the fact that it is indicated by the Argentine Consensus Statement for ST-elevation acute coronary syndrome in a subgroup of patients defined as “high-risk” if they meet at least 1 of the following criteria: 14
• Heart rate >100 bpm
• Systolic blood pressure <100 mm Hg
• Extensive AMI
• Inferior AMI with right ventricle involvement
• Previous AMI
• Left ventricular ejection fraction <35%
• Killip and Kimball ≥ II
• Complete left bundle-branch block
Therefore, the purpose of this study was to examine the distinctive characteristics of the PI strategy in our country and its correlation with the patient’s risk (selective pharmacoinvasive strategy).
METHODS
ARGEN-IAM-ST is a national prospective, multicenter, observational, and transversal registry. 15
It includes STEMI patients with less than 36 hours of progression, and, to date, 6775 patients have been enrolled. This analysis included 5989 patients enrolled up to May 2022.
We performed a descriptive analysis of the characteristics of the population treated with the PI strategy, the reported times to treatment, its indication and the results obtained, and compared it to PPCI and thrombolysis with positive reperfusion criteria (TL+). We also analyzed its indication in relation to patient’s risk according to the SAC Consensus criteria on STE-ACS. Patients who were not reperfused and those treated with rescue PPCI, or other late reperfusion types were excluded.
Statistical analysis
Qualitative variables are shown as frequencies and percentages with their corresponding confidence intervals (CI 95%). For quantitative variables, means ± standard deviation (SD) or median and interquartile range (IQR) were used according to its distribution. The analysis of qualitative variables was performed with the chi-square test or the Fisher test, as applicable; the analysis of continuous variables was performed with the t-test or Kruskall-Wallis test for non-matched data or through the analysis of variance (ANOVA), as applicable. For the analysis, Stata 13.0® was used and a p-value <0.05 was considered significant.
RESULTS
As of May 2022, a total of 5989 patients were enrolled, of which 4788 were analyzed after excluding patients who were not reperfused and those who underwent rescue angioplasty or other types of late revascularization.
Within this group, only 143 patients underwent PI strategy as reperfusion therapy (2.98%), whereas most patients were treated with PPCI (n = 4240, 88.56%), and the remaining 405 patients (8.46%) with TL+.
Characteristics are described in Table 1.
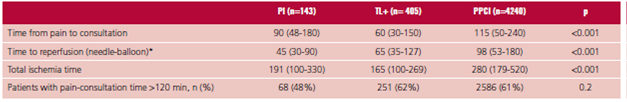
Patients who underwent PI strategy were significantly younger, more frequently smokers, and less hypertensive than those who underwent PPCI. Median (IQR) time from onset of pain to consultation was 90 min (48-180), higher than the group that only received fibrinolytics (60 min) and lower than the PPCI group (115 min) (p <0.001) (Table 2).
Median door-to-needle time in the PI strategy group was 45 min (IQR 30-90), while door-to-balloon time in the PPCI group was 98 min (IQR 53-180) (p <0.01).
A lower total ischemic time (TIT) was observed in patients who received thrombolytics, with a median (IQR) of 165 min (100-269), and in those who underwent PI strategy (191 min, IQR 100-330) compared to PPCI patients (280 min, IQR 179-520), p <0.001.
Based on the above data, there are 89 minutes of difference in total ischemic time (TIT) in favor of patients who received PI strategy compared to those treated with PPCI.
It is worth noting that analysis of PPCI door-to-balloon time includes 38% of patients who required referral to PPCI, and a remaining 62% who had a consultation in centers with hemodynamics services (Table 1). If we analyzed the TIT of the 38% of the patients who were transferred, the median TIT was 435 minutes (260-778), therefore the difference in time to PI strategy would be 244 minutes in this group.
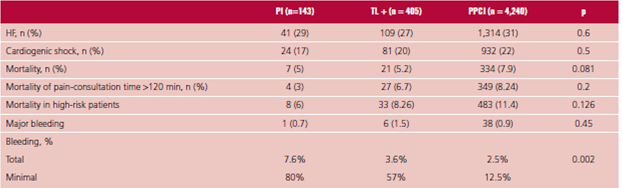
In our analysis, no significant differences were observed in mortality as regards the adopted reperfusion strategy. When considering the subgroup of patients who underwent PPCI with more than 120 minutes of door-to-balloon time, while no significant differences were observed in intra-hospital mortality, development of cardiogenic shock and heart failure, there was a trend favoring the PI strategy.
Bleeding rate in the PI strategy group was 7.6%, with a significant difference compared to PPCI, 2.5%. However, this difference was due to minimal bleedings rather than major ones (Table 3).
No significant differences were observed when choosing the reperfusion strategy according to patient’s clinical risk. Out of the enrolled patients, 58% met the criteria for high clinical risk and 49% of them were transferred for reperfusion treatment, mainly PPCI (73%), while only 3% received PI strategy.
At the same time, within the group of TL+ patients, more than a half was transferred to other facilities, and a similar proportion (57%) of patients met the criteria for high risk. None of these two variables affected the PI strategy selection.
DISCUSSION
PI has a class I-A indication in the European guidelines for myocardial infarction 16 and the American guidelines recommend it with a class II indication and level of evidence B, although the concept of transferring all thrombolyzed patients to a center with hemodynamics is not prioritized. 17 Our national guidelines indicate it with a class I-B recommendation, especially in patients at high clinical risk, based on the risk criteria presented in the CARESS-IN-AMI study. 18 However, usage rate of this strategy is very low (below 3%) and has not changed since the beginning of this registry. If we only consider reperfused patients, there is also no difference in the usage rate of the PI strategy in relation to the total sample (only 3% high-risk patients received pharmacoinvasive strategy). Delays associated with the intrahospital care system due to multiple barriers are predictors of poor prognosis in patients with coronary syndrome. 19
As regards the times, previous data obtained in our registry show that the TIT of a patient transferred to another center for a primary angioplasty is 350 minutes, more than double compared to patients that might initiate a therapy with thrombolytics in their center of origin (50 minutes door-to-needle and 170 minutes TIT)). 20
In our analysis, door-to-needle time for the PI strategy group was 45 minutes, with 191 minutes of TIT, a difference of 244 minutes compared to the TIT of a patient who required a transfer for PPCI.
Considering this data and what has been observed in international registries, PI therapy might have an important role in our population.
When analyzing possible reasons for this under-usage, we observed there is a high percentage (56%) of thrombolyzed patients with positive criteria who are transferred to tertiary healthcare centers; however, they do not receive pharmacoinvasive therapy. This evidences that access to a potential transfer would not be a barrier hindering access to PI strategy.
In addition, acknowledgement of high-risk patients does not affect decision-making. Just over a half of the patients met high-risk criteria, and 49% of them required transfer to be reperfused, especially with PPCI. These patients might benefit from a PI strategy.
The high-risk patients present heterogeneous definitions and prognoses in the different studies that evaluated them 18,21,22. In our registry, the mortality of this subgroup of patients is higher than those who do not belong to the high-risk profile. This finding is supported by significant differences among patients undergoing PPCI and thrombolytics. However, in the PI strategy group, mortality of high-risk patients is not significantly higher than that in the rest of patients, probably due to the number of enrolled patients.
Based on the foregoing, usage or non-usage of PI strategy seems to be explained by a random criterion of certain centers that may have established this strategy as routine compared to centers in which this strategy has not been adopted.
There is a lack of benefit observed in patients with pain-consultation time >120 min and the absence of significant differences in HF and shock incidence during hospitalization, but still a trend favoring this group, indicating the strategy is safe and beneficial. However, the issues mentioned above may be explained by an insufficient sample of patients receiving PI strategy.
As a result, no clear barriers appear to be identified to increase the usage of this strategy beyond its diffusion. Our analysis may be relevant in this context where a selection bias seems to be inexistent.
Regarding the increase in bleeding, whereas a difference against the PI strategy is observed, the bigger risk is due to bleedings defined as minimal.
For this reason and as a first experience analyzing the PI strategy usage in our country, we believe the data obtained may be useful for planning new studies in order to further analyze this issue and promote the actual usage of this strategy in our context.
There are some limitations: ARGEN-IAM-ST registry is a study with voluntary participation; thus, it does not represent the overall situation in the country. It includes participating sites that are mostly affiliated to scientific associations. From another point of view, those non-participating low-complexity low-income sites might have even more difficulties to reach the adequate reperfusion times, and this might result in larger clinical advantages by using the PI strategy. In addition, the number of patients who received PI strategy is low and this may affect the external validity of the results. However, the trend towards fewer ischemic complications than in the PPCI group and the higher risk of bleeding, but minor bleeding, should be highlighted. Moreover, the thrombolytic agent used in the vast majority of referenced registries and papers is tenecteplase (TNK), not available in Argentina.
CONCLUSION
Only 3 out of 100 reperfused patients received PI strategy. Despite the high risk criteria to benefit from this strategy are established and recommended in our national guidelines, it is underused.
Its implementation is not systematically related to high-risk patients, as more than a half of patients who received thrombolytics have not underwent PI strategy, despite having been transferred to other facilities and belonging to a high-risk population.
Despite the under-usage, as the TIT in the PI strategy group is lower than in the TPCA group, the PI strategy remains an option to be considered in our context. It has shown to be a safe strategy with no increase in the number of clinically significant bleeding, and promising for its clinical benefits for patients who cannot reach adequate times for a primary angioplasty.