Heart valve disease affects approximately 2.5% of adults in developed countries. Since 1960, valve replacement with mechanical prostheses is one of the therapeutic alternatives for the management of valve disease. Its main complication is the development of thrombosis or embolic phenomena, with an estimated annual incidence of 0.3-1.3% and 0.7-6%, respectively. 1 The risk is increased in the first months of implantation, depending on its anatomical position and its association with other thromboembolic risk factors (e.g., atrial fibrillation).
We present a case of ST-segment elevation acute myocardial infarction in a young woman with a prosthetic aortic valve who had voluntarily discontinued anticoagulation.
A 23-year-old woman, from the Colombian Pacific region, with a history of mitral regurgitation and mechanical valve prosthesis implantation at 8 years of age, was anticoagulated with warfarin until 2 years ago when she discontinued medical treatment. She consulted the emergency department due to 8 hours of high-intensity oppressive chest pain radiating to the right upper limb, with no other associated symptoms. On physical examination, she was afebrile, with blood pressure of 121/76 mmHg, heart rate 82 bpm, and respiratory rate 19 rpm. Auscultation revealed a grade III/VI holosystolic murmur in the mitral focus, and a grade III/VI diastolic murmur in the aortic focus, with no signs of acute heart failure and no other relevant findings. The electrocardiogram showed sinus rhythm with ST-segment elevation from V1 to V3 and inferior ST-segment depression, with the presence of pathological Q waves in leads I and aVL, and signs of left ventricular enlargement. Emergency coronary angiography was performed 12 hours after admission, which documented a total occlusion of chronic appearance in the mid-proximal segment of the left anterior descending artery (Figure 1) and a thrombotic lesion in the first obtuse marginal of the circumflex artery, with 90% stenosis (Figure 2), without other angiographically significant lesions. Loss of mobility of one of the hemidiscs of the double-disc mechanical valve prosthesis was evidenced, due to in situ thrombus.

Fig. 1 Left: Chronic occlusion of the left anterior descending artery at the junction of the proximal to middle segment (black arrow) with heterocoronary and homocoronary collat eral circulation (white arrow). Right: Obtuse marginal artery with filling defect compatible with thrombus generating subocclusion and TIMI 2 flow (black arrow).
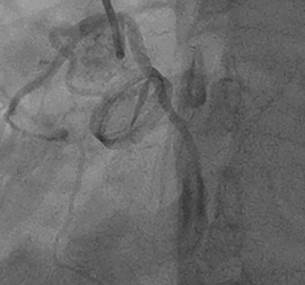
Fig. 2 Loss of mobility of one of the hemidiscs of a mechanical double disc prosthesis due to in situ thrombus
An anomalous origin of the right coronary artery and a second marginal obtuse artery, independently from the left coronary sinus were demonstrated as incidental findings. Due to the high risk of prosthetic thrombosis, it was initially decided to anticoagulate the patient with low molecular weight heparin and warfarin until international normalized ratio (INR) goals were reached. Laboratory tests showed positive cardiac troponin I (6.53 ng/mL for a normal upper limit of 0.12 ng/mL). Transesophageal echocardiogram revealed akinesia without thinning of the anterolateral and inferolateral walls, with a left ventricular ejection fraction of 47% by Simpson's method. It also showed mechanical aortic prosthesis in adequate position with restriction of the posterior leaflet movement, and presence of pannus and marked turbulence in the antegrade flow, with maximum velocity of 3.2 m/s and a mean gradient of 22.5 mm Hg, as well as severe mitral regurgitation secondary to perforation of the anterior leaflet.
With these findings, she underwent aortic valve prosthesis replacement using a n° 23 Medtronic mechanical prosthesis. Enlargement of the aortic annulus with a heterologous pericardial patch using Manougian´s technique, and repair of the mitral valve with closure of the anterior leaflet orifice were performed. Fresh thrombi in the aortic mechanical prosthesis at the hinge level of both discs and severe subvalvular pannus were found. It was not possible to perform revascularization of the anterior descending artery as its course could not be visualized due to the presence of epicardial-pericardial adhesions from the previous surgery, so coronary angioplasty was indicated. The second coronary angiography performed 25 days after admission revealed complete resolution of the thrombotic lesion in the obtuse marginal artery. The total occlusion of the left anterior descending artery persisted, but it was not possible to perform percutaneous revascularization as it was a vessel with a small caliber. It was decided to continue medical treatment, accompaniment by the Psychology and Education service, and she was discharged after 41 days of hospitalization, without complications, with an INR of 3.2 and indications for strict medical control.
Ischemic heart disease is the leading cause of death worldwide, mainly associated with atherosclerosis. Significant atherosclerotic lesions are not found in up to 7% of cases. Coronary embolism is a cause of non-atherosclerotic infarction, and it is estimated that it represents 3% of all myocardial infarctions. It generally affects the left coronary circulation, 1 as in the case of our patient.
The main associated causes are atrial fibrillation, cardiomyopathies, presence of prosthetic valves, endocarditis, tumors, and prothrombotic conditions. Coronary thrombosis associated with acute infection by SARS-CoV-2 during the pandemic has been reported for this entity. 2 Before the use of prosthetic valves, endocarditis was the main cause of death; now atrial fibrillation is mainly considered. 1 Currently, prosthetic valve replacement is the gold standard for the management of severe valve disease in patients with low or intermediate surgical risk. Mechanical valves have a longer life, but are prothrombotic, which requires indefinite anticoagulation to prevent valve thrombosis and embolic events.
There are three types of coronary embolism: direct, paradoxical, and iatrogenic. Direct coronary embolism occurs when an embolus enters the coronary circula tion from the left ventricle, left atrial appendage, pulmonary veins, and the aortic or mitral valve. 3
The clinical, electrocardiographic, and echocardiographic manifestations of myocardial infarction due to coronary embolism are indistinguishable from infarction of atherosclerotic origin, and it should be suspected in patients with prothrombotic risk factors who present with sudden chest pain. 4
There are currently no guidelines for the management of coronary embolism. Intracoronary thrombus aspiration vs. angioplasty alone has been tested in patients with ST-segment-elevation myocardial infarction, without demonstrating an additional benefit in mortality. However, patients with a high thrombotic burden, such as patients with coronary embolism, could benefit more from this measure. 5 In cases of coronary embolism, systemic thrombolysis with tissue plasminogen activator (t-PA) has been reported to be successful in restoring coronary flow. Karakoyun et al 5 effectively and safely treated three patients with coronary embolism associated with prosthetic valves with low-dose intravenous t-PA. Similarly, intravenous infusion of bivalirudin for 48 hours in coronary embolism of the distal right coronary artery has been described, with complete resolution of the thrombus without major bleeding. 6 Other therapies include balloon angioplasty, which has been shown to be successful in restoring blood flow, both as isolated treatment and as adjunctive therapy to thrombotic aspiration. 5
In conclusion, we describe the case of a young woman with mechanical aortic valve prosthesis who voluntarily discontinued anticoagulation and who presented an acute myocardial infarction due to coronary embolism. This condition is potentially fatal, so adherence to pharmacological treatment and education about the disease is essential in a patient at high risk of thrombosis. Permanent anticoagulation, strict clinical monitoring and education are the most important measures to prevent new events.














