Introduction
The air pollution is one of the major issues for the Climate Change due to pollutants such as Carbon (CO), Methane (CH4), water vapor (H2O), among others, that have the potential to increase the global Temperature (Pan-American Health Or-ganization PAHO) 2016; United Nations Frame-work Convention on Climate Change (UNFCCC) 2018). Nevertheless, this is not the only problem, the different components in the air such as Par-ticulate Matter 10 and 2.5 (PM 10, PM 25), have the potential to generate adverse effects on the health of humans and other organisms. The World Health Organization (WHO) estimates nine out of ten people breathe polluted air (Singh etal. 2018; WHO 2018). The result is that each year between 6.5 and 7 million people around the world die due to air pollution exterior and indoor air pollution, this is estimated to increase by 20% in coming years (Singh et al. 2018; Flores-Ramirez et al. 2021b). Chronic exposure to pollutants in the air increases the risk of the development of non-communicable diseases (NCDs) such as Chronic Obstructive Pulmonary Disease (COPD), lung can-cer, and cardiovascular diseases. Now is reported a relationship between exposure to environmental pollutants in the air with the development and increased incidence of various diseases such as renal, lungs and cardiovascular diseases (Flores-Ramirez et al. 2021b), and different clinical and epidemiological studies have demonstrated that the acute and chronic exposure to air pollution can increase the mortality of cardiovascular and respiratory diseases (Fiordelisi et al. 2017). The 24% of diseases around the world and 23% of mortality global is a consequence of environmental factors such as air, water or food pollution; this is proof of the role that the environment plays in people's health. (WHO, 2006; Prüss-Üstün et al. 2016; Alamo-Hernández et al. 2019). For example, many deaths concerning COPD appear in low and middle-income countries, and the principal risk factors are smoking, occupational environments, ozone, passive smoking and household air pollution from solid fuels (Rodríguez-Aguilar et al., 2020). Nonetheless, not everyone is in the same conditions, there are populations more susceptible to the effects of pollution environments, socio and economic conditions, one of these populations are the indigenous people. Only in the region of Latin America and the Caribbean is estimated the indigenous population was around 42 million people in 2015 (Berumen-Rodríguez et al. 2021; Flores-Ramirez 2021a). Those populations are often vulnerable to different environmental, social and economic situations that affect their health; for example, these communities are frequently ubicated in places away from cities, which results in fewer opportunities, the education levels are less in comparation with cities, this cause that many youngers have to work as soon as they finish high school or even before, most of these jobs are precarious and many times these communities have social margination. On the other hand, their environments are often polluted by mycotoxigenic fungi, pathogens, heavy metals in soil or water, or pollutants due to traditional methods of cooking that can cause adverse health effects; furthermore, in these communities access to health centers is limited, and even in the best cases, they only receive basic cares. The mixture of these factors cause a risk for the health, development and for their life quality (Suleyman et al. 2018; Díaz de León-Martínez et al. 2020a; Díaz de León-Martínez et al. 2020b; Flores-Ramirez et al. 2021a).
One of the main issues related to NCDs as men-tioned before is exposure to polluted air. Cooking by using solid fuels like wood is reported to cause chronic exposure to PM 10 and PM 25, carbon monoxide, nitrogen and sulfur oxides, but also organic pollutants such as benzene, phenols, form-aldehyde, and polycyclic aromatic hydrocarbons (PAHs) (Pruneda-Álvarez et al. 2012; Cincinelli y Matellini 2017; Flores-Ramirez et al. 2021b). The latter, are multiple aromatic rings bounded, those containing up to four rings are called “light” and four or more rings are called “heavy” which are more stable and toxic than light ones (Chen et al. 2019; Díaz de León-Martínez et al. 2021a). PAHs are bound in different structural configurations. They can be transferred long distances in Particulate Matter are considered global pollutants because they have the potential to produce carcinogenic and teratogenic effects (Sarigiannis et al. 2015; Alegbeleye et al. 2017; Chen et al. 2019). They are liberated into the environment from natural and anthropogenic sources such as traffic, domestic heating, oil refining, industrial processes, incomplete combustion of solid fuels (Kim et al. 2013; Tavera et al. 2018; Ciao et al. 2020; Ferhat et al. 2020). PAHs present different pathways of exposure, inhalation of smoke, ingestion of contaminated food, and dermical absorption (Agency for Toxic Substances and Diseases Registry (ATSDR) 2016; Díaz de León-Martínez et al. 2021b). Due to their toxic effects and their persistence in the environment PAHs have been classified by the US EPA and European Commission as priority pollutants. Even though, there are around 100 mixtures of
PAHs these agencies have prioritized 16 of them, which are reported to cause mutagenicity, carci-nogenicity and teratogenicity effects (Drwal et al. 2018; Zhu et al. 2019). Because PAHs are highly lipophilic, they have the potential to cross the cel-lular membrane easily and accumulate in fat or other tissue. They are metabolized by cytochrome p450 enzymes and epoxide hydrolase, after, these reactions cause epoxides, dihydrodiol phenols and quinones which are conjugated with glucuronide and sulfate, furthermore, these products will be eliminated by urine. However, on the other hand, they can produce a toxic effect due to PAHs metabolites making covalent attachment with the DNA that result in mutagenesis and therefore, cancer (Cao et al. 2019; Rodríguez-Aguilar et al. 2019). There are known effects of exposure to PAHs in the lungs, cardiovascular diseases, neurotoxicity, however, recent research has associated a signifi-cant burden of renal damage associated with the exposure to these pollutants (Pérez-Maldonado et al. 2018; Ciao et al. 2020; Flores-Ramirez et al. 2021b). The International Agency for Research on Cancer (IARC 2010) listed one of them, the Benzo (a) pyrene in group 1, as a carcinogen to humans. The biomonitoring of these pollutants is frequently carried out in working environments due to occupational exposure, nevertheless, the indigenous populations are also susceptible to suf-fering from the exposure to these pollutants and hence their toxicity. For indigenous people, the main exposure route is through smoke inhalation for wood burning to cook garbage burning and the consumption of polluted foods (Flores-Ramirez et al. 2021b). Only in Mexico, about 27 million people depend on biomass burning especially wood to cook and heat their homes, using traditional open fires which causes chronic exposure; moreover, most of these people are concentrated in rural indigenous communities (Riojas-Rodríguez et al. 2011). For the biomonitoring of PAHs, the quan-tification of hydroxylated metabolites is usually applied, 1-OH-Pyrene (1-OH-PYR) excreted in urine is frequently used as the best biological indi-cator of exposure to PAHs, nevertheless, the use of more excreted products has gained relevance in recent years, because using more metabolites permits a better estimation of exposure.
Indoxyl sulfate (IS) is a small molecule (213 g/mol). It is a uremic toxin that is bound to at least 90% of plasma proteins (Leong and Sirich 2016; Tan et al. 2017). There are clinical studies that sup-port that iS could contribute to the diagnosis of Chronic Kidney Disease (CKD), in this disease, there are uremic products, which tend to accumulate in the blood due to loss of kidneys function to correctly eliminate these toxins. For this reason, uremic toxins like IS are proposed as biomarkers of kidney damage (Barreto et al. 2009; Villaseñor and Martínez y Martínez 2013). Several authors reported in different clinical studies, that IS may contribute to abnormalities in cardiovascular diseases, this uremic toxin is capable to stimulate oxidative stress and also multiple NADPH oxidase signalling pathways; for this reason, IS could help in the diagnostics of renal damage and even a relation with cardiovascular diseases (Gao and Liu, 2017; Szu-Chun et al. 2017; Tan et al. 2017; Xiong and Leong 2019). CKD still affects many people around the world, in México, only in 2019 this disease caused 72, 539 deaths (8.43% of the total deaths that year in Mexico) one of the leading causes of mortality due to NCDs in the country according to data of the Global Burden Disease (IHME 2019).
For pulmonary assessment, spirometry is a tech-nique that by using a spirometer predicts how is the respiratory capacity of a person. This test gives different values after a person is tested, these values can be interpreted, so in this form to know if the patient has normal or abnormal respiratory health, so, the spirometry helps to estimate the risk of lung cancer, COPD, cognitive impairment, cardiovascular or other causes of obstruction in the respiratory tract (Coates et al. 2013; García-Río et al. 2013).
It is important to propose new strategies to as-sess the diagnosis and monitoring of renal and pulmonary disease, which must be accurate and easily implemented in remote locations such as rural communities, where access to health ser-vices is limited and environmental pollution is high, therefore, the main objective of this work was the evaluation of exposure to polycyclic aromatic hy-drocarbons through 10 hydroxylated metabolites of PAHs (1-hydroxynaphtalene (1-OH-NAP) and 2 hydroxynaphtalene (2-OH-NAP); 2-, 3-, and 9- hy-droxyfluorene (2-OH-FLU, 3-OH-FLU, 9-OH-FLU); 1-, 2-, 3-, and 4-, hydroxyphenanthrene (1-OH-PHE, 2-OH-PHE, 3-OH-PHE, 4-OH-PHE) and 1-hy-droxypyrene (1-OH-PYR), also, the evaluation of the renal health through the biomarker Indoxyl Sulfate and the respiratory health through spirometry.
Material and methods2.1 Population and study design.This study was conducted in the community of Tocoy, located in San Antonio, at the Huasteca Potosina, San Luis Potosí, México (21° 38’ 19” N and 98° 52’ 15” W). The average climate is warm and humid, with an annual temperature of around 24°C. There are 1061 habitants approximately of indigenous Tenek origin; this community has been described with high levels of marginalization (Díaz de León-Martínez et al. 2020a)
A transversal study was conducted in November 2019, the ethical protocol was approved by the ethics committee of the Faculty of Medicine of the Autonomous University of San Luis Potosi (CEI-2018-002). An open invitation was extended to the population with the following inclusion criteria: i) older than 30 years old; ii) residence of over 3 years at the site (community); iii) signatures of informed consent; iv) No kidneys disease at the time of the study; v) No recent urinary infections; vi) No medication before sample collection. Meanwhile, the exclusion criteria were: i) insuf-ficient sample and ii) Not having signed the informed consent form. The participants received and answered a questionnaire about topics such as socio-demographic characteristics, general health, family history of chronic diseases and di-etary habits, to identify risk habits of exposure and other risks habits or situations that might apply in the exposition of PAHs (e.g. smokers at home, use of firewood and hours per year in front of this, burning garbage, among others).
2.2 Determination of hydroxylated metabolites in urine.The urine samples were collected from the first micturition in the morning in sterile polypropylene-50 mL glasses after the samples were transported at 4°C and stored at 80°C until analysis. The determination of hydroxylated metabolites in urine was conducted based on the method established by the Centers for Disease Control and Prevention (CDC) with slight modifications. Ten metabolites were determined: 1-, 2-OH-NAP; 2-, 3-, 9-OH-FLU, 1-, 2-, 3- y 4-OH-PHE y 1-OH-PYR. First, 5 mL of each of the samples of urine were filtered through a PVDF membrane. Subsequently, enzy-matic hydrolysis of 2 mL of sample was performed. For this, 20 pL of the enzyme 6-glucuronidase/ arylsulfatase was added (Merck, Millipore, EE. UU) 2 mL of 1 M acetate buffer at pH 5.5 and the samples were incubated at 37°C for 17 h under constant conditions. After this incubation a liquid-liquid extraction was performed in duplicate with an 80:20 (V:V) solution of pentane and toluene evaporated with a gentle stream of nitrogen gas (N) at 45°C until the desired volume of 10 pL was reached, after that, 10 pL of N, O-Bis (trimethylsi-lyl) trifluoroacetamide (BSTFA) (derivatizing agent) (Merck Millipore, Massachusetts, USA) and 2.5 pL of internal standard 13C6 1-OH-PYR (Cambridge Isotopes Laboratories) at 25 ng/ml by calibrating the solution to 100 pL with toluene. Finally, the solution was subjected to a derivatization process at 60°C for 30 min. Samples and calibration curves were analyzed by gas chromatography (GC) (Agilent 6890) coupled to a mass detector (MS) (Agilent 5975) in electron impact ionization (EI) mode. The injection port was operated in splitless mode, with a temperature of 270°C using helium as a carrier gas at a pressure of 36 psi at a constant flow rate of 0.9 ml/min. The chromatographic separation was performed using a 30 m X 0.25 mm X 0.25 pm HP 5 MS column (Agilent®). The oven setting conditions were as follows: 95°C (1 min), 195°C (15°C/min) 206°C (2°C/ min) until minute 13.2, followed by an increase to 320°C (40°C/min) and hold until minute 24 with a total run time of 24 min. The parameters under which the detector was operated are described below: emission of 35 pA and energy, 69.9 V. SCAN mode (50-500 m/z) was used to identify the compound and the identifi-cation and quantification ions were selected for SIM mode. The identification fragment ions were for 1-OH-NAP and 2-OH-NAP 201 and 216 m/z; for 2-OH-FLU and 9-OH-FLU 253 and 254 m/z respectively for 3-OH-FLU 253, 254 and 255 m/z; for 1-OH-PHE, 2-OH-PHE, 3-OH-PHE and 4-OH-PHE 251 and 266 m/z and 1-OH-PYR 290 and 291 m/z and the internal standard 13C6 1-OH-PYR 281 and 296 m/z. The results were obtained and processed with Chemstation software (Agilent®).
2.3 Determination of Indoxyl Sulfate (IS) in plasma.The determination of IS was performed with slight modifications to the methodology described by Barreto et al. (2009) and Xiong and Kwang (2019). The plasma samples were stored at -80°C until their subsequent analysis; briefly, the samples were thawed for approximately 15-20 min. 100 pL of the sample were then taken and deposited in 2.5 mL, then 150 pL of distilled water were added and 900 pL of ice-cold acetonitrile were added to extract the IS; after that, the samples were shaken vigorously for 30 seconds and then centrifuged at 10,000 rpm for 5 min at a temperature of 5°C. From the supernatant, a 2 mL aliquot was ex-tracted and finally, the samples were filtered for further processing in the liquid chromatography. The parameters evaluated for the validation of the method were: Correlation coefficient (0.99); the slope was of (0.079); the limit of detection was 0.01 ppm and the limit of quantification was 0.05 ppm respectively. For reproducibility, it was obtained from 5.1 to 17.9 with repeatability from 0.36 to 25.6, with which it was possible to obtain a confidence interval of 95%.
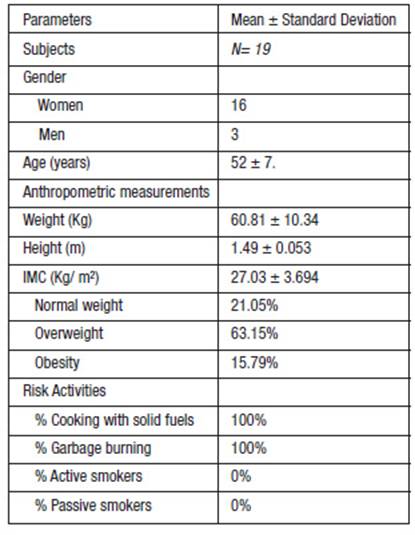
Table 1: Population Characteristics.
2.4. Lung function testFor the pulmonary function assessment, spirometry was performed before and after administration of 200 mg of salbutamol, following the guidelines of the ATS/ERS standards. A spirometer (EasyOne® plus) was used. Spirometry was performed by a professional certified by the National Institute for Occupational Safety and Health (NIOSH) who complied with ATS/ERS standards. The predicted normal values were those of the Mexican-American population of the NHANES III study and the predic-tions of the equations described by Perez-Padilla in the platinum project (Latin American Project for the Investigation of Pulmonary Obstruction) were also used. Measurements included were: Forced expiratory volume in one second (FEV1); Forced Vital Capacity (FVC); and the ratio of the two volumes (FEV1/FVC). The alterations in these spirometric parameters indicate restrictive and obstructive patterns according to the Global Initia-tive for Chronic Obstructive Lung Disease (GOLD) 2019, the results were classified as normal breath-ing patterns, mild restriction, moderate restriction and severe restriction.
3.0 Results 3.1 Characteristics of the study of population There were 19 participants, of whom 16 were women (84.21%) and 3 were men (15.79%). Table 1 “Population characteristics” shows the general anthropometric characteristics and risk activities of the population studied in this research. The anthropometric characteristics of the study par-ticipants are presented below. The average age was 52.09 ± 7.18 years; the average weight was 60.81 ± 10.34 Kg. The average height was 1.49 ± 0.053 m. The average body fat percentage was 38.69 ± 7.98%. The Body Mass Index (BMI) was
27.03 ± 3.694 (CDC, 2015); 12 people (63.15%) presented overweight, 3 people (15.79%) were in a state of obesity, and only 4 (21.05%) were within normal weight values. All study participants reported spending more than 8 hours in front of the stove for cooking and food consumption activities. None of the women reported being preg-nant or breastfeeding. Regarding comorbidities, 3 people reported high blood pressure, 5 had type 2 diabetes mellitus. 100% of the participants reported using firewood during childhood and in the present, so there is chronic exposure, as well as burning garbage.
3.2 Evaluation of hydroxylated metabolites in urine samplesThe data of the results were analyzed by descrip-tive statistics using the "GraphPad Prism" pro-gram. The retention times (TR) obtained for each of the OH-PAHs were TR ± 0.2 min. The TR= 7.6 min for 1-OH-NAP; TR=7.9 for 2-OH-NAP; TR= 12.3 min for 9-OH-FLU; TR=12.5 min for 3-OH-FLU; TR=12.9 min for 2-OH-FLU; TR=14.8 min for 4-OH-PHE; TR= 16. 5 for 3-OH-PHE; TR= 16.7min for 1-OH-PHE; 17.6 min for 2-OH-PHE; and TR= 23.2 min for 1-OH-PYR and 13C6 1-OH-PYR (Díaz de León-Martínez et al. 2021a).
A descriptive statistical analysis was performed where all the hydroxylated metabolites of each sample were summed for better analysis. The mean concentration of Total Hydroxylated Metabolites (I-OH-HAPs) in urine was 6.44 ± 9.79 pmol/ mol of creatinine. Hydroxylated metabolites were found in 89.47% of the samples analyzed. Of the PAHs analyzed in the study population, the most frequently found hydroxylated metabolite was 1-OH-PYR which was present in 84.21% of the samples, followed by 1-OH-NAP and 2-OH-NAP which were present in 68.42% and 63.15% of the samples, respectively. Regarding the other metabolites, 4-OH-PHE was found in 31.57% of the samples, 3-OH-FLU was present in only 2 samples, while 3-OH-PHE and 1-OH-PHE were found in only one sample each; 2-OH FLU,2-OH-
PHE was not detected in any of the samples ana-lyzed. The references valúes were taken from the guideline of Jongeneelen, 2001 which has three levels, nevertheless, these references valúes are just for the excretion for 1-OH-PYR in urine. Table 2 “Results of PAHs in the population” shows the metabolites detected in the samples collected, as well as the percentages and levels obtained. The first reference valúe is the excretion or 1-OH-PYR for 0.24 gmol/ mol of creatinine for non-smokers and 0.74 gmol/ mol of creatinine for smokers; in the second level, with excretion of 1.4 gmol/ mol of creatinine, in this level genotoxic effects starts to appears in workers; for the third level there is two population: coke oven workers with 2.3 gmol/ mol of creatinine and 4.9 gmol/ mol of creatinine for the primary aluminium industry. The mean of 0.33 gmol/ mol of creatinine, exceeds the first reference value, however, the mean does not exceed the second level of Guideline PAHs. The highest value of 1-OH-PYR did not exceed the second reference value either, because the value was 1.11 gmol/ mol of creatinine. On the other hand, 1-OH-NAP was present in 68.42% of samples with a mean of 2.52 gmol/ mol of creatinine, the 2-OH-NAP was present in 63.15% of samples, with a mean of 2.16 gmol/ mol of creatinine
Table 2: Results of OH-PAHs in the population.
3.3. Renal and Respiratory health
For the renal health assessment, the mean con-centrations for IS were 193.4 ± 91.85 gg/L. There are no reference values for this biomarker, so it is not possible to determine exactly the severity of renal damage, so the results of other studies are compared. The 3 men who participated in the study obtained concentrations below the mean. The women obtained concentrations above this value, except for one woman, who had 65.55 gg/L. The respiratory evaluation was performed utiliz-ing a spirometer EasyOne® Plus. The alteration in spirometric values can indicate restrictive and obstructive respiratory patterns. Of the 19 par-ticipants in the study, 9 obtained non-assessable spirometry, 5 showed normal respiratory patterns, 2 were mildly obstructive and 2 were moderately obstructive, 0 were severely restrictive and 1 was below the lower limit, none of them showed ob-structive patterns.
4. DiscussionThe results of this study indicated the study population is highly exposed to a mixture of different PAHs because 89.47% of the population presented detectable levels of one or more hydroxylated metabolites. The metabolite that was in more percent-age of the population was 1-OH-PYR 84.21%, then 1-OH-NAP 68.42%; 2-OH-NAP 63.15%; 4-OH-PHE 31.57%; 3-OH-FLU 10.52%; 9-OH-FLU; 3, 1-OH-PHE 5.26%; on the other hand, 2-OH-FLU and 2-OH-PHE were not detectable to be pres-ent in any of the samples. However, the means were different as 1-OH-NAP obtained a mean in the total population of 2.52 pmol/mol creatinine,
2- OH-NAP with a mean of 2.16 gmol/mol creatinine; 1- OH-PYR 0.33 pmol/mol creatinine; 4-OH-PHE 0.20 pmol/mol creatinine; 9-OH-FLU pmol/mol creatinine; 3-OH-FLU 0.08 pmol/mol creatinine; 3- OH-PHE 0.03 pmol/mol creatinine and 1-OH-PHE 0.02 pmol/mol creatinine. The results were compared with the reference levels proposed by (Jongeneelen 2001). The mean 1-OH-PYR of 0.33 pmol/mol creatinine and the maximum value of
1.11 pmol/mol creatinine exceed Jongeneelen's first reference level of 0.24 pmol/mol creatinine; however, they did not exceed the second level of 1.4 pmol/mol creatinine which is when biological effects are observed. However, the presence of different hydroxylated metabolites depends on the presence of PAHs in the smoke to which the person is exposed (Díaz de León-Martínez et al. 2021b). The results show that the population is not only exposed to this pollutant because the samples also presented detectable levels of 1-OH-NAP with a mean of 2.52 pmol/mol of creatinine;
2- OH-NAP with a mean of 2.16 pmol/mol of creatinine; 9- and 3-OH-FLU with means of 0.12 and 0.08 pmol/mol of creatinine respectively; 4-, 3-, 1-OH-PHE with means of 0.20, 0.03 and 0.02 pmol/mol of creatinine respectively, so the use of a battery of hydroxylated metabolites allows a better estimation of exposure to more pollutants since if only 1-OH-PYR were used as a marker of exposure, the other metabolites would not be taken into account, which as the results show. The presence of these metabolites is demonstrated by the results and allows a better estimation of the pollutants that in these communities are mainly due to the burning of solid fuels such as wood and therefore can cause various adverse health effects, since different epidemiological studies have shown that exposure to PAHs can increase the risk of developing cardiovascular diseases, diabetes, inflammation in the respiratory tract and decreased pulmonary function and respiratory parameters (Perez-Padilla et al. 2010; Rodríguez-Aguilar et al. 2019). Two of them, which were pres-ent in a high percentage in the population studied, were 1- and 2-OH-NAP, which are metabolites of naphthalene, this compound is also found in exposure to solid fuels such as wood combustion. In 2000, the IARC and the US EPA re-classified this compound as having the capacity to produce cancer in humans (Preus et al. 2003). In this con-text, the NIOSH proposes an exposure limit of 10 ppm for no more than 8 hours because of the effects that this compound generates problems in acute exposures such as headaches, loss of appetite and nausea. However, exposure to this compound has also been reported to cause corneal damage, optic neuritis and even kidney damage, while ingestion of large amounts of naphthalene can cause severe hemolytic anemia. While the target organs affected are the eyes, skin, blood, liver, kidneys and central nervous system. On the other hand, the lethal dose reported in hu-mans is 50 mg/kg so the main protective mea-sures are focused on protecting these tissues to avoid inhalation or ingestion of these compounds in some type of personal protective equipment in the working population (NIOSH 2011; NIOSH 2019) However, this happens in controlled and well-regulated occupational environments. In the context of the Tocoy community, or as in precari-ous jobs, the population does not have the nec-essary protective measures, so exposure to this compound is unavoidable in these environments, which can cause adverse health effects. In addi-tion, the actual exposure is not known because indoor air quality monitoring has not been car-ried out. Experimental studies in animal models have reported that exposure to this compound increases the incidence of cancer-related mainly to the respiratory tract. For this reason, the IARC has classified this compound as possibly carci-nogenic to humans (Group 2B) (Yost et al. 2021). It is necessary to implement reference levels, as well as to better understand the consequences of chronic exposure to naphthalenes, and thus better estimate the actual exposure risk to which this population is exposed to provide a more complete picture of the health status of indigenous peoples and their quality of life. In a study conducted by Riojas-Rodríguez et al. (2011) where the authors also found that in the 10 hydroxylated metabolites that were evaluated in this study, such concen-trations decreased when implementing the use of Patsarístoves, which by design, decrease the exposure of these pollutants, so the implemen-tation of strategies such as these, can reduce exposure to PAHs and other pollutants in the air, contributing to the improvement of health and quality of life of these populations.
Respect the IS, toxin this accumulates throughout the progression of CKD, it may indicate disease progression. Unfortunately, there are still no reference values for this biomarker, so the results of this work are compared with other studies in clinical settings. A study by Wang et al. (2019) where IS levels were evaluated in different groups to investigate their relationship with mortality in the first 90 days of an acute kidney infection, revealed that biomarker levels were higher in patients with CKD (3070 ± 301pg/L) than those with hospital-acquired infections (2704 ± 750 pg/L); however, these levels in persons with infections were also higher than in healthy persons (1730 ± 110 pg/L), which can be interpreted that, at higher IS con-centrations, renal damage could be greater. In this study, the mean IS in the population was found to be 193.4 ± 91.85 pg/L which does not exceed the values of healthy subjects reported in these studies. In another study conducted by Cheng-Jui et al. (2011) where they measured the levels of Indoxyl Sulfate and cresyl sulfate in patients with different stages of CKD, the authors found that these two uremic toxins increased gradually as renal function declined; among the IS values reported were, Stage 3: 3200 ± 3000 pg/L; Stage 4: 5400 ± 3600 pg/L; Stage 5: 19,900 ± 10,500 pg/L; Stage 5 with patients on hemodialysis: 42500 ± 15600 pg/L. As can be observed, toxin values increased as the disease progressed, as did cresyl sulfate. This is of concern as the accumulation of various uremic toxins can lead to adverse effects such as mortality from cardiovascular causes and infection events. Since the concentrations in this study are much lower than those compared in the two studies, it could be mentioned that the renal damage in this population is not yet as great as in those studies compared, however, since there are no reference values, it is not possible to indicate with certainty that the study population do not present or will present some type of renal damage in the future. No correlation was found between IS levels and PAH exposure, however, it does not imply that kidney damage is absent or that the compounds are not related to it. The presence of this uremic toxin means that there is renal dam-age, which worsens as time goes by because its elimination decreases, causing an increase in the risk of suffering some cardiovascular disease, which ends up worsening the state of health of people and increasing the probability of mortality more than 50% of deaths in those patients treat-ed with hemodialysis are due to cardiovascular diseases, while the prevalence of cardiovascular complications is approximately 80% in patients on hemodialysis. As it can be seen, there is a close relationship between these two systems, which could be due to the accumulation of toxins in the body such as IS that cause some complications in the cardiovascular system (Gao and Liu 2017). It has been reported that exposure to these pollut-ants may be related to renal damage, an example is a study conducted by Flores-Ramirez et al. (2021b) also in Tocoy, which revealed a correlation between the hydroxylated metabolites 1-OH-NAP, 2-OH-NAP, 9-OH-NAP, 9-OH-FLU and 4-OH-PHE with 4 biomarkers of early kidney damage that were evaluated in the study, which provides an overview of the damage that the inhabitants of the Tocoy area may be suffering. It is important to mention that it is not enough to evaluate only one PAH at the site, because as mentioned above, there is exposure to different compounds, so it is necessary to perform a broader and more varied analysis that consider a wider range of pollutants. Regarding respiratory health, of the men in the study, 3 obtained non-assessable spirometry. Of the women, 6 presented non-assessable spirometry and 5 presented normal respiratory patterns, which means that they did not present any type of respiratory difficulty at the time of the study, 2 with low restrictions; 2 with middle restrictions and 0 with severe restriction, and 1 below of the limit. On the other hand, it does not mean that at some point in the future they will develop some type of respiratory difficulty due to exposure to wood smoke. Four female participants presented mild or moderate restrictive patterns, this can be caused by several situations, an important one could be the continuous exposure to PAHs pres-ent in wood smoke at the time of cooking and in the future the continuous exposure to these pollutants can aggravate the scenario, causing severe restrictions or even developing respiratory diseases. An important fact to mention is that 100% of this population cooks their food and have a heating system that is based on the combustion of solids such as firewood.
Among the limitations reported for the analysis of the study data, due to the nature of the pilot study (reduced n), it was not possible to establish a correlation between biomarkers of exposure to PAHs, spirometry results and the presence of IS, it is recognized that a greater number of participants is needed to establish direct causality. Neverthe-less, this study corroborates the application of various biomarkers for the accurate assessment of PAH exposure and biomarkers of effect such as IS, which can describe renal damage, as well as respiratory assessment.
The scenario of the population of Tocoy is difficult, on one hand, people are exposed to different types of threats ranging from physical pollutants from biomass smoke such as PM 10 and 2.5, and soot, which, along with these, come to some chemi-cal pollutants such as PAHs and other air pollutants present in indoor air, some pesticides from the use of these in agriculture, as well as some mycotoxins. These have different sources such as food contaminated by these mycotoxigenic fungi, without taking into account other possible pathogenic agents that can be harbored in food, air, water and soil, which end up causing chronic exposure through the three existing routes of ex-posure such as inhalation of particles and atmo-spheric pollutants, consumption of contaminated food, water that is often unhealthy and could be contaminated by microorganisms capable of causing diarrheal infections, inhalation and ingestion of dust particles that can bring with them different threats. Indigenous communities face various problems, from scarcity of resources to polluted environments, which undermine the development of these peoples, forcing them to migrate in search of better opportunities, language barriers, as well as poor access to the internet and education. Although there are health centers that have free diagnostic services, these are mainly located in urban centers, far from remote communities such as Tocoy, which means that people must pay for transportation, food and lodging expenses that many cannot afford, causing people to consciously or unconsciously ignore the risks to which they are exposed, normalizing situations that are af-fecting their health and quality of life.
Conclusión
The results of this study have shown that exists a chronic exposure to PAHs, among other pollutants present in the air due to traditional meth-ods of cooking. Since the population of Tocoy is constantly exposed to indoor air pollution, it is necessary to monitor air quality to know the exact concentration to which these residents are exposed. Regarding IS levels, there are no ref-erence values for this biomarker in this type of population, more studies are needed to establish cut off points and use it as a more practical, ac-cessible and accurate method for the evaluation of renal damage and its progression. Besides, for the evaluation of respiratory function, further studies are needed, since the toxic potential of biofuel smoke is known to cause exposure to different pollutants such as PAHs and PM 10 and 2.5, which are known to affect mainly the respiratory tract. It is necessary to address these issues since the life quality of the population is being affected, which could cause probable illnesses in the future, or aggravate some that are already present in the population. There is a risk that people's health could be affected due to constant exposure. The community of Tocoy is abandoned, far from cities that have health centers, and the socio-economic situation of the inhabitants is not the best either, as they are highly marginalized and have precari-ous socioeconomic conditions, in addition to the accumulated risks caused by mixtures of con-taminants such as metals, aflatoxins, pesticides, pesticides and other pollutants, aflatoxins, pesticides or persistent organic compounds, pandemics such as COVID-19 and the prevalence of different non-communicable diseases that tend to affect the health of the ecosystem and the inhabitants (Díaz de León-Martínez et al. 2021a). Therefore, it is necessary to propose new monitoring strate-gies that help in the early detection of diseases, as well as environmental health diagnostics and studies aimed at environmental problems such as air monitoring, water quality studies, among others. The present work serves as a pilot study to support the next studies to be carried out in this community or in communities that have similar conditions to those of Tocoy, which use traditional cooking and heating methods. The present study has background information on the evaluation of respiratory and renal health as well as exposure to different PAHs and provides a general overview of the situation faced by the community that may be affecting its development. This will allow us to know broadly what the challenges are, and subsequently propose comprehensive interven-tions that will benefit the environment and also the health of people, as well as propose programs and policies in these areas that contribute to access to a healthy environment and decent health, thus ensuring access to these human rights and contributing to achieving sustainable develop-ment goals, thus improving the quality of life of the community with a sustainable approach and a healthy environment.
Acknowledgements
COPOCYT. Fideicomiso 23871 Multas Electorales Convocatoria 2021-01, Desarrollo y evaluación de un Sistema de tamizaje basado en la metabolómica exhalatoria para la clasificación y predicción de COVID largo mediante métodos de aprendizaje automatizado. Addressing the cumulative risk from emerging biological, chemical and social threats that will exacerbate the second outbreak of COVID-19 of CEEPAC/UASLP 2020.
Recibido 27/04/2022
Aceptado 08/06/2022
Editores: Susana García y Laura Lanari












 uBio
uBio