Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Insuficiencia cardíaca
versão On-line ISSN 1852-3862
Insuf. card. vol.13 no.1 Ciudad Autónoma de Buenos Aires mar. 2018
ORIGINAL ARTICLE (Original version)
Outpatient disease management program for heart failure: a multidisciplinary approach with an ambulatory intravenous diuretic therapy
Pedro Zuzarte1,3 , Kari Kostiw1, Malgorzata Maciukiewicz2, Maria L. Figueira3, Atilio Costa-Vitali1
1 Heart Failure Disease Management Program. Division of Clinical Sciences at Northern Ontario Medical School. Health Sciences North. Sudbury. Ontario. Canada.
2 Pharmacogenetics Research Clinic. Centre for Addiction & Mental Health. University of Toronto. Toronto. Ontario. Canada.
3 Faculty of Medicine. University of Lisbon. Lisbon. Portugal.
Institution: Heart Failure Disease Management Program. Health Sciences North. Sudbury. Ontario. Canada.
Corresponding author: Atilio Costa-Vitali, MD.
Heart Failure Disease Management Program, Health Sciences North, Sudbury, Ontario, Canada. Tel.:+1-705-523-7100 Ext.: 3663; fax: +1-705-523-7081
E-mail: acostavitali@hsnsudbury.ca
Received: 11/19/2017
Accepted: 02/09/2018
Summary
Aims. Heart failure (HF) is one of the most common causes of hospitalization, has high mortality and represents an economic burden. The Heart Failure Disease Management Program (HFDMP) at Health Sciences North (HSN) was designed and implemented utilizing various outpatient strategies aimed to help patients avoid emergency department (ED) visits, lower HF hospitalizations, improve outcomes, decrease mortality and lower health care costs. This study was designed to evaluate the effectiveness and safety of this program.
Methods and results. 138 patients were enrolled in the HFDMP over a period of 12-months. Patient outcomes, admission, readmission and mortality rates were observed to determine the safety, efficacy and the costs associated. Of the patients treated for acute decompensated HF (ADHF) 29 patients received 79 continuous intravenous furosemide therapy (infusions). These patients were monitored for electrolyte changes, ED visits and hospitalizations to determine the safety and efficacy of the infusion clinic (IC). During the period of study NT-proBNP, eGFR and ejection fraction among other variables were analyzed. Only five readmissions within 30 days were noted over 12 months however, none of these hospitalizations was related to ADHF. The programs mortality rate was 3%. No patient subjected to infusions required an ED visit or hospitalization. No clinical significant electrolyte changes was seen requiring hospitalization.
Conclusions. The findings from our study suggests that this outpatient approach is a safe way to manage ADHF and an effective way to avoid ED visits, lower HF hospitalizations, decrease mortality, improve clinical symptoms and lower health care utilization costs.
Keywords: Heart failure; Outpatient; Management; Hospitalization; Readmissions; Mortality; Diuretic therapy
Resumo
Programa de tratamento ambulatorial para insuficiência cardíaca: uma abordagem multidisciplinar com uma terapia diurética intravenosa ambulatório
Objetivos. A insuficiência Cardíaca (IC) constitui uma das maiores causas de hospitalização, apresenta uma alta taxa de mortalidade e representa um grande peso econômico para o sistema de saúde. O programa para gestão ambulatória Heart Failure Disease Management Program (HFDMP) em Health Sciences North (HSN), Sudbury, Canadá, foi estabelecido utilizando várias estratégias ambulatórias com destino a evitar a necessidade de uso de serviços de urgência (SU) e diminuir hospitalizações por episódios de insuficiência cardíaca aguda descompensada (ICAD) com o objetivo de melhorar resultados clínicos, diminuir mortalidade e baixar o custo econômico na gestão de pacientes com IC. Este estudo foi desenhado para avaliar a eficácia e segurança deste programa.
Métodos e resultados. 138 pacientes entraram no programa HFDMP durante um período de 12 meses. Resultados clínicos e analíticos foram recolhidos durante este estudo, incluindo taxas de hospitalização, readmissão e mortalidade para determinar a segurança e eficácia do programa, assim como os custos associados a esta gestão. Durante o período em estudo 29 pacientes com episódios de ICAD receberam 79 infusões continuas com furosemida endovenosa em ambulatório (Infusões). Estes pacientes foram monitorizados para alterações eletrolíticas durante os procedimentos. Foi registrado a necessidade de encaminhamento para SU e hospitalizações para determinar a segurança e eficácia da clínica de infusão ambulatória. Foram analisados níveis de NT-proBNP, taxa de filtração glomerular (TFG) e fração de ejeção (EF), além de outras variáveis. Apenas 5 readmissões em 30 dias ocorreram nos pacientes do HFDMP durante o estudo, contudo, nenhuma destas hospitalizações se deveram a ICAD. A taxa de mortalidade no programa foi de 3%. Nenhum paciente submetido a Infusão ambulatória por ICAD necessitou transferências para SU ou admissão hospitalar. Nenhuma alteração eletrolítica significativa foi notada ou requereu hospitalização como resultado das infusões ambulatórias.
Conclusões. Este estudo sugere que a abordagem ambulatória do programa HFDMP como resposta a ICAD é segura e representa uma forma eficaz de evitar visitas ao SU, baixando hospitalizações e a mortalidade nestes pacientes enquanto melhora indicadores clínicos e baixa custos de gestão.
Palavras-chave: Insuficiência cardíaca; Ambulatório; Gestão; Hospitalização; Readmissões; Mortalidade; Terapia diurética
Introduction
Patients with heart failure (HF) are typically adults with multiple concurrent diagnoses, complex drug regimens and significant disease management challenges1. Approximately seven million North-Americans2, 4.2 million South Americans3 and 15 million Europeans4 are living with HF: one of the most common causes of hospitalization and readmission worldwide5. In Canada, hospital readmission rates for HF remain high at approximately 9% at 30 days and 15% at 90 days6. It is estimated that readmission rates cost the Canadian healthcare system as much as $1.8 billion per year7 and that up to 59% of those readmissions could have been avoided by improving the care patients receive before and after discharge.
In response to the burden of care as it relates to repeated hospital readmissions and emergency department (ED) visits due to acute decompensated heart failure (ADHF), there have been several publications with regards to strategies that address the post-hospitalization needs of patients and their ability to mitigate readmission risk8. HF management programs vary in complexity and models9,10. Currently, there is no clearly defined model to achieve the best possible clinical outcomes and decrease the cost of the burden of care. Characteristics of the most effective programs have been identified but are extremely broad11-13. Furthermore, evidence of the effectiveness and safety of the use of IV diuretic therapy in a non-emergency setting is still very limited8,14 and requires further investigation.
The Heart Failure Disease Management Program (HFDMP) at Health Sciences North (HSN) was developed as an outpatient strategy aimed to reduce hospitalizations and re-hospitalizations, ED visits and improve clinical outcomes. This programs model was established combining several successful strategies reported in the literature for HF management, including an infusion clinic (IC) so that patients in ADHF may receive continuous intravenous (IV) diuretic therapy (infusions) for symptomatic volume overload who would otherwise have had to visit an ED or be admitted to the hospital.
This work aims to describe the HFDMP approach to outpatient management of HF. We intend to determine indicators of effectiveness of the HFDMP including the safety and efficacy of the IV diuretic component of the program. Specifically, we intend to determine the ability of HFDMP to manage acutely decompensated episodes of HF in an outpatient setting, while at the same time decreasing the need for patients to visit the ED and thereby decreasing admissions and readmissions rates while cutting health care related expenditures and improving patient outcomes. Furthermore, we aim to determine if the IC is a safe way to manage ADHF with the use of IV diuretic therapy in an outpatient setting.
Methods
Study population
Study population consisted of patients referred to the HFDMP at HSN between July 2012 and July 2013. Subjects admitted to the HFDMP were HF patients at high risk of hospitalization. These patients were referred from general practitioners, cardiologists or other clinicians. There were no restriction criteria for referral to this program. All patients referred and enrolled in the program during the period of study were included in this analysis. No sample size calculation was used since there was no restriction to the number of patients to include in this programs 12-month evaluation. Subjects included were only limited to the total number of patients enrolled in the HFDMP in that year.
All patients had a diagnosis of chronic HF - according to the Framingham criteria15; and were classified according to functional capacity (NYHA) and limited to those that continued their treatment in HFDMP during the entire period of the study. Those who only attended the initial visit and did not attend subsequent scheduled visits were excluded. No other exclusion criteria were applied for this analysis.
To assess the effectiveness of the HFDMP, we have compared both the HFDMP and HSNs admission, readmission and mortality rates as well as patient outcomes for the same period. Finally, patients included were divided into two groups according to the treatment modality they underwent in the program: infused group (those that during the study had symptomatic volume overload, signs and symptoms of ADHF and required intervention with IV diuretic therapy); and non-infused group (patients treated in the program that did not require IV diuretic therapy during the same period). This was aimed to determine the safety and efficacy of the different treatment approaches provided by the program. This study complies with the declaration of Helsinki; the appointed ethics committee has approved the research protocol (#930).
Clinical intervention
The HFDMP at HSN consisted of a multidisciplinary program for outpatients at high risk of hospitalization. Patients included received at their first visit a thorough clinical assessment by a cardiologist. Medical management of the patient included up or down titration of medications according to evidence-based guidelines; medication reconciliation, self-care education and support for patients and their families, psychosocial care, advanced care planning and palliative care. Other features of the program included telemonitoring, nurse-led telephone-based chronic care services for symptom monitoring and management, medication counseling, health education and self-care coaching, ongoing assessment of maximal exercise capacity and functional capacity, peak VO2, six-minute walking tests, sleep apnea testing, assessment of cardiac function and referral to cardiac and pulmonary rehabilitation. Selfcare for HF encompasses a spectrum of behaviours ranging from adherence to medication, exercises, diet recommendations, recognition of early warning signs of HF, what to do and when to call the HFDMP. The ability of patients and families to be able to call the clinic at any time to discuss concerns is considered a key component of this program.
Infusion clinic
During the period of this study if a patient had complaints of weight gain, increased dyspnea, cough, orthopnea or paroxysmal nocturnal dyspnea (PND) and/or increased edema, the patient was instructed to up-titrate their oral loop diuretic for 24-48 hours and an appointment was booked within that timeframe in the HFDMP. If the patient experienced ongoing signs and symptoms of ADHF, the patient was instructed to report in to the HFDMP for evaluation and treatment (infused group). Patients were given an IV bolus of a loop diuretic followed by a continuous infusion. After the patients treatment, a decision was then made whether the patient would return the following day for continued IV loop diuretic treatment or be seen in the program for ongoing follow up. Patients requiring more than one day of IV diuretic therapy were discharged home at the end of the day and asked to return to the HFDMP the following day for ongoing treatment and monitoring. All treatments included IV furosemide with an initial bolus dose of 40 - 100 mg over 10 minutes followed by a continuous IV infusion rate between 10 - 40 mg/ hr. The dosage administrated was determined based on the estimated glomerular filtration rate (eGFR) of the patient. Depending on the patient specific diuretic needs, patients might have also received metolazone concomitantly. The duration of the continuous IV infusion typically lasted six to eight hours.
Outcome data collection
Outcome measures were collected for each patient at baseline, 30 days, 3 and 6 months after enrolment in the program. The clinical characteristics, lab values and other variables of patients included in the study both pre-and post intervention were collected. The changes over time in selected variables, such as ejection fraction (EF), N-Terminal Pro B Natriuretic Peptide (NT-proBNP), eGFR, sodium (Na+), potassium (K+) and creatinine (Cr) were documented. Data collection also included the number of ADHF episodes, number of visits to the ED for any reason, HF admissions, 30-day readmission rates and mortality rates during the period of study. ED rates, HF readmission and admission rates as well as mortality rates were also collected for HSNs HF patients not attending the HFDMP from the Electronic Medical Record (EMR).
Safety and efficacy of the infusion clinic
Through the use of the IC we hoped to eliminate the need for ED visits and subsequent hospitalizations in patients actively enrolled in HFDMP. To evaluate the efficacy of the IC we have documented the number of patients that received continuous IV furosemide therapy during the period of the study. We have determined the number of infusions these patients received and calculated the number of ED visits and/or hospitalizations that were avoided through this method. One episode of ADHF treated in the outpatient setting (with either single or multiple infusions) and subsequent discharge home without having to be admitted or attend an ED, was considered one ED/hospitalization avoidance. The admission and readmission rates for ADHF for patients enrolled in the HFDMP were determined, and compared to HSNs admission and readmission rates for patients not attending the program, in the same period.
To evaluate the safety of the IC we recorded pre and post intervention changes in creatinine, sodium and potassium levels before and after each infusion. Adverse reactions such as infection at IV site, hypotension, dizziness, tinnitus or hearing impairment as well as any other complications were documented to determine the safety of this treatment approach. Urine output was measured non-invasively or invasively for all patients. Finally, the number of patients that required transfer to ED and/or admission after treatment in the IC was determined.
Statistical analysis
Descriptive and inferential statistics were used to explore the relationship between the independent and dependent variables. Chi-square was used for categorical variables and one-way ANOVA for continuous variables. Timedependent morbidity and mortality data of the 138 patients was used to construct Kaplan-Meier eventfree survival curves for the sample set. Analysis were conducted using SPSS (v17). Statistical significance was set at p<0.05.
Results
1- Demographics and clinical characteristics of patient groups
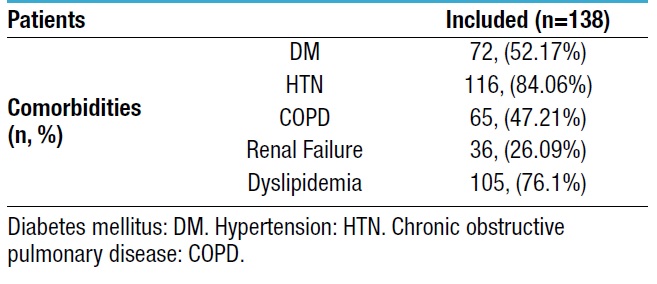
A total of 167 patients were referred to the HFDMP during the period of this study. After the initial assessment, 29 patients did not return for any subsequent visits and were excluded from the study. The main reasons patients did not continue with HFDMP were personal preference and wanting to continue treatment with their usual cardiologist, and/or patients lived too far from the clinic. Therefore, a total of 138 patients were followed by the HFDMP program for at least 12 months and were included in the analysis. Patient demographics and clinical characteristics at enrolment (T1) can be found in Table 1. The mean age of included patients was 74.6 years; 50% (n=69) of patients had reduced EF [left ventricular ejection fraction (LVEF) ≤40%] at enrolment. The NYHA functional classification of patients was as follows: Class I 7.9% (n=11); Class II 45.7% (n=63); Class III 43.5% (n=60) Class IV 3% (n=4) at T1. Participant comorbidities can be found in Table 2. The most common comorbidities were as follows: 84.1% (n=116) hypertension, 76.1% (n=105) dyslipidemia and 52.2% (n=72) had type II diabetes, 26.9% (n=36) had chronic kidney disease.
Table 1. Characteristics and demographics of patients

Patients characteristics at baseline (baseline or T1: moment of enrolment in the HFDMP). *HF Type/Etiology: data missing for 5 excluded patients;
**NYHA: data missing for 4 excluded patients. Percentages in table are computed using whole sample as reference for each group: overall
(n=167), patients included (n=138) and patients excluded (n=29). Heart Failure Disease Management Program (HFDMP).
Table 2. Patients comorbidities
Twenty-nine patients were treated with intravenous diuretic therapy in the IC during the period of this study (infused group). The remaining 109 patients were followed in the HFDMP during the study and did not require an infusion (non-infused group).
2- Safety and efficacy of the HFDMP
2.1- Infusion clinic
Of 138 patients followed in the HFDMP during the 12 month period, 29 patients (infused group) received outpatient continuous intravenous furosemide therapy for ADHF. A total of 79 infusions were done on these patients. All patients experienced relief of their symptoms and reported an overall improvement in their dyspnea. All patients were discharged from the IC to their homes after treatments. No patient that attended the IC required transfer to the ED or admission to the hospital for their ADHF episode.
2.2- Safety of the infusion clinic
No incidence of clinically significant electrolyte disturbances was noted for the patients that attended the IC. There was no ED visits or admissions as a result of the infusion treatment in the IC. Renal function values were obtained before and after each infusion. No significant change was seen in the measured variables in all the treatments performed as seen in Figure 1.

Figure 1. Variations in patients sodium (Na+) (A), potassium (K+) (B) and creatinine (Cr) (C) before and after infusion therapy in the outpatient infusion clinic (infused patient group).
2.3- EF, NT-proBNP and eGFR assessments
Changes in clinical indicators with progression of treatment in the program can be seen in Figure 2. Notably, the levels of NT-proBNP for all patients at time of enrolment (T1) in the program was 3214 ng/L. Three months after enrolment (T2) there was a significant decrease in the levels of NT-proBNP to 2109 ng/L (p<0.05). In the non-infused group, NT-proBNP at baseline was 3072 ng/L and decreased to 2124 ng/L (p<0.05) for the same period. For the infused group, NT-proBNP levels were 3772 ng/L at baseline and a decrease to 2056 ng/L (p<0.05) was found at 3 months post intervention. The mean EF in the infused group was 42% at T1 and increased to 58% at 3-6 months post intervention. The mean EF for the non-infused group was 43% at baseline and increased to 51% in the same period. Finally, the eGFR of the infused group was 45 mL/min at baseline and remained relatively stable (48 mL/min) 3 months post intervention. As for the noninfused group, eGFR decreased from 47.5 mL/min at baseline to 43.5 mL/min with no clinical significance.
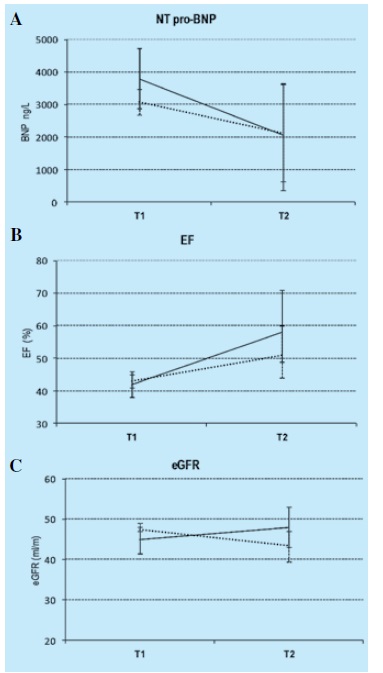
Figure 2. Changes over time in patients clinical indicators with progression of treatment in the Heart Failure Disease Management Program (HFDMP).
Solid line: infused patient group. Dotted line: non-infused patient group. T1: moment of enrolment in the HFDMP. T2: 3-6 months after enrolment in the HFDMP.
NT-proBNP: N-Terminal Pro B Natriuretic Peptide. EF: ejection fraction. eGFR: estimated glomerular filtration rate.
2.4- Distribution of admissions and re-admissions
From July 2012 to July 2013 the total number of hospitalizations at HSN with a primary diagnosis of HF was 295. Of 295 admissions, 18 admissions were patients from HFDMP and 277 admissions were from patients not enrolled in the program. In the same period, there were 60 readmissions within 30 days at HSN; 5 of which were patients enrolled in the HFDMP. Of the 55 readmissions for patients not attending the HFDMP, 20 were HF related. Notably, of the 5 readmissions for patients enrolled in the program, zero was due to ADHF.
2.5- Mortality
Mortality rate for the HFDMP was 3% (4/138) during the 12-month period of follow-up. One patient (0.7%) had a cardiovascular related cause of death (Table 3). We have determined the mortality rate and causes of death for the excluded patients from this study (n=29), identified by HSN´s electronic medical records. For these patients, 21% (n=6) died in the same period of the study and 14% (n=4) experienced a cardiovascular related cause of death.
Discussion
Heart failure has a significant impact on patients lives and is responsible for high costs within our healthcare system. This problem needs to be addressed with more effective treatment approaches. Data obtained from the Decision Support department at HSN states that between 2006-2012 the 30-day HF readmission rate was 30% at HSN. This figure is over the international reported average 16. The average length of stay at HSN for a patient admitted with HF is 10.8 days, equating to approximately $1000/day17, which translates into a considerable high burden of healthcare costs for this patient population. The introduction of the HFDMP at HSN was an attempt to address this problem. Although, there are several studies on HF disease management programs and clinics12,18 there still exists a lack of published standards/guidelines on care processes and structural elements of such programs. Our program was established following HFSA19 and ACC/AHA20 guidelines and in line with the European Society of Cardiology11 (ESC) recommendations for HF clinics. However, all recommendations do not provide specific details about the characteristics of the clinics themselves. We decided to incorporate in our programs model several combined approaches for HF management as reported in the literature. Such considerations should be a cardiologist to help manage care21,22, telemonitoring23, and the implementation of outpatient diuretic therapy clinics for the treatment of ADHF24,25.
Improved patient outcomes were demonstrated when a cardiologist participates and leads the management of treatment for a patient in a HFDMP21. In the HFDMP there is a lead cardiologist. This standard of care has proven to be particularly significant when there is a close interaction between the HFDMP and the primary care physician (up to 40% reduction in mortality, or mortality combined with hospitalization) when compared to patients that were managed solely by their primary care physician22.
We have incorporated telemonitoring23 for patients who have difficulty accessing specialized care because of geography, transportation, or infirmity26. Studies have demonstrated that isolated telephone-based care services in HF populations does not help to decrease the rate of readmission or death when compared with usual care (HF programs without telemonitoring)27,28. Telemonitoring improves patient outcomes significantly in HF populations when provided in the context of a broader disease management program29, which is one of the guiding principles of our program.
The ability to provide outpatient intravenous diuretic therapy is a key element in the HFDMP. The IC allows an alternative to hospitalization for the treatment of patients with ADHF. Although innovative and potentially effective, the safety of providing IV diuretic therapy in an outpatient setting (and discharging patients home the same day) needs to be further investigated. Additionally, this study sought to evaluate the programs ability to improve patients clinical indicators over time, to determine the safety and efficacy of this model of care and whether a combination of strategies to try and reduce ADHF would lower HF mortality, prevent ED visits for ADHF and lower admission and readmissions rates.
The safety and efficacy of the patients in the HFDMP (infused or not) maintained a stable eGFR over time, % of EF improved, and NT-proBNP values decreased over time.
Patients who required IV loop diuretics (infused group) had the best response to the treatment. Our results demonstrated that the use of IV loop diuretics (with or without metolazone) was effective in reducing edema and dyspnea without negatively affecting electrolyte balance in an outpatient setting. No significant adverse effects were noted in our study when patients were infused in the IC. Of note, when we looked at all HF admissions at HSN, 30-day readmission for all causes and 30-day readmission with a primary diagnosis of HF at HSN, there was evidence to support that the IC at the HFDMP had a positive impact on decreasing ED visits and admissions. Only a small percentage of all HSN´s HF admissions and 30-day readmission rate were for patients enrolled in the HFDMP (18/295 admissions and 5/60 readmissions within 30-days). Furthermore, the program did not have a single 30-day readmission due to ADHF (0/5), compared to 33% (20/60) readmissions with a primary diagnosis of HF for patients not attending the program. We consider this to be a strong indicator that utilization of the HFDMP has a potential to decrease ED visits, admissions and readmissions and decrease healthcare utilization costs.
Despite advances in HF management, mortality associated with this disease remains high. The estimated 1-year mortality varies between 20 to 30%30 while other reports cite an estimate of 1-year mortality at 11%31. The 1-year mortality rate for patients enrolled in the HFDMP was calculated to be 3% for all causes. Furthermore, only a single case was related to a cardiovascular cause of death. The mortality rate for patients that were not included in our study (patients assessed at baseline in HFDMP but lost to follow-up) was 21% for the same period, which is comparable to the international reported average for 1-year HF mortality rates30. Furthermore, in these patients 14% died from cardiovascular related causes. Although a direct comparison of these figures have several limitations, our study suggests that the mortality rates of patients enrolled in the HFDMP were significantly lower compared to those patients who were lost to follow-up. The same can be said about the program´s effect on decreasing the burden of health care costs. Although this study was not designed to measure cost savings for the hospital as it relates to the burden of care for HF, the data would suggest that the program had a positive impact on cost savings for the hospital by reducing HF admissions and readmissions and by decreasing the average length of stay. Based on the aforementioned data above we could infer that the HFDMP may have saved over one million dollars. However, this would need to be further verified through specific case costing data.
Conclusions
All these indicators show that this multidisciplinary model for HF management, including the infusion clinic appear to be a safe, efficacious and cost-effective program when compared with current HF standards (ED and inpatient treatment for patients with HF requiring diuretic therapy) and other HF clinic models. The infusion of loop diuretics to HF patients in an outpatient setting is an effective and well-tolerated treatment option for patients but also plays a role preventing unnecessary ED visits and hospital admissions and readmissions. The cost savings based on the number of HF admissions in a given year, length of stay and average cost per patient admission is substantial. Lastly, the open access granted to patients to be able to speak to someone in the HFDMP in a timely fashion allows patients to be triaged, assessed and managed safely and efficaciously in an outpatient setting prior to an acute decompensation requiring an ED visit or hospital admission. We believe this aspect to be one of the cornerstones of the success of the HFDMP.
The findings of the present study also has its limitations. This is a single-center experience; therefore, the findings may not be generalized to other HF populations. Comparisons of the mortality rates between included and excluded patients have to be interpreted as indicative (and not conclusive) since variables were not under control for the excluded patients. Regardless of these aspects, our data suggests that the HFDMP at HSN is considered to be safe and provides an alternative solution for ADHF management outside of inpatient hospital settings. Furthermore, this study has demonstrated that this model of care could provide an effective way of avoiding unnecessary emergency visits and hospitalizations with important cost saving implications.
Acknowledgments
A.C.V., P.Z and K.K. designed the study. A.C.V is director of the HFDMP and responsible for the project and. P.Z. and K.K. collected the data. P.Z, A.C.V. and M.C. analyzed the data. P.Z. and A.C.V prepared the manuscript and all authors edited and approved the manuscript.
Funding
This study was supported by the Academic Health Sciences Centre (AHSC) Alternative Funding Plan (AFP) Innovation Fund of the Northern Ontario Academic Medicine Association (NOAMA), Canada [NOAMA A-1301].
Conflict of interest
The authors declare no conflict of interest.
1. Wong CY, Chaudhry SI, Desai MM, Krumholz HM. Trends in comorbidity, disability, and polypharmacy in heart failure. Am J Med 2011;124(2):136-43. [ Links ]
2. Ross H, Howlett J, Arnold JM, Liu P, ONeill BJ, Brophy JM, Simpson CS, Sholdice MM, Knudtson M, Ross DB, Rottger J, Glasgow K, Group CCSAtCW. Treating the right patient at the right time: access to heart failure care. Can J Cardiol 2006;22(9):749-54. [ Links ]
3. Ciapponi A, Alcaraz A, Calderón M, Matta MG, Chaparro M, Soto N, Bardach A. Burden of Heart Failure in Latin America: A Systematic Review and Meta-analysis. Rev Esp Cardiol (Engl Ed) 2016;69(11):1051-60. [ Links ]
4. Roccaforte R, Demers C, Baldassarre F, Teo KK, Yusuf S. Effectiveness of comprehensive disease management programmes in improving clinical outcomes in heart failure patients. A meta-analysis. Eur J Heart Fail 2005;7(7):1133-44. [ Links ]
5. Krumholz HM, Normand SL, Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke, 1999-2011. Circulation 2014;130(12):966-75. [ Links ]
6. Johansen H, Strauss B, Arnold JM, Moe G, Liu P. On the rise: The current and projected future burden of congestive heart failure hospitalization in Canada. Can J Cardiol 2003;19(4):430-5. [ Links ]
7. Monette M. Hospital readmission rates under the microscope. CMAJ 2012;184(12):E651-2. [ Links ]
8. Stauffer BD, Fullerton C, Fleming N, Ogola G, Herrin J, Stafford PM, Ballard DJ. Effectiveness and cost of a transitional care program for heart failure: a prospective study with concurrent controls. Arch Intern Med 2011;171(14):1238- 43. [ Links ]
9. Whellan DJ, Hasselblad V, Peterson E, OConnor CM, Schulman KA. Metaanalysis and review of heart failure disease management randomized controlled clinical trials. Am Heart J 2005;149(4):722-9. [ Links ]
10. Holland R, Battersby J, Harvey I, Lenaghan E, Smith J, Hay L. Systematic review of multidisciplinary interventions in heart failure. Heart 2005;91(7):899-906. [ Links ]
11. McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, Guidelines ECfP. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 2012;33(14):1787-847. [ Links ]
12. Hauptman PJ, Rich MW, Heidenreich PA, Chin J, Cummings N, Dunlap ME. The heart failure clinic: a consensus statement of the Heart Failure Society of America. J Card Fail 2008;14(10):801-15. [ Links ]
13. McAlister FA, Stewart S, Ferrua S, McMurray JJ. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomized trials. J Am Coll Cardiol 2004;44(4):810-9. [ Links ]
14. Hebert K, Dias A, Franco E, Tamariz L, Steen D, Arcement LM. Open access to an outpatient intravenous diuresis program in a systolic heart failure disease management program. Congest Heart Fail 2011;17(6):309-13. [ Links ]
15. McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Engl J Med 1971;285(26):1441-6. [ Links ]
16. Gheorghiade M, Pang PS. Acute heart failure syndromes. J Am Coll Cardiol 2009;53(7):557-73. [ Links ]
17. HSN. Health Sciences North statistics; Decision support department. 2011. [ Links ]
18. McIntyre HF, Barrett J, Murphy S, Wray R, Sutcliffe SJ, Walker DM. Across the interface: the hastings heart function clinic. Heart 2002;88 Suppl 2: ii23-7. [ Links ]
19. Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, America HFSo. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail 2010;16(6):e1- 194. [ Links ]
20. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, Foundation ACoC, Guidelines AHATFoP. 2013 ACCF/ AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;62(16):e147-239. [ Links ]
21. Ansari M, Alexander M, Tutar A, Bello D, Massie BM. Cardiology participation improves outcomes in patients with new-onset heart failure in the outpatient setting. J Am Coll Cardiol 2003;41(1):62-8. [ Links ]
22. Indridason OS, Coffman CJ, Oddone EZ. Is specialty care associated with improved survival of patients with congestive heart failure? Am Heart J 2003;145(2):300-9. [ Links ]
23. Clark RA, Inglis SC, McAlister FA, Cleland JG, Stewart S. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. BMJ 2007;334(7600):942. [ Links ]
24. Ryder M, Murphy NF, McCaffrey D, OLoughlin C, Ledwidge M, McDonald K. Outpatient intravenous diuretic therapy; potential for marked reduction in hospitalisations for acute decompensated heart failure. Eur J Heart Fail 2008;10(3):267- 72. [ Links ]
25. Buckley LF, Carter DM, Matta L, Cheng JW, Stevens C, Belenkiy RM. Intravenous Diuretic Therapy for the Management of Heart Failure and Volume Overload in a Multidisciplinary Outpatient Unit. J Am Coll Cardiol Heart Fail 2016;4(1):1-8. [ Links ]
26. Jaarsma T, Strömberg A, De Geest S, Fridlund B, Heikkila J, Mårtensson J. Heart failure management programmes in Europe. Eur J Cardiovasc Nurs 2006;5(3):197-205. [ Links ]
27. Chaudhry SI, Mattera JA, Curtis JP, Spertus JA, Herrin J, Lin Z, Phillips CO, Hodshon BV, Cooper LS, Krumholz HM. Telemonitoring in patients with heart failure. N Engl J Med 2010;363(24):2301-9. [ Links ]
28. Koehler F, Winkler S, Schieber M, Sechtem U, Stangl K, Böhm M, Boll H, Kim SS, Koehler K, Lücke S, Honold M, Heinze P, Schweizer T, Braecklein M, Kirwan BA, Gelbrich G, Anker SD, Investigators T-H. Telemedical Interventional Monitoring in Heart Failure (TIM-HF), a randomized, controlled intervention trial investigating the impact of telemedicine on mortality in ambulatory patients with heart failure: study design. Eur J Heart Fail 2010;12(12):1354-62. [ Links ]
29. Polisena J, Tran K, Cimon K, Hutton B, McGill S, Palmer K, Scott RE. Home telemonitoring for congestive heart failure: a systematic review and meta-analysis. J Telemed Telecare 2010;16(2):68-76. [ Links ]
30. Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KK, Murabito JM, Vasan RS. Long-term trends in the incidence of and survival with heart failure. N Engl J Med 2002;347(18):1397-402. [ Links ]
31. Bleumink GS, Knetsch AM, Sturkenboom MC, Straus SM, Hofman A, Deckers JW, Witteman JC, Stricker BH. Quantifying the heart failure epidemic: prevalence, incidence rate, lifetime risk and prognosis of heart failure The Rotterdam Study. Eur Heart J 2004;25(18):1614-9. [ Links ]















