Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Acta Odontológica Latinoamericana
On-line version ISSN 1852-4834
Acta odontol. latinoam. vol.22 no.3 Buenos Aires Dec. 2009
ARTÍCULOS ORIGINALES
The effect of smoking on gingival crevicular fluid volume during the treatment of gingivitis
Sabrina C. Gomes1,3, Flávia B. Piccinin1, Rui V. Oppermann1, Cristiano Susin2, Rosemary Adriana C. Marcantonio3
1 Department of Periodontology, Universidade Federal do Rio Grande do Sul, Porto Alegre, RS, Brazil
2 Department of Periodontics, Medical College of Georgia School of Dentistry, Augusta, GA, USA
3 Department of Periodontology, UNESP Universidade Estadual Paulista, Araraquara, SP, Brazil
CORRESPONDENCE Sabrina Carvalho Gomes Av. Lageado, 1000/702. Petropolis. 90460110. Porto Alegre, Brazil e-mail: sabrinagomes.perio@gmail.com
ABSTRACT
Smoking is detrimental to periodontal tissues, and periodontal destruction is greater among smokers. Paradoxically, smokers seem to have less gingival bleeding than never-smokers with comparable supragingival plaque. There is scarce information about the impact of smoking on gingival crevicular fluid (GCF) volume. This singlearm study clinical trial assessed the effect of smoking on GCF volume during the treatment of gingivitis. The sample included 24 never-smokers (47.3 ± 6.7 years old, 41.7% males) and 21 smokers (45.8 ± 5.1 years old; 55% males; 19.6 ± 11.8 cigarettes/day; 24.1 ± 8.7 years of smoking) with gingivitis and chronic periodontitis. After baseline supragingival scaling, patients received oral hygiene instructions weekly for 180 days. Participants were examined at baseline, 30, 90 and 180 days, and gingival bleeding index (GBI), bleeding on probing (BOP), periodontal probing depth (PPD) and GCF volume were recorded. Statistical analysis was performed using linear models (Wald test, p<0.05%). Smokers had significantly smaller GCF volumes than never-smokers. This finding was not attributed to GBI, BOP or PPD. Higher volumes of GCF were significantly associated with deeper pockets. GCF was significantly reduced throughout the study for both smokers and never-smokers, and the largest reductions were seen at 30 days. Smoking affected the GCF crevicular fluid volume independently of the presence of gingival bleeding, BOP and PPD. Smoking status and PPD should be taken into account when GCG volume and components are under investigation.
Key words: Smoking; Oral hygiene; Gingivitis; Periodontitis; Gingival crevicular fluid.
RESUMO
Efeito do tabagismo sobre o volume de fluido crevicular gingival durante o tratamento da gengivite
O tabagismo e capaz de alterar a resposta periodontal determinando maior expressao de destruicao periodontal em pacientes fumantes. Paradoxalmente, estes pacientes apresentam menos sangramento gengival frente a uma quantidade semelhante de biofilme dental, quando comparados a pacientes que nunca fumaram. Por outro lado, existe pouca informacao sobre o impacto do tabagismo sobre o volume de fluido crevicular gengival (FCG). O presente ensaio clinico de braco unico teve como objetivo avaliar o efeito do tabagismo sobre o volume de FCG durante o tratamento da gengivite. A amostra foi composta por 24 pacientes que nunca fumaram (47.3 ± 6.7 anos, 41.7% homens) e 21 fumantes (45.8 ± 5.1 anos; 55% homens; 19.6 ± 11.8 cigarros por dia; 24.1 ± 8.7 anos de exposicao ao tabaco), com diagnostico de gengivite e periodontite cronica. Os exames periodontais: Indice de Placa Visivel (IPV), Indice de Sangramento Gengival (ISG), Sangramento a Sondagem (SS) e Profundidade de Sondagem (PS) e a coleta de FCG foram realizados nos dias 0, 30, 90 e 180. Apos a raspagem supragengival realizada no dia zero (dia 0), os pacientes receberam instrucao de higiene bucal semanalmente, ate o dia 180. A analise estatistica utilizou modelos lineares (Teste de Wald, p<0.05%). Os fumantes apresentaram um volume significativamente menor de FCG. Este resultado nao esteve associado ao ISG, SS ou PS. Sitios com maiores valores de PS apresentaram maior volume de FCG. Durante o tratamento, uma reducao significante do volume de FCG foi observada em fumantes e pacientes que nunca fumaram. Conclui-se que o tabagismo influenciou o volume de FCG independente da presenca de sinais inflamatorios clinicos e que o habito de tabagismo e a PS devem ser observados quando o volume de FCG e seus componentes estiverem sob investigacao.
Palavras-chave: Tabaco; Higiene bucal; Gengivite; Periodontite; Fluido do sulco gengival.
INTRODUCTION
Smoking is a well-established risk factor for destructive periodontal disease. Epidemiological and clinical studies showed that smokers have deeper periodontal probing depth (PPD) and greater clinical attachment loss (CAL) and gingival recession than never- or former-smokers1-5. Paradoxically, several studies demonstrated that current-smokers have less gingival bleeding than never- and former-smokers6, but there were no differences in bleeding on probing (BOP)7.
Gingival crevicular fluid (GCF) is an inflammatory exudate that results from the interaction between the host and dental biofilms8. GCF volume, the net result of gingival and periodontal inflammatory exudates, has been used to evaluate the inflammatory status of the gingival and periodontal tissues in health and disease9-12. Recent studies demonstrated that GCF volume increases with dental plaque accumulation12,13 and decreases after microbial challenge is reduced or removed14. The effect of smoking on GCF volume has not been consistently studied in the periodontal literature. Some studies raised questions about whether differences observed in GCF between smokers and never-smokers may be attributed to smoking or to confounding factors, such as gingival bleeding and microbiota15-22. This study assessed the effect of smoking on GCF volume in patients undergoing treatment for gingivitis.
MATERIALS AND METHODS
Study design and sample
The present study was a single-arm, 6-month follow- up clinical trial; supragingival plaque control was the intervention, and smoking, the effect modifier21. A consecutive sample of 45 individuals was selected according to smoking status from the pool of patients of the Department of Periodontology, Universidade Federal do Rio Grande do Sul, Porto Alegre, Brazil. Twenty-four never-smokers (47.3 ± 6.7 years old, 41.7% males) and 21 smokers (45.8 ± 5.1 years old; 55% males; 19.6 ± 11.8 cigarettes/ day; 24.1 ± 8.7 years of smoking) fulfilled the following selection criteria and were included in the study:
1. No known systemic disease or previous periodontal treatment;
2. No anti-inflammatory or antibiotic therapy in the previous 3 and 6 months. No pregnancy, hormone therapy or chemical plaque control;
3. At least 12 or more teeth, excluding third molars;
4. At least 4 teeth with one site with periodontal pocket depth (PPD) of 3 to 5 mm and 4 additional teeth with one site with PPD 6 to 10 mm;
5. Availability to return weekly and to be enrolled in a plaque control program.
The study was approved by the Committee on Ethical Affairs of the Universidade Estadual de Sao Paulo, Araraquara, Brazil.
Experimental procedures
All participants underwent strict supragingival plaque control for 6 months. Initially, full mouth supragingival debridement, extraction of hopeless teeth, endodontic treatment, and placement of temporary fillings and crowns were performed. Participants received oral hygiene instructions according to their needs, and supragingival plaque control was evaluated weekly throughout the study. All procedures were performed by three periodontists. Clinical examination A full-mouth, excluding third molars, periodontal examination was conducted at baseline, 30, 90 and 180 days. Gingival bleeding index (GBI), bleeding on probing (BOP) and PPD were recorded. The nearest upper millimeter was used to record PPD. Six sites in each tooth were examined: mesiobuccal, midbuccal, distobuccal, mesiolingual, midlingual, and distolingual. All clinical examinations were performed by one calibrated and blinded periodontist (FP). The unweighted and weighted kappa (±1 mm) values for each site PPD were 0.65 and 0.95.
Gingival Crevicular Fluid sampling
Gingival crevicular fluid (GCF) was randomly collected from 8 sites (1 site per tooth) with visible plaque, gingivitis and chronic periodontitis. Sites were selected according to initial PPD: 4 sites with PPD <6 mm and 4 with PPD >6 mm. After careful removal of all supragingival plaque, teeth were washed with water spray, isolated with cotton rolls and gently dried for 30 seconds. Paper strips (PerioPaper Strips, OraFlow, PlainView, New York, USA) were gently inserted until slight resistance was met, and the strip was kept in the selected site for 30 seconds. GCF volume was measured using a calibrated Periotrom 8000 (OraFlow, PlainView, New York, USA) according to manufacturer’s instructions. Paper strips with traces of blood were discarded. One examiner (SCG) performed all GCF sampling.
Statistical analysis
Raw Periotrom scores were converted to volume of GCF in microliters (μl). Data were normalized using logarithmic transformation. Results were reported as back-transformed values. Linear models were used to estimate GCF volume according to smoking status and study time point. Measurements for each tooth were used, and estimates were adjusted for the clustering of teeth for participants using a robust variance estimator. Wald tests were used for comparisons, and the p-value was adjusted for multiple comparisons (STATA software). The level of significance was set at 5%, and 95% confidence intervals (CI) were calculated. Additionally, generalizing estimating equations were used to model the association between GCF and various factors. An exchangeable correlation structure was used to model correlations within participants.
RESULTS
Never-smokers had significantly greater GCF volumes than smokers, and this difference was constant over 6 months (Table 1). The volume of GCF significantly decreased in both groups along the study. The greatest decrease was found at 30 days. Additional significant, but not substantial, decrease in GCF was observed between 30 and 180 days. The amount of GCF was associated with PPD, and deep pockets had significantly greater amounts of GCF than shallow pockets. After the study time, no differences in mean GCF volume were observed in shallow and moderate pockets (PPD <6 mm) according to smoking status, but never-smokers had a significantly greater GCF volume than smokers in sites with PPD >6 mm (Fig. 1).
Table 1: Mean (CI) gingival crevicular fluid volume in microliters according to study time points and smoking habits.


Fig. 1: Mean gingival crevicular fluid volume in never-smokers (non-smoker) and smokers according to periodontal probing depth at all study time points (baseline, 30, 90 and 180 days). Bars represent 95% confidence interval.
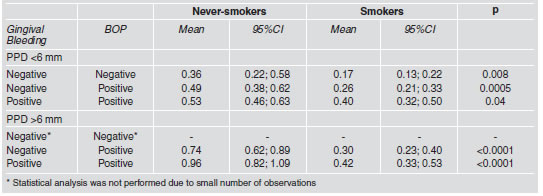
At 30 days, reductions in the GCF volume were associated with a decrease in gingival bleeding and BOP (Fig. 2). Further decrease in GCF was mostly associated with a reduction in BOP only, because gingival bleeding was practically non-existent. Never-smokers had greater GCF volumes than smokers, regardless of presence of gingival bleeding or BOP (Table 2).

Fig. 2: Mean gingival crevicular fluid volume and percentage of sites with gingival bleeding and bleeding on probing at all study time points (baseline, 30, 90 and 180 days). Bars represent 95% confidence interval.
Table 2: Mean values of gingival crevicular fluid volume according to gingival bleeding index, bleeding on probing (BOP) and periodontal probing depth (PPD) for never-smokers and smokers.
The multivariable analysis showed that smoking, gingival bleeding, BOP and PPD were significant independent factors of GCF volume (Table 3). After adjusting for other factors, PPD had the greatest effect on GCF volume, followed by smoking. The magnitude of the effect of gingival bleeding and BOP on GCF volume was similar after adjusting for cofactors.
Table 3: Multivariable longitudinal analysis of the effect of smoking, gingival bleeding, bleeding on probing (BOP) and periodontal probing depth (PPD) on the volume of gingival crevicular fluid volume.

DISCUSIÓN
This study showed that smoking affected the volume of GCF negatively regardless of the presence gingival bleeding or subgingival bleeding (BOP). Smokers and never-smokers had significant reductions in GCF volume during the treatment of gingivitis although smokers had lower GCF values before and at the end of the intervention. The smaller GCF volumes observed among smokers could not be attributed to other factors, such as gingival bleeding, BOP and PPD.
To our knowledge this is the first study to show that smoking affects the volume of GCF regardless of the inflammatory conditions associated with gingival and subgingival bleeding. Other studies showed that smokers had less gingival bleeding than never- or former- smokers23. However, no significant differences have been reported for BOP according to smoking7. These findings may suggest that smoking has a major effect on gingival tissues but not on periodontal inflammation. According to this study, smoking has a detrimental effect on both gingival and periodontal inflammatory parameters in terms of GCF volume. Most of the reduction in GCF volume was found after one month of supragingival plaque control, which may be associated with the decrease in the percentage of sites with gingival bleeding. As gingival bleeding was virtually absent for the remaining time of the study, additional reductions were probably associated with the decrease in BOP and PPD.
Our results showed that the presence of gingival inflammation is associated with increased GCF volume. Consequently, supragingival biofilm control may help to differentiate between GCF volumes found in gingivitis and those found in periodontitis. Gingivitis and periodontitis are currently classified as two different diseases24. The fact that fluid volumes are different in these diseases may be relevant for the analysis of immune-inflammatory markers and indicators. These observations suggest that the recommendation to clearly distinguish between formerand never-smokers when studying the relationship between periodontal diseases and systemic health25 should be expanded to the study of GCF formation and composition. In this regard, GCF volume should be accounted for when investigating the composition of fluid and its impact on etiology, diagnosis and prognosis of periodontal diseases, as suggested by Giannopoulou et al., 200326. The effect of smoking can be better appreciated by the observation that the initial GCF volume at PPD>6 mm sites in smokers was similar to the volume in PPD<6 mm sites in never-smokers. Throughout the study, never-smokers showed a faster volume reduction, although no differences were found at 180 days. The reasons for these findings are unclear, but may be associated with the fact that smokers respond more slowly to periodontal therapy than never- or former-smokers26, 27.
GCF volume decreases after subgingival scaling and root planing28,29. Our results showed that the treatment of gingivitis, based on mechanical supragingival plaque control, yielded significant reductions in GCF volume. This is in accordance with evidence that supragingival control may affect the subgingival environment and lead to a decrease in inflammation and subgingival microbiota21. Smoking affected gingival and periodontal clinical parameters of inflammation negatively. Smokers had significantly lower GCF values than neversmokers at baseline and throughout the study, regardless of gingival bleeding, BOP or PPD. Future studies should take in consideration that GCF volume is associated with smoking status, gingival bleeding, BOP and PPD, and that these variables should be taken into account when GCG volume and components are under investigation.
ACKNOWLEDGMENTS
The authors acknowledge Elcia Silveira and Graziela Benemmann for their clinical support and CNPq (National Research Council, Brasilia, DF, Brazil), CAPES (National Coordination of Post-Graduate Education, Brasilia, DF, Brazil) and FAPESP (Sao Paulo State Research Foundation, Sao Paulo, SP, Brazil) for financial support.
1. Haffajee AD, Socransky SS. Relationship of cigarette smoking to attachment level profiles. J Clin Periodontol 2001;28: 283-295. [ Links ]
2. Albandar JM. Global risk factors and risk indicators for periodontal disease. Periodontol 2000 2002;29:177-206. [ Links ]
3. Susin C, Dalla Vechia CF, Oppermann RV, Haugejorden O, Albandar JM. Periodontal attachment loss in an urban population of Brazilian adults: effect of demographic, behavioral, and environmental risk indicators. J Periodontol 2004;75:1033-1041. [ Links ]
4. Bergstrom J. Tobacco smoking and risk for periodontal disease. J Clin Periodontol 2003;30:107-113. [ Links ]
5. Bajloon M, Natto S, Bersgtrom J. Long-term effect of smoking on vertical periodontal loss. J Clin Periodontol 2005;32:789-797. [ Links ]
6. Bergstrom J, Persson L, Preber H. Influence of cigarette smoking on vascular reaction during experimental gingivitis. Scand J Dent Res 1988;96:34-39. [ Links ]
7. Gomes SC, Oppermann RV, Piccinin F, Susin C, Nonnenmacher CI, Mutters R, Marcantonio RAC. Periodontal status in smokers and never-smokers: clinical findings and Real- Time PCR quantification of putative periodontal pathogens. J Periodontol 2006;77:1483-1490. [ Links ]
8. Griffiths GS. Formation, collection and significance of gingival crevicular fluid. Periodontol 2000 2003;31:32-42. [ Links ]
9. Egelberg J. Permeability of the dento-gingival blood vessels. II. Clinically healthy gingiva. J Periodont Res 1966a;1:276-286. [ Links ]
10. Egelberg J. Permeability of the dento-gingival blood vessels. III. Chronically inflamed gingiva. J Periodont Res 1966b;4:287-296. [ Links ]
11. Rudin H.J, Overdiek HF, Rateitschak KH. Correlation between sulcus fluid rate and clinical and histological inflammation of the marginal gingiva. Helv Odontol Acta 1970;29:21-26. [ Links ]
12. Rudiger SG, Carlen A, Meurman JH, Kari K, Olsson J. Dental biofilms at health and inflamed gingival margins. J Clin Periodontol 2002;29:524-530. [ Links ]
13. Zhang J, Kashket S, Lingstrom P. Evidence for the early onset of gingival inflammation following short-term plaque accumulation. J Clinl Periodontol 2002;29:1082-1085. [ Links ]
14. Trombelli L, Scapoli C, Orlandini E, Tosi M, Bottega S, Tatakis DN. (2004) Modulation of clinical expression of plaque-induced gingivitis. J Clin Periodontol 2004;31:253- 259. [ Links ]
15. Lie MA, Timmerman MF, van der Velden U, van der Weijden GA. Evaluation of 2 methods to assess gingival bleeding in smokers and non-smokers in natural and experimental gingivitis. J Clin Periodontol 1998;25:695-700. [ Links ]
16. Rosa GM, Lucas GQ, Lucas ON. Study of the crevicular fluid flow rate in smokers. Acta Odontol Latinoam 2000; 13:51-60. [ Links ]
17. Bergstrom J, Bostrom L. Tobacco smoking and periodontal hemorrhagic responsiveness. J Clin Periodontol 2001;28: 680-685. [ Links ]
18. Mavropoulos A., Aars H, Brodin P. Hyperaemic response to cigarette smoking in health gingiva. J Clin Periodontol 2003;30:214-221. [ Links ]
19. Morozumi T, Kubota T, Sato T, Okuda K, Yoshie H. Smoking cessation increases blood flow and gingival crevicular fluid. J Clin Periodontol 2004;31:267-272. [ Links ]
20. Apatzidou DA, Riggio MP, Kinane DF. Impact of smoking on the clinical, microbiological and immunological parameters of adult patients with periodontitis. J Clin Periodontol 2005;32:973-983. [ Links ]
21. Gomes SC, Piccinin FB, Susin C, Oppermann RV, Marcantonio RAC. Effect of supragingival plaque control in smokers and never-smokers: 6 months evaluation of patients with periodontitis. J Periodontol 2007;78:1515-1521. [ Links ]
22. Mavropoulos A, Brodin P, Rosing CK, Aass Am, Aars H. Gingival blood flow in periodontitis patients before and after periodontal surgery assessed in smokers and nonsmokers. J Periodontol 2007;78:1774-1782. [ Links ]
23. Preber H, Bersgtrom J. Effect of non-surgical treatment on gingival bleeding in smokers and non-smokers. Acta Odontol Scand 1986;44:85-89. [ Links ]
24. Page R, Offenbacher S, Schoreder HE. Advances in the pathogenesis of periodontitis. Periodontol 2000 1997;14: 216-248. [ Links ]
25. Spiekerman CF, Hujoel PP, DeRouem TA. Bias Induced by Self-reported Smoking on Periodontitis-Systemic Disease Associations. Dent Res 2003;82:345-349. [ Links ]
26. Giannopoulou C, Cappuyns I, Mombelli A. Effect of smoking on gingival crevicular fluid cytokine profile during experimental gingivitis. J Clin Periodontol 2003;30:996-1002. [ Links ]
27. Persson L, Bergstrom J, Gustafsson A. Effect of tobacco smoking on neutrophil activity following periodontal surgery. J Periodontol 2003;74:1475-1482. [ Links ]
28. Tullger G, Kurtis B, Serdar M, Yucel A, Ayhan E, Karaduman B, Ozcan G. Effects of phase I periodontal treatment on gingival crevicular fluid levels of matrix metalloproteinase- 3 and tissue inhibitor of metalloproteinase. J Clin Periodontol 2005;32:1011-1015. [ Links ]
29. Linden GJ, Mullally BH, Burden DJ, Lanney PJ, Shaw C, Ardill J, Lundy FT. Changes in vasoactive intestinal peptide in gingival crevicular fluid in response to periodontal treatments. J Clin Periodontol 2002;29:484-489. [ Links ]














