Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Acta Odontológica Latinoamericana
On-line version ISSN 1852-4834
Acta odontol. latinoam. vol.24 no.2 Buenos Aires Sept. 2011
ARTÍCULOS ORIGINALES
Optical X-ray density of composite resin luting agents
Helena G. Carracho1, Ivori D. da Silveira2, Clarissa G. Soares2, Maria Paula G. Paranhos2, Luiz Henrique Burnett Junior2, Ana Maria Spohr2
1 Department of Restorative Dentistry, School of Dentistry, Passo Fundo University, Brazil.
2 Department of Restorative Dentistry, School of Dentistry, Pontifical Catholic University of Rio Grande do Sul, Brazil.
CORRESPONDENCE Ana Maria Spohr Pontifical Catholic University of Rio Grande do Sul (PUCRS) School of Dentistry, Block 6 Av. Ipiranga 668 CEP: 90616-900, Brazil E-mail: anaspohr@terra.com.br
ABSTRACT
This study verified the optical density of four composite resin luting agents – RelyX ARC (RY), Enforce (E), C&B Cement (CB) and Flow it (FI), at thicknesses of 2, 3, and 4 mm. The optical density of the luting agents was compared with that of enamel and dentin at the same thicknesses. Fifteen tooth crowns were embedded in PVC cylinders with self-cured acrylic resin. In addition, acrylic resin was poured into 5 PVC cylinders and four equidistant 5 mm diameter holes were prepared, with one luting material inserted in each. A laboratory cutting machine was used to prepare 4-, 3- and 2-mm thick slices of the tooth crowns and materials. Digital images were obtained with a Digora system. Three radiographs of each thickness were obtained, totalizing 135 radiographs of the crowns and 45 of the materials. Three readings were carried out on each radiograph: three in enamel, three in dentin and three in each material, totalizing 1350. According to Student’s t-test (p≤0.05), the materials RY and CB did not differ statistically from enamel at any thickness, but differed from E and FI, which had statistically higher results. RY did not differ statistically from dentin, presenting a lower value than enamel and lower than the other materials at all thicknesses. The composite resin luting agents E and FI can be distinguished from dental structures, while the CB and RY are not easily distinguished.
Key words: Dental digital radiography; Resin cements; Dental enamel; Dentin.
RESUMO
Densidade óptica de cimentos resinosos
Este estudo verificou a densidade optica de quatro cimentos resinosos – RelyX ARC (RY), Enforce (E), C&B Cement (CB) and Flow it (FI) – nas espessuras de 2, 3 e 4 mm, e comparou esses materiais com o esmalte e a dentina nas mesmas espessuras. Quinze coroas de terceiros molars foram incluidas em cilindros de PVC com resina acrilica autopolimerizavel. Alem disso, resina acrilica foi vertida dentro de 5 cilindros de PVC e feitos quatro orificios equidistantes, sendo um material inserido em cada orificio. Fatias das coroas e dos materiais foram obtidos em maquina de corte laboratorial nas espessuras de 4, 3 e 2 mm. O sistema Digora foi usado para obter as imagens digitais. Tres radiografias de cada espessura foram obtidas, totalizando 135 radiografias para as coroas e 45 para os materiais. Tres leituras foram realizadas em cada radiografia, sendo tres em esmalte, tres em dentina e tres em cada material, totalizando 1350 leituras. De acordo com o teste de Student (p≤0,05), os materiais RY e CB nao tiveram diferenca estatistica do esmalte em todas as espessuras, mas se diferenciaram do E e do FI, os quais apresentaram valores de densidade optica estatisticamente superiores. RY nao se diferenciou estatisticamente da dentina, apresentando um valor menor do que o esmalte e dos outros materiais em todas as espessuras. Os cimentos resinosos E e FI podem facilmente ser diferenciados das estruturas dentais, enquanto CB e RY nao seriam facilmente diferenciados.
Palavras-chave: Radiografia dental digital; Cimento resinoso; Esmalte; Dentina.
INTRODUCTION
The use of adhesive materials is invaluable in restorative techniques. Composite resin belongs to this material category and has been used as an esthetic alternative to metal restorations for over three decades. Composite resin-based materials have also been used as luting agents and are generally called resin cements. The use of resin cements has become popular due to the increasing demand for bonded restorations, such as composite/ceramic inlays, onlays, veneers, and crowns. The properties of resin cements are superior to those of traditional cements such as zinc phosphate and glass ionomer cements, and they also improve esthetics1. Moreover, resin cements enable bonding to both tooth structure and indirect restorative material, increasing resistance to fractures2.
In addition to resin cements, low viscosity composite resins (flowable composite resins) have been used as luting agents. The usefulness of direct resins in dentistry was recognized in 1977 through specification No 27 formulated by the Council on Dental Materials and Devices3, and one of the desirable requisites of the material is its radiopacity. This radiopacity would help clinicians to distinguish these restorative materials radiographically from decay, voids, gaps, or other defects that could lead to clinical failure4. Research on the radiopacity of restorative materials has contributed to clinical practice diagnosis in dentistry. With the advance of digital technology, it has been possible to measure the optical density of different materials, which aids the detection of unusual structures5-10. Digital technology reduces the variables of human limitation and offers a great number of tools and benefits. Lower radiation doses, shorter working time, and the possibility of working on-line are some of the advantages of using digital technology11-14. In view of the importance of the radiopacity of materials and the development of digital images, it seems vital to assess whether the resin cements can be observed and distinguished from dental structures. The aim of this study was to evaluate the optical Xray density of three resin cements and one flowable composite resin at different thicknesses (2, 3, and 4 mm) and compare them with enamel and dentin at the same thicknesses. The null hypothesis is that there is no difference in the optical density of the different luting agents in comparison with enamel and dentin.
MATERIALS AND METHODS
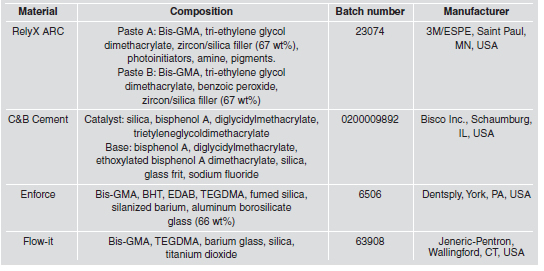
The materials used in this study are listed in Table 1.
Table 1. Information about the materials used and their composition.
Preparation of enamel and dentin samples
Fifteen human molars extracted by therapeutic indication were used in this study. The Ethical Committee of Pontifical Catholic University of Rio Grande do Sul approved this study. The teeth were cleaned using running water, stored in distilled water under refrigeration at 4oC, and used within 6 months after extraction. Before use, the teeth were sterilized for 20 minutes in an autoclave at 121.C and pressure of 1.4 to 1.8 Kgf/cm2.
The roots were removed at the level of the cementenamel junction. The convex buccal and lingual surfaces of the crowns were removed using a diamond disk (KG Sorensen, S.o Paulo, SP, Brazil) under water cooling. The buccal-lingual distance was measured with a digital caliper with a precision of 0.01 mm (Mitutoyo Sul Americana Ltda., Suzano, S.o Paulo, Brazil). Each tooth crown was fixed with wax with the lingual surface against a glass plate. A 3 cm high PVC cylinder, with an external diameter of 2.5 cm and internal diameter of 2 cm, was placed over the glass plate with the tooth crown in the center. Self-cured acrylic resin was poured into the cylinder to completely embed the tooth crown, without covering the lingual face (Fig. 1). Extreme care was taken to avoid contact of the acrylic resin with the lingual surface.
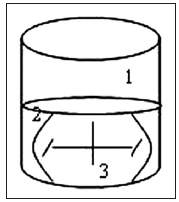
Fig. 1: Tooth crown embedded in selfcured acrylic resin. 1) PVC tube, 2) acrylic resin, 3) tooth crown.
The tooth crown embedded in acrylic resin was fixed to a laboratory cutting machine (Labcut 1010, EXTEC Corp., London, England) by means of the remainder of the PVC tube. The first cut thickness was calculated according to the measurement of the embedded tooth crown, which was previously measured with the caliper. This cut was made in order to obtain a remaining thickness of 4 mm, of which the first radiograph was taken. For instance, if the crown measured 6.45 mm, the first slice would measure 2.45 mm so that a remaining thickness of 4 mm could be obtained. The other two slices were 1 mm thick each, in order to obtain measurements of 3 and 2 mm, respectively. Radiographs were taken at each thickness. Fifteen specimens were obtained for each thickness.
Preparation of composite resin luting agent samples
Marks were made on five 3 cm-high PVC cylinders, with external diameters of 2.5 cm and internal diameters of 2 cm, at the measurement corresponding to 4 mm cylinder height. The cylinder was placed on a glass plate and then self-cured acrylic resin was poured into it up to the mark. When polymerization was complete, a milling cutter was used to make four equidistant 5 mm diameter holes through the entire thickness (4 mm) of the acrylic resin. To enable the materials to escape at the time they were applied inside the holes, niches were made in the acrylic resin with No. 2 diamond burs under low speed. These niches were made in the positions of 3, 6, 9 and 12 hours to identify the material inserted in each hole (Fig. 2).
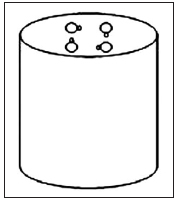
Fig. 2: PVC tube with the four equidistant holes and niches, into which the materials were inserted.
Before inserting the resin materials, tape with the same diameter as the PVC cylinder was placed inside it to prevent the material from leaking into the PVC tube, and to ensure that the thickness would remain at 4 mm. The materials were handled in accordance with the manufacturers’ recommendations. Shade A3 was used for all the luting agents, with the exception of C&B Cement, which is marketed in a universal shade. The resin cements were inserted into the holes with the aid of a Centrix syringe with metal ends, and the flowable composite resin was inserted with a pointer provided by its manufacturer. The materials were placed in two 2 mm increments; the first increment was lightcured for 40 s with a XL3000 (3M/ESPE, Saint Paul, Minnessota, USA) light-curing unit. A clear matrix strip and a glass plate were placed over the second increment, leaving the niche free for the material to escape. With the glass plate in position, the last increment was light-cured for 10 s, and after the plate was removed, for another 30 s, with a total of 40 s of light-curing. The light intensity of the unit was controlled by a radiometer (model 100 – Demetron/Kerr, Danbury, Connecticut, USA), and found to stay between 580 and 630 mW/cm2. For the self-cured resin cement (C&B Cement) the glass plate was removed after waiting 15 minutes. The materials inserted in the acrylic resin were fixed to a laboratory cutting machine and the cuts were obtained, as described for the tooth crowns. Five specimens were obtained of each thickness, and each of them contained the four different materials.
Digital imaging and optical density measurement
Four small-sized optical plates (26 x 35 x 1.6 mm, from the direct digitizing system Digora®) were used (Soredex, Orion Corp., Helsinki, Finland). A preliminary test was carried out to define the exposure time. The exposure time was varied in order to determine which digital image would show the best density and contrast, according to the agreement between two radiologists. Digital image standardization was obtained in accordance with the following description: a) utilization of an x-ray device (Gnatus®) with electrical regime of 120 V and 50/60 Hz; b) exposure time of 0.1 sec; c) 40 cm focal distance; d) x-ray central beam perpendicular to the center of the specimen. Three radiographs of each thickness were obtained, totalizing 135 radiographs for the crowns and 45 for the materials. This was done in order to minimize the probability of error due to possible variation of the electric current during exposure or during the scanning process. The specimen was placed in a centralized position on the optical plate. Image digitizing was carried out in a room with low intensity light by means of the Digora direct image digitizing system. Each optical plate was unpacked and introduced into the laser reader, and each plate presented the image of one thickness. The optical plate with the image of the 4 mm thickness was always the first to be inserted in the scanner, followed by the 3- and 2-mm thicknesses, respectively. Each radiograph was identified within the system by a number.
For the optical density reading, a point at x and y coordinates was selected, always located in the same area of the sample. Three readings were carried out on each radiograph: three in enamel, three in dentin and three in each material, and the mean was considered the value for each of the specimen. As 180 radiographs were taken (135 for the crowns and 45 for the materials) a total 1350 optical readings were obtained. Both image digitalization and optical readings were always carried out by the same operator.
Statistical Analysis
The data were analyzed by two-way ANOVA and Tukey multiple comparisons test. Materials and thicknesses were the two factors. For comparison between the dental structures (enamel and dentin) and each material, one by one, and at each thickness, Student’s t-test was applied. All statistical analyzes were performed at a significance level of 0.05.
RESULTS
Results of the ANOVA are summarized in Table 2. The material and thickness factors were significant.
Table 2. Two-way ANOVA for the results.

The interaction between the factors was not significant. In accordance with Tukey multiple comparisons test, Enforce (182.02) and Flow It (172.67) had the highest mean optical density, differing statistically from enamel (122.43), dentin (98.95), and the other materials (p<0.05). C&B Cement showed the third highest mean optical density, differing statistically from enamel, dentin, and RelyX ARC (p<0.05). RelyX ARC (97.79) did not differ statistically from dentin, presenting a lower mean when compared to enamel and the other materials (p<0.05) (Table 3).
Table 3. Mean Optical density of the luting agents, enamel, and dentin at all thicknesses.
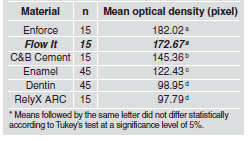
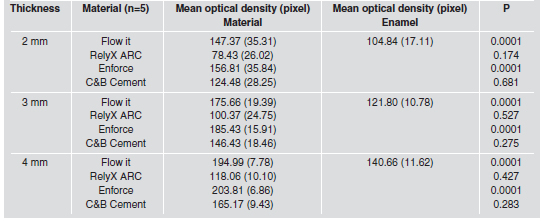
According to Student’s t-test, Flow It and Enforce had greater and statistically different optical densities than enamel at all thicknesses. RelyX ARC and C&B Cement did not differ statistically from enamel at all thicknesses. The increase in thickness was proportional to the increase in optical density values for both luting agents and enamel (Table 4).
Table 4. Mean optical density of enamel compared to the luting agents at each thickness.
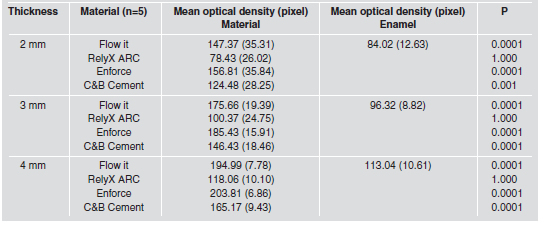
RelyX ARC did not present significant difference when compared with dentin at all thicknesses, whereas all other materials presented greater optical density than dentin. The increase in thickness was proportional to the increase in optical density values for both luting agents and dentin (Table 5).
Table 5. Mean optical density of dentin compared to the luting agents at each thickness.
DISCUSSION
The selection of the resin cements (C&B Cement, Enforce, and RelyX ARC) and the flowable composite resin (Flow It) in this study was based on their wide use in dentistry. Flowable composite resins can be beneficial when applied to areas with difficult access, such as the gingival floor of proximal boxes in class II restorations. These low viscosity materials also feature the possibility of being used as luting agents14,15.
One of the major advantages that a luting agent can offer is a radiographic image that differs from the radiographic image of dental structures. This is why the radiopacity of these materials must be higher than that of dentin, and must also be similar to or even higher than that of enamel6,16-18. Adequate radiopacity leads to an optimum radiographic contrast. This is clinically relevant because of the possibility of distinguishing the dental materials radiographically from tooth structure and decay, voids, gaps, or other defects. In addition, the radiopacity allows the identification of dental materials in cases of aspiration, deglutition or penetration into the tissues as a result of accident or trauma19. According to the results, the null hypothesis of this study was rejected because the optical densities of the luting agents differed from those of enamel and dentin. The optical density of Enforce and Flow It was higher than that of enamel and dentin, which suggests that they can be easily differentiated in a radiograph. Rubo and El-Mowafy6 also found higher values for Enforce when compared with enamel. Murchison et al.15 and Bouschlicher et al.18 compared the radiopacity of flowable composite resins with enamel and dentin, and also reported higher values for the composite resin Flow It than for enamel. The optical density of C&B Cement was higher than that of enamel and dentin, which would make it easier to differentiate this material from these tissues (Table 3). However, when the thicknesses were separately evaluated, the optical density of C&B Cement did not differ statistically from that of enamel. Regardless of whether the statistical test did or did not find any difference between the optical density values, it is important to verify the clinical significance of these numerical values. According to a subjective visual evaluation of the optical density on the computer screen while the values of optical density were being obtained, it was observed that numerical differences above 30 pixels would allow visual differentiation between the materials. As the numerical difference of the optical density of C&B Cement and enamel was lower than 30 pixels, it can be assumed that although there is a statistical difference, this material would not be easily distinguished from enamel.
Enforce and Flow It would be differentiated because they presented numerical differences in optical density far above 30 pixels in comparison with enamel. RelyX ARC had the lowest optical density mean at all thicknesses, being similar to dentin and statistically lower than enamel, suggesting that it would be more difficult to visualize and distinguish from the dental tissues than the other materials. However, there was no statistical difference when the thicknesses were separately evaluated and compared with enamel. In the same way as with C&B Cement, regardless of whether the test found statistical difference or not, the differences in the optical density value were lower than 30 pixels. The results of the present study corroborate those of Attar et al.20, in which RelyX ARC was also the material with the lowest optical density. Different chemical elements with high atomic numbers, such as barium, strontium, zirconium, zinc, yttrium, ytterbium and lanthanum are responsible for the radiopacity21-23. In addition to the atomic composition, the density of each atom in the material and its physical structure may also influence the optical density24. The different chemical elements used in each material, as well as the percentage of these elements in the composition, are factors that may interfere with the optical density of those materials. This might justify the different optical density values among the materials evaluated. Toyooka et al.22 and Sabbagh et al.25 found a linear correlation between the percentage of fillers and the radiopacity of the tested materials. Elements with a low atomic number, such as silicium, result in radiolucent materials, while materials with high atomic numbers (Barium, Ytrium, Ytterbium, Zirconium, Strontium) are more radiopaque14,26. Toyooka et al.22 emphasized that the chemical element zirconium confers greater radiopacity on materials than barium does. The manufacturers, however, do not inform the exact percentage of each element in the composition of the dental materials. RelyX ARC contains 67 wt% of silica and zirconium fillers, but the manufacturer does not specify the exact percentage of zirconium. Most likely there is not a sufficient percentage of zirconium to allow an optical density greater than the enamel and dentin, since this resin cement presented the lowest optical density mean value. The manufacturers of C&B Cement did not report any radiopaque particle in its composition. It can be assumed that some radiopaque particles may be present since it showed satisfactory optical density. Enforce and Flow It contain barium in their compositions, possibly in a high percentage, since their optical density was higher than that of enamel. When evaluating each material at the three thicknesses, the optical density means were higher as the thickness increased for all materials tested. This finding was predictable, since the greater the thickness, the greater the quantity of radiopacifying elements.
In the present study, the luting agents samples were evaluated separately from the tooth samples, as in previous studies6,8. A larger number of samples (n=15) was used for the dental structures than for the materials (n=5) due to the variability of the dental structure, especially dentin5. In spite of this variability, the optical density means obtained for enamel and dentin in this study corroborate the values found by Bouschlicher et al.18 and Fonseca et al.27, who also compared base and luting materials with enamel and dentin at 2-mm thickness.
The clinical significance of the present study was the identification of which materials did not present adequate radiopacity. The lack of radiopacity suggests that these materials would not be appropriate for clinical use since their differentiation from the dental structures would not be possible. According to the methodology used and within the limitations of this study, the results suggest that Enforce and Flow It can be easily distinguished from dental structures, while C&B Cement and Rely X would not be easily distinguished.
1. Li ZC, White SN. Mechanical properties of dental luting cements. J Prosthet Dent 1999;81:597-609. [ Links ]
2. Burke FJT. The effect of variations in bonding procedure on fracture resistance of dentin-bonded all-ceramic crowns. Quintessence Int 1995;26:293-300. [ Links ]
3. Council on Dental Materials and Devices. New American Dental Association Specification No. 27 for Direct Filling Resins. Reports of Councils and Bureaus. J Am Dent Assoc 1977;94:1191-1194. [ Links ]
4. Council on Dental Materials, Instruments and Equipment. The desirability of using radiopaque plastics in dentistry: a status report. J Am Den Assoc 1981;102:347-349. [ Links ]
5. Akerboom HB, Kreulen CM, van Amerongen WE, Mol A. Radiopacity of posterior composite resins, composite resin luting cements, and glass ionomer lining cements. J Prosthet Dent 1993;70:351-355. [ Links ]
6. El-Mowafy M, Benmergui C. Radiopacity of resin-based inlay luting cements. Oper Dent 1994;19:1-13. [ Links ]
7. Khademi JA. Digital images & sound. J Dent Educ 1996; 60:41-46. [ Links ]
8. Rubo MHM, El-Mowafy O. Radiopacity of dual-cured and chemical cured resin based cements. Int J Prosthodont 1998;11:70-74. [ Links ]
9. Rosenstiel SF, Land MF, Crispin BJ. Dental luting agents: A review of the current literature. J Prosthet Dent 1998;80: 280-301. [ Links ]
10. Fraga RC, Luca-Fraga LRL, Pimenta LAF. Physical properties of resinous cements: an in vitro study. J Oral Rehabil 2000;27:1064-1067. [ Links ]
11. Grondahl HG. Digital radiology in dental diagnosis: a critical view. Dentomaxillofac Radiol 1992;21:198-202. [ Links ]
12. Farman AG, Scarfe WF. Pixel perception and voxel vision: constructs for a new paradigm in maxillofacial imaging. Dentomaxillofac Radiol 1994;23:5-9. [ Links ]
13. Versteeg CH, Sanderink GCH van der Stelt PF. Efficacy of digital intra-oral radiography in clinical dentistry. J Dent 1997;25:3-4. [ Links ]
14. Turgut MD, Attar N, .nen A. Radiopacity of direct esthetic restorative materials. Oper Dent 2003;28:508-514.
15. Murchison DF, Charlton DG, Moore WS. Comparative radiopacity of flowable resin composites. Quintessence Int 1999;30:179-184. [ Links ]
16. Lutz F, Phillips RW, Roulet JF, Setcos JC. In vivo and in vitro wear of potential posterior composites. J Dent Res 1984;63:914-920. [ Links ]
17. Nair MK, Tyndall DA, Ludlow JB, May K, Ye F. The effects of restorative material and location on the detection of simulated recurrent caries. A comparison of dental film, direct digital radiography and tuned aperture computed tomography. Dentomaxillofac Radiol 1998;27:80-84. [ Links ]
18. Bouschlicher MR, Cobb DS, Boyer DB. Radiopacity of compomers, flowable and conventional resin composites for posterior restorations. Oper Dent 1999;24:20-25. [ Links ]
19. Klein KA, Hobbs BB. Radiopacity of glass: Does the lead content matter? CMAJ 1995;153:1224. [ Links ]
20. Attar N, Tam LE, McComb D. Mechanical and physical properties of contemporary dental luting agents. J Prosthet Dent 2003;89:127-134. [ Links ]
21. Bowen RL, Cleek GW. A new series of x-ray-opaque reinforcing fillers for composite materials. J Dent Res 1972;51:177-182. [ Links ]
22. Toyooka H, Taira M, Wakasa K, Yamaki M, Fujita M, Wada T. Radiopacity of 12 visible-light-cured dental composite resins. J Oral Rehabil 1993;20:615-622. [ Links ]
23. Aoyagi Y, Takahashi H, Iwasaki N, Honda E, Kurabayashi T. Radiopacity of experimental composite resin containing radiopaque materials. Dent Mater J 2005;24:315-320. [ Links ]
24. Fonseca RB, Haiter-Neto F, Fernandes-Neto AJ, Barbosa GA, Soares CJ. Radiodensity of enamel and dentin of human, bovine and swine teeth. Arch Oral Biol 2004;49:919-922. [ Links ]
25. Sabbagh J, Vreven J, Leloup G. Radiopacity of resin-based materials measured in film radiographs and storage phosphor plate (Digora). Oper Dent 2004;29:677-684. [ Links ]
26. Taira M, Toyooka H, Miyawaki H, Yamaki M. Studies on radiopaque composites containing ZrO2- SiO2 fillers prepared by the sol-gel process. Dent Mater 1993;9:167-171. [ Links ]
27. Fonseca RB, Branco CA, Soares PV, Correr-Sobrinho L, Haiter-Neto F, Fernandes-Neto AJ et al. Radiodensity of base, liner and luting dental materials. Clin Oral Investig 2006;10:114-118. [ Links ]














