Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Acta Odontológica Latinoamericana
On-line version ISSN 1852-4834
Acta odontol. latinoam. vol.24 no.2 Buenos Aires Sept. 2011
ARTÍCULOS ORIGINALES
Self-bone graft and simultaneous application of implants in the upper jawbone. (Fit lock technique)
Pedro Vittorini-Velasquez1, Giovanni Falisi2, Massimo Galli2, Juan Carlos Gallegos-Rivera3
1 Maxillo-facial Clinic Cochabamba, Bolivia.
2 Department of Dentistry, Sapienza University of Rome.
3 Department of Dentistry, Municipal Japanese University Hospital, Santa Cruz de la Sierra, Bolivia.
CORRESPONDENCE Dr. Giovanni Falisi Via del Vivaio 19 00172 Rome - Italy g.falisi@tiscali.it
ABSTRACT
The implant-supported rehabilitation of posterosuperior sectors may be sometimes conditioned by the pneumatization of the para-nasal sinuses, which decreases the possibility of implant placement when the bone height is ≤ 4 mm. (prerequisite for primary stabilization). Sinus lift surgery with simultaneous application of implants is the procedure which provides the best chance of success compared to the application of the filling material only. There are many surgical techniques which combine autogenous bone grafting (ilium crest, calvaria, fibula) with implant placement. The objective of this report is to present a new technique which aims to minimize invasive bone grafting and patient morbidity. The authors performed a longitudinal study on 21 cases with a 94.5% success rate, exemplified by one clinical case. The advantages of this technique are:
1) Functional and anatomical recovery of the jaw cavity.
2) Simultaneous application of implants when the bone is ≤ 4mm.
3) Reduction of surgical times.
4) Reduced patient morbidity.
5) Local anesthesia.
Key words: Bone grafting; Dental implants.
RESUMEN
Auto injerto de hueso y aplicación simultánea de los implantes en el maxilar superior. (Técnica de bloqueo de implante)
La rehabilitacion implanto soportada de los sectores posterosuperiores resulta, a veces, condicionada por la neumatizacion del seno maxilar, reduciendo la posibilidad de la aplicacion de los implantes cuando la disponibilidad osea es inferior a los 4 mm. (Condicion Limite para la estabilidad primaria). El levantamiento del seno maxilar y la aplicacion simultanea de los implantes es con seguridad la condicion que mejor garantiza el exito, respecto a la sola aplicacion del material de relleno. Muchas son las tecnicas quirurgicas desarrolladas en la utililizacion del hueso autologo (cresta iliaca, calota craneana, perone) y la aplicacion de los implantes. En este articulo se presenta una nueva tecnica para reducir al minimo la invasividad de la toma del material oseo de injerto autologo y la morbilidad del paciente. Se ha realizado un estudio longitudinal sobre 21 casos consecutivos, mostrando un exito del 94,5%.
Las ventajas de esta tecnica son:
1) Recuperacion funcional y anatomica del seno maxilar.
2) Aplicacion inmediata de los implantes con un espesor residuo de hueso de piso de seno menor a los 4 mm.
3) Reduccion de los tiempos quirurgicos.
4) Menor Morbilidad del paciente.
5) Anestesia loco regional.
Palabras clave: Injerto de hueso; Implantes dentales.
INTRODUCTION
Tooth loss often causes the pneumatization of the para-nasal sinuses, leaving not enough bone tissue to set dental implants. The approach to this anatomical zone has always been controversial, regarding both surgical approach and post-surgical complications1-8. Many techniques have been used in order to avoid this zone: the use of pterygoid and trans-zygomatic implants, for example9-12.
Even in this case, however, the maxillary sinus is intruded to seek bicorticalism and to obtain primary implant stabilization5,13. International literature suggests maxillary sinus filling with simultaneous implant placement with a bone height of ≥4 mm6,14-18. When the bone portion is ≤4 mm, as in Misch’s classification, it is suggested that a reconstructive- regenerating phase should be performed first, followed by a second surgical phase for implant placement17-22. Some authors propose the use of extrasinus osteosynthesis plates in order to obtain primary implant stabilization23- 25. Other authors2,10-12, 26-30 report that primary stabilization can be achieved through extraoral autogenous bone grafting (fibula or hip) and simultaneous implant placement20,25,31.
However, this technique involves some disadvantages:
• It requires total anesthesia, therefore surgery must be performed in a private clinic or hospital.
• The extraction of the autograft from the donor site must be performed by an orthopedist.
• Patient mobility and morbidity.
• The high biological and economic costs.
Considering the abovementioned disadvantages, the authors of this article propose an alternative surgical technique which allows simultaneous implant placement when the bone height is ≤4 mm, by means of intraoral autogenous bone grafting and local anesthesia.
MATERIALS AND METHODS
About 400 patients were evaluated for implant-supported rehabilitation of posterosuperior sectors at the Clinica Dentomaxillofacciale Vittorini Cochabamba and at the Municipal Japanese Hospital, Bolivia, in 2002 and 2003. During this period all patients were evaluated according to our clinical implant protocol for successful prosthetic restoration. We selected a group of 21 patients by means of the following standard exclusion and inclusion criteria:
Standard exclusion criteria:
• Insufficient dental care.
• Acute and chronic sinusitis.
• Patients with high risk factors.
• Patients who were undergoing Cadwell Luc treatments.
• Patients who were undergoing radiation therapy.
• Patients with a bone height of ≥4 mm.
Standard inclusion criteria:
• Bone height ≤ 4 mm (assessed by means of x-ray).
• Available harvesting bone at the ramus-symphysis donor site.
• Patient’s consent to participate in the clinical study.
• Patient’s consent to undergo clinical follow-up.
A total 330 patients were excluded from the study. Among the 70 patients considered for inclusion: 30 did not give consent to treatment; 19 did not undergo clinical follow-up. The study group was finally composed of 21 patients. Of these, 13 were male, with an average age of 58.2 years, and 8 were female, with an average age of 59.8 years. All patients underwent the placement of cone implants with Tps in combination with SLA surface treatment ( microporous surface and plasma-spray). The total number of implants was 37, placed as follows:
6 in position 1.6;
3 in position 1.7;
12 in position 2.6;
11 in position 2.7.
The length of inserted implants was 11.5 mm for 16 implants and 13 mm for 21 implants, with a diameter of 3.75 mm (Table 1). All implants were loaded progressively 6 months after the insertion.
Table 1. Specimen description.

Surgical Technique
- Surgical asepsis: disinfection of intraoral field with a 0.2% chlorhexidine gluconate mouthwash for 2 minutes and sterilization of extraoral field with povidone (polyvinylpyrrolidone PVP ).
- Isolation of surgical field with sterile towels.
- Locoregional anesthesia with mepivacaine hydro chloride 1:100.000.
- Nerve block and plexus block anesthesia in the maxillary region (retromolar triangle, vestibular and palatal portion and nasopalatine nerve) and nerve block and plexus block anesthesia in the mandibular region.
Recipient site preparation
1. A primary crestal incision and secondary full-thickness releasing incisions (trapezoidal flap) were made following the incision design (Fig. 1 a-b).
2. The flap was detached by means of a Freeman periosteal elevator (Fig. 1 b).
3. The vestibular cortical malar bone surface was exposed up to the retromolar tuberosity.
4. The osteotomy of the vestibular wall of the maxillary sinus was performed by means of an oscillating saw or Piezosurgery Device. (Fig. 1 c-d).
5. The Schneider membrane was detached starting from the back portion to pass with delicate movements to the front and then inferior portions to achieve the complete detachment and exposure of the bone portion of the medial wall of the maxillary sinus (Fig. 1 e-f).
6. The wound was rinsed with an anti - biotic solution (gentamicin 80 mg).
7. The alveolar socket for implants was prepared.
8. In order to maintain the new membrane position, a TNT gauze, soaked in the same antibiotic solution used for rinsing, was inserted.

Fig. 1: a ) Flap design, primary crestal incision and two full-thickness releasing incisions (trapezoidal flap). b) Flap is detached and the vestibular cortical malar bone surface is exposed up to the retromolar tuberosity. c) Osteotomy of the vestibular wall of the maxillary sinus is performed by means of an oscillating saw or Piezosurgery Device. d) Prospective view of the flap depth which must not lacerate the Schneider membrane. e) The Schneider membrane is detached from the sinus wall with delicate movements. f) The membrane is detached from the medial wall of the maxillary sinus. g) Donor site preparation. h) After mucosal detachment, the alveolar socket for implant is prepared performing all the drill passages to 3.75 mm. diameter. i) A trephine-type dental drill with a diameter of 8 mm. is used to perform the osteotomy and to harvest the bone graft. j) Bone graft is examined. k) The implant friction level is tested under physiological solution jet. l) The alveolar socket for implant is prepared and the bone graft is inserted into the recipient site. m)The implant is placed and screwed. n) Empty residual spaces are filled with autologous bone or alloplastic fillers.
Donor site preparation
The donor site was chosen (Fig. 1 g).
1. A primary paramarginal incision was made along the anterior border of the mandibular ramus, starting from the retromolar triangle up to the distal position 4.6 (Fig. 1 h).
2. An all-thickness detachment was performed.
3. The surgical socket was prepared as if the implant was to be inserted, performing all the drill passages to prepare the alveolar socket for implant and the implant threading, as in the line to line technique (Fig. 1 h).
4. A Trephine with a diameter of 8 mm was used to perform the osteotomy and to harvest the bone graft (Fig. 1 i-j).
5. The implant with graft was tested under physiological solution jet to evaluate the friction level and adaptability (Fig. 1 k).
6. The implant and the bone graft were inserted into the recipient site (Fig. 1 l-m).
7. The empty spaces were filled with autologous bone or/and filling materials (Fig. 1 n).
8. The bony window was repositioned (Fig. 1 n).
9. The wound was sutured in layers with separate knots.
RESULTS
All clinical and radiographic indications (x-ray) were followed during the follow-up period and stability and osseointegration were assessed by means of Percussion test and Reverse torque at 25 Newton. The first clinical and radiographic control after three months from implant fixing revealed no clinical and radiographic modification of the 37 implants inserted or of the surrounding tissues. Six months later, when implants were functionalized, 2 implants (5.5%) were lost, one because the patient had continued to wear a mobile prosthesis which pressed the treated site, the other because the implant was not osseointegrated, while the remaining 35 implants (94.5%) showed good stability. After definitive rehabilitation, the 35 implants, assessed after 1-2-3-5 years, showed no radiological or clinical alterations except for the typical changes due to functionalization (marginal crestal bone reabsorption) and with negative perimplant probing.
Clinical case (Fig. 2)
A 53-year-old patient who needed a prosthetic rehabilitation in position 2.6 with a bone thickness lower than 4 mm.
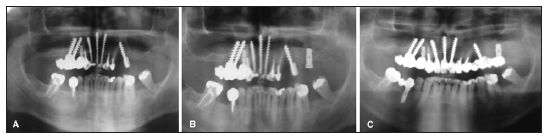
Fig. 2: a) Presurgical orthopanoramic X-ray. b) Post-surgical orthopanoramic X-ray. c) X-ray 5 years after surgery.
DISCUSSION
The autologous intraoral bone graft, used to reconstruct maxillary sinus and to fix simultaneous implants, allows surgical times to be reduced and primary stability to be achieved, which is necessary for osseointegration and implant-supported prosthetic rehabilitation.
Disadvantages
1. The impossibility to use an implant diameter exceeding 3.75 mm because it would cause a fracture of the graft during the screwing phase.
2. The bone block can not exceed 8 mm in diameter because of the anatomical structure of oral cavity.
3. Impossibility to perform this technique when an onlay graft procedure is needed.
Benefits
1. Functional and anatomical recovery of the jawbone cavity.
2. Simultaneous application of implants with a residual bone thickness lower than 4 mm.
3. Reduction of surgical times.
4. Reduced patient morbidity.
5. Local anesthesia. This method is surely a therapeutic alternative, considering that the clinical results are comparable to other techniques described in medical literature2,6,13,19,30,31, but it requires a histomorphometric study and a larger sample group.
1. Busenlechner D, Huber CD, Vasak C, Dobsak A, Gruber R, Watzek G. Sinus augmentation analysis revised: the gradient of graft consolidation. Clin Oral Implants Res 2009; 20:1078-1083. [ Links ]
2. Handschel J, Simonowska M, Naujoks C, Depprich RA, Ommerborn MA, Meyer U, Kübler NR. A histomorphometric meta-analysis of sinus elevation with various grafting materials. Head Face Med 2009;11:5-12. [ Links ]
3. Smiler DG, Johnson PW, Lozada JL, Misch C, Rosenlicht JL, Tatum OH Jr, Wagner JR. Sinus lift grafts and endosseous implants. Treatment of the atrophic posterior maxilla. Dent Clin North Am. 1992;36:151-186. [ Links ]
4. Wallace SS. Maxillary sinus augmentation: evidence-based decision making with a biological surgical approach. Compend Contin Educ Dent. 2006;27:662-668. [ Links ]
5. Chiapasco M, Zaniboni M, Rimondini L. Dental implants placed in grafted maxillary sinuses: a retrospective analysis of clinical outcome according to the initial clinical situation and a proposal of defect classification. Clin Oral Implants Res. 2008;19:416-428. [ Links ]
6. Pjetursson BE, Tan WC, Zwahlen M, Lang NP. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J Clin Periodontol. 2008;35:216-240. [ Links ]
7. Timmenga NM, Raghoebar GM, Boering G, van Weissenbruch R. Maxillary sinus function after sinus lifts for the insertion of dental implants. J Oral Maxillofac Surg. 1997;55:936-939. [ Links ]
8. Scolozzi P, Martinez A, Lombardi T, Jaques B. Lateral antrotomy as a surgical approach for maxillary sinus: a modified technique with free bone flap repositioning and fixation with a titanium plate. J Oral Maxillofac Surg. 2009;67:689-692. [ Links ]
9. Aparicio C, Ouazzani W, Garcia R, Arevalo X, Muela R, Fortes V. A prospective clinical study on titanium implants in the zygomatic arch for prosthetic rehabilitation of the atrophic edentulous maxilla with a follow-up of 6 months to 5 years. Clin Implant Dent Relat Res. 2006;8:114-122. [ Links ]
10. Esposito M, Worthington HV, Coulthard P. Interventions for replacing missing teeth: dental implants in zygomatic bone for the rehabilitation of the severely deficient edentulous maxilla. Cochrane Database Syst Rev 2005;19:CD004151. [ Links ]
11. Mozzati M, Monfrin SB, Pedretti G, Schierano G, Bassi F. Immediate loading of maxillary fixed prostheses retained by zygomatic and conventional implants: 24-month preliminary data for a series of clinical case reports. Int J Oral Maxillofac Implants. 2008;23:308-314. [ Links ]
12. Malevez C, Daelemans P, Adriaenssens P, Durdu F. Use of zygomatic implants to deal with resorbed posterior maxillae. Periodontol 2000. 2003;33:82-89. [ Links ]
13. Chiapasco M, Casentini P, Zaniboni M. Bone augmentation procedures in implant dentistry. Int J Oral Maxillofac Implants 2009;24:237-259. [ Links ]
14. Esposito M, Grusovin MG, Worthington HV, Coulthard P. Interventions for replacing missing teeth: bone augmentation techniques for dental implant treatment. Cochrane Database Syst Rev 2006;25:CD003607. [ Links ]
15. Fenner M, Vairaktaris E, Fischer K, Schlegel KA, Neukam FW, Nkenke E. Influence of residual alveolar bone height on osseointegration of implants in the maxilla: a pilot study. Clin Oral Implants Res 2009;20:555-559. [ Links ]
16. Misch CE. Implants and the general practitioner. Dent Today 2007;26:48-52. [ Links ]
17. Misch CE. Progressive bone loading. Dent Today 1995;14:80-83. [ Links ]
18. Misch CE, Dietsh F. How to select, use bone substitute materials in conjunction with root-form implants. Dent Implantol Update 1993;4:93-97. [ Links ]
19. Graziani F, Donos N, Needleman I, Gabriele M, Tonetti M. Comparison of implant survival following sinus floor augmentation procedures with implants placed in pristine posterior maxillary bone: a systematic review. Clin Oral Implants Res 2004;15:677-682. [ Links ]
20. Peleg M, Garg AK, Misch CM, Mazor Z. Maxillary sinus and ridge augmentations using a surface-derived autogenous bone graft. J Oral Maxillofac Surg 2004;62:1535-1544. [ Links ]
21. Kübler NR, Will C, Depprich R, Betz T, Reinhart E, Bill JS, Reuther JF. Comparative studies of sinus floor elevation with autologous or allogeneic bone tissue. Mund Kiefer Gesichtschir 1999;3:S53-60. [ Links ]
22. Tischler M, Misch CE. Extraction site bone grafting in general dentistry. Review of applications and principles. Dent Today 2004;23:108-113. [ Links ]
23. Lang M. Der Sinus-Implantat-Stabilisator in Extremfallen. Implantologie J 1999;3:27-30. [ Links ]
24. Lindorf HH, Müller-Herzog R. Der autologe Sinus-Implantat- Stabilisator(ASIS). ZMK 2004;4:180-189. [ Links ]
25. Nedir R, Nurdin N, Szmukler-Moncler S, Bischof M. Osteotome sinus floor elevation technique without grafting material and immediate implant placement in atrophic posterior maxilla: report of 2 cases. J Oral Maxillofac Surg 2009; 67:1098-1103. [ Links ]
26. Chiapasco M, Biglioli F, Autelitano L, Romeo E, Brusati R. Clinical outcome of dental implants placed in fibula-free flaps used for the reconstruction of maxillo-mandibular defects following ablation for tumors or osteoradionecrosis. Clin Oral Implants Res 2006;17:220-228. [ Links ]
27. Gbara A, Darwich K, Li L, Schmelzle R, Blake F. Longterm results of jaw reconstruction with microsurgical fibula grafts and dental implants. J Oral Maxillofac Surg 2007;65: 1005-1009. [ Links ]
28. Fenner M, Vairaktaris E, Stockmann P, Schlegel KA, Neukam FW, Nkenke E. Influence of residual alveolar bone height on implant stability in the maxilla: an experimental animal study. Clin Oral Implants Res 2009 DOI: 10.1111/j. 1600-0501.2008.01570. [ Links ]
29. Kahnberg KE, Henry PJ, Hirsch JM, Ohrnell LO, Andreasson L, Br.nemark PI, Chiapasco M, Gynther G, Finne K, Higuchi KW, Isaksson S, Malevez C, Neukam FW, Sevetz E Jr, Urgell JP, Widmark G, Bolind P. Clinical evaluation of the zygoma implant: 3-year follow-up at 16 clinics. J Oral Maxillofac Surg 2007; 65:2033-2038. [ Links ]
30. Kamal D, Abida S, Jammet P, Goudot P, Yachouh J. Outcome of oral implants after autogenous bone reconstruction. Rev Stomatol Chir Maxillofac 2009;110:86-88. [ Links ]
31. Misch CE. The use of ramus grafts for ridge augmentation. Dent Implantol Update 1998;9:41-44. [ Links ]














