Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Acta Odontológica Latinoamericana
versão On-line ISSN 1852-4834
Acta odontol. latinoam. vol.25 no.1 Buenos Aires abr. 2012
ARTÍCULOS ORIGINALES
Periodontal conditions in a group of Colombian type 2 diabetic patients with different degrees of metabolic control
Carlos Serrano1, Clara Perez2, Mauricio Rodríguez1
1Department of Oral Medicine and Basic Science, School of Dentistry, National University of Colombia
2Division of Lipids and Diabetes, School of Medicine, National University of Colombia
CORRESPONDENCE Dr.Carlos Serrano Universidad Nacional de Colombia Facultad de Odontología, Ciudad Universitaria Carrera 30 No. 45-03, Building 210, Office 301 Bogotá, Colombia caserranom@unal.edu.co
ABSTRACT
The aim of this study was to measure the occurrence of severe chronic periodontitis in a group of Colombian type 2 diabetes patients. A group of type 2 diabetic patients regularly attending a diabetes program was selected according to specific criteria. Demographic, medical and periodontal variables were recorded. A randomized half-mouth examination was performed, including plaque index, bleeding on probing, pocket depth and clinical attachment level. They were compared to a group of individuals without diabetes, based on different criteria; the first was the presence of ¡Ý 2 interproximal sites with CAL ¡Ý 6 mm, and ¡Ý 1 interproximal sites with PD ¡Ý 5 mm; the second was presence of ¡Ý 50% percentage of bleeding on probing, and ¡Ý 20% sites showing PD ¡Ý 4 mm. The effect of metabolic control was analyzed. Results were tested through Chi-square, Mann-Whitney, Kruskal-Wallis and Pearson correlation tests. Seventy-two subjects with type 2 diabetes were compared to 39 subjects without diabetes of a similar age. Diabetic subjects had a fair degree of metabolic control, HbA1c 7.94% (1.60). Occurrence of severe chronic periodontitis was similar for both groups when using diagnostic criteria based on CAL levels, 22.22%, but was greater for subjects with diabetes when using criteria based on periodontal inflammation, 23.07% versus 5.12%. Degree of metabolic control had a relation to periodontal parameters. Colombian type 2 diabetes subjects demonstrated poorer periodontal conditions than non-diabetic individuals.
Key Words: Chronic periodontitis; Periodontal diseases; Diabetes mellitus; Hemoglobin A, Glycosylated; Diabetes complications.
RESUMEN
Condiciones periodontales de un grupo de pacientes diabéticos tipo 2 con diferente grado de control metabólico en Colombia
El objetivo fue medir la ocurrencia de Periodontitis Crónica Avanzada en un grupo de pacientes diabéticos tipo 2 en Bogotá, Colombia. Un grupo de pacientes diabéticos tipo 2 adherido a un programa de atención fue seleccionado de acuerdo a criterios específicos. Se registraron datos demográficos, médicos y periodontales; los pacientes recibieron un examen periodontal en media boca, de forma aleatoria, que incluía: Número de dientes, hemorragia al sondaje, profundidad de bolsa y nivel de inserción clínico. Los parámetros periodontales fueron comparados con los de un grupo de pacientes sin diabetes. La ocurrencia de Periodontitis Crónica Avanzada fue comparada entre los grupos de acuerdo a dos criterios; el primero fue la presencia de ¡Ý 2 superficies proximales con una pérdida de inserción clínica ¡Ý 6 mm., y ¡Ý 1 superficie proximal con profundidad de bolsa ¡Ý 5 mm.; el segundo criterio fue la presencia de un porcentaje de hemorragia al sondaje ¡Ý50%, y un porcentaje de superficies con profundidad de bolsa ¡Ý 4 mm de ¡Ý20%. El efecto del grado de control metabólico fue analizado. Los resultados fueron sometidos a las pruebas de Chi-cuadrado, Mann-Whitney, Kruskal-Wallis y de correlación de Pearson. Un grupo de 72 pacientes diabéticos tipo 2 fue comparado con 39 pacientes no diabéticos de edad similar. Los pacientes diabéticos presentaron un grado aceptable de control metabólico, HbA1c 7.94% (1.60). La ocurrencia de Periodontitis Crónica Avanzada fue similar en los dos grupos cuando se utilizaron criterios basados en el nivel de inserción clínico, 22.22%; pero fue mayor en los pacientes con diabetes tipo 2 cuando se utilizaron criterios basados en parámetros de inflamación gingival, 23.07% contra 5.12%. El grado de control metabólico demostró una relación con la severidad de los parámetros periodontales. Este grupo de pacientes diabéticos tipo 2 demostró peores condiciones periodontales que las del grupo control analizado.
Palabras Clave: Periodontitis Crónica; Enfermedades Periodontales; Diabetes Mellitus, tipo 2; Hemoglobina A, Glicosilada; Complicaciones de la Diabetes.
INTRODUCTION
Diabetes mellitus is a common endocrine pathology affecting approximately 6-8.5% of the world population1,2. It has been calculated that its prevalence will increase, due to demographic changes, from 171 million people affected worldwide in 2000 to 366 million by the year 2030; in Latin America, this changing prevalence would nearly triple the number of diabetics, from 13 to 32 million people3. An estimated 97% of diabetic individuals suffer from type 2 diabetes4, a multifactorial pathology caused by alterations in several gene products leading to pancreatic â-cell dysfunction and insulin resistance5. Macrovascular and microvascular complications of diabetes represent the main medical burden of the disease; it has been reported that cardiovascular morbidity of type 2 diabetic patients is two to four times greater than that of non-diabetic people6.
Several epidemiological studies have described an increased severity of periodontal disease among diabetic subjects. Data from 4343 individuals included in the NHANES III survey in the USA showed that poorly controlled diabetic subjects were 2.90 times more likely to have severe periodontitis than nondiabetic subjects, after controlling for relevant confounding factors; at the same time, a tendency for higher prevalence of severe periodontitis, odds ratio 1.56, was present in better controlled diabetics7. Studies on the Pima Indian community in Arizona, the population with the highest recorded prevalence of type 2 diabetes mellitus in the world, have described a 2.3 to 4.8 higher prevalence of periodontal disease in different age groups for subjects with diabetes8, 9. Several references originating in different countries have described poorer periodontal conditions in diabetic subjects. Greater significant level of gingival inflammation and attachment loss were found in type 2 diabetic subjects, compared to nondiabetic controls, in a large epidemiological study of 2144 individuals in France10. In Germany, an analysis of type 1 and 2 diabetic subjects comparing the Pomerania Health Study (Germany) to diabetic clinic patients revealed greater attachment level loss in diabetics, this relationship being significantly affected by the level of metabolic control11. In Latin America, few references have described the periodontal conditions of diabetic individuals compared to control subjects, with mainly type 1 patients being examined. In Mexico, a cross-sectional study on a sample of 175 type 1 and 2 diabetic patients found significantly poorer periodontal conditions in subjects affected by type 2 diabetes compared to a control group of non-diabetic individuals12.
The degree of metabolic control has been studied as a factor influencing increased prevalence of periodontal disease in diabetic subjects. Studies performed on patient samples in the USA and Finland have revealed that poorly controlled diabetic subjects had increased signs of periodontal disease, reflected as greater loss of attachment, deeper periodontal pockets and greater numbers of missing teeth13-16. A report on 181 diabetic patients in Singapore found that the percentage of glycated hemoglobin (HbA1c) was a significant predictor variable for percentage of bleeding on probing and percentage of periodontal pockets ¡Ý 5 mm17.
The aim of this study was to measure the occurrence of periodontal parameters in a group of Colombian type 2 diabetic patients, compared to a group of nondiabetic individuals, and at the same time to evaluate the possible relation between the degree of metabolic control and other medical and periodontal variables.
MATERIALS AND METHODS
An examination was performed on diabetic patients regularly attending the Program for Diabetes Control at the Medical School, National University of Colombia. The objective of this program is to provide medical care to subjects with diabetes registered in the university health system, mainly students, teachers and administrative personnel; it includes approximately 130 individuals. The program includes medical appointments every 3 months, laboratory examinations, counseling regarding diet and physical activity, and provision of equipment for glucose self-monitoring.
Study Individuals
All patients registered in the Program were screened for inclusion criteria and willingness to participate in a periodontal examination. After an explanation of examination procedures, all patients provided informed consent. Approval of the study was obtained from the Ethics Committee, Dental School, National University of Colombia. Inclusion criteria were:
• Diagnosis of type 2 diabetes mellitus
• Adherence to the Diabetic Control Program, Division of Lipids and Diabetes, Medical School, National University of Colombia
• Presence of at least six natural teeth
• Absence of systemic conditions that would require antibiotic prophylaxis for periodontal examination
A group of non-diabetic individuals of a similar age seeking general dental treatment at the Dental School was recruited for comparison. Subjects seeking periodontal care were excluded from the non-diabetic group.
Examination Procedures
Demographic, medical and periodontal variables were collected for all individuals. Demographic variables included age, gender and education level. The medical variables studied were HbA1c percentage, body mass index (BMI), time since diagnosis of diabetes (in months) and smoking status. A randomized half-mouth examination carried out by a single periodontitst (CS) was performed on four surfaces per tooth: mesio-lingual, mid-lingual, mid-buccal and disto-buccal. The periodontal examination included number of teeth, plaque accumulation, bleeding on probing, pocket depth (PD) and clinical attachment level (CAL). Plaque Index scores18 were calculated and dichotomized based on presence of visible plaque; scores 2 and 3 became a 1 value; scores 0 and 1 became a 0 value. Full-mouth percentage of bleeding on probing and percentage of pockets ¡Ý 4 mm were calculated. Measurements were carried out to the nearest millimeter using the UNC 15 probe (Hu-Friedy, Chicago, IL, USA).
The occurrence of severe periodontitis was descri - bed according to two different diagnostic criteria. The first criterion was according to the Center for Disease Control (CDC) Working Group19, which defined severe periodontitis as the presence of ¡Ý 2 interproximal sites with CAL ¡Ý 6 mm, and ¡Ý 1 interproximal sites with PD ¡Ý 5 mm. The second diagnostic criterion used a modification of the Biofilm-Gingival Interface (BGI) classification described by Offenbacher et al. (2007)20. According to the original criterion, a case defined as BGIdeep lesion had ¡Ý 1 sites with PD ¡Ý 4 mm and ¡Ý 50% percentage of bleeding on probing; for the present study the criterion was modified to select even more severe cases, as the PD inclusion criterion was ¡Ý 20% sites showing PD ¡Ý 4 mm. Repeated assessments were performed on five randomly selected individuals two months apart to calculate intra-examiner reproducibility. The reproducibility coefficient for PD measurements was 0.90; for NIC measurements it was 0.94.
Degree of Diabetic Metabolic Control
The diabetic subject sample was divided into three groups according to the degree of metabolic control: good control HbA1c < 7%, fair control HbA1c 7-7.9%, and poor metabolic control HbA1c ¡Ý 8%.
Statistical Analysis
All variables were analyzed for normal distribution using the Shapiro-Wilk test. Means and standard deviations were calculated for data description. Most results showed a non-normal distribution; therefore the differences in periodontal variables between the diabetic and non-diabetic group were analyzed using the Chi-square, Fisher Exact and Mann-Whitney test. The few results showing a normal distribution were analyzed using a t-test. When the diabetic sample was divided into three groups according to degree of metabolic control, differences among groups were studied by the Kruskal- Wallis test. The correlation between the various parameters studied was analyzed by Pearson´s partial correlation analyses. All analyses were performed using JMP v. 8.0 software. The level of statistical significance was set at p <0.05.
RESULTS
Sample Description
From an approximate total number of 130 diabetic patients regularly attending the Diabetic Control Program, a group of 72 type 2 diabetic subjects met the inclusion criteria to be examined. The majority of patients not having periodontal examination were completely edentulous, 27 patients. Other patients not included were type 1 diabetics, individuals undergoing periodontal treatment, having very few teeth remaining, or requiring medication modification or antibiotic prophylaxis before examination; others refused to participate in the study. The diabetic subjects were compared to a group of 39 nondiabetic patients of similar age.
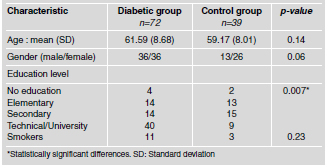
Demographic characteristics of the diabetic and control sample are summarized in Table 1. In general, the ages of subjects with and without diabetes were similar. The diabetic group included the same number of men and women, while the non-diabetic group included a larger number of women, but the differences were not statistically significant. The education level was significantly higher in the diabetic group, as a majority of individuals had university or technical education, compared to the non-diabetic group, where most subjects had elementary or secondary education. There were very few smokers in the two groups, and differences between groups were not statistically significant. Medical variables in diabetic subjects showed a mean HbA1c% level of 7.94 (1.60), range 5.4 to 12.6, revealing an average fair metabolic control of the diabetic condition. A total of 28 patients could be considered under good metabolic control, 18 were under fair metabolic control and 26 were under poor metabolic control. The time since diagnosis of diabetes had great variability, 83.59 (88.30) months, representing subjects with a long-term history of the disease as well as recent diagnosis of type 2 diabetes mellitus. Diabetic patients had slightly higher levels of BMI than non-diabetic patients, 27.77 kg/cm2 (3.91) compared to 25.69 kg/cm2 (2.99), respectively; nevertheless the mean values for both groups were in the overweight category.
Table 1: Comparison of demographic characteristics in diabetic and control groups.
Occurrence of Severe Chronic Periodontitis
For diabetic subjects, the two different criteria for establishing the presence of severe chronic periodontitis gave similar prevalence results; a total of 16 patients, equivalent to 22.22% of the sample, received this diagnosis. However, only 8 out of the 16 subjects were diagnosed with severe chronic periodontitis, according to both classification systems. For non-diabetic subjects, the two different criteria yielded different results; for the CDC Working Group criterion19, the disease occurrence was 23.07%, while for the modified BGI criterion20 it was 5.12%. The patients diagnosed with severe chronic periodontitis, according to the modified BGI criterion, were also included in the periodontitis group, based on the CDC Working Group criterion. Only for the modified BGI criterion was the occurrence of severe chronic periodontitis significantly higher in diabetic than in non-diabetic subjects, p<0.03. Periodontitis diagnosis according to the modified BGI criterion was significantly associated with HbA1c level, p<0.04; however no significant association was found with the dichotomized plaque index score p<0.53, smoking status p<0.90 and time since diabetes diagnosis p<0.66.
Comparison of Periodontal Parameters
Periodontal parameters of both study groups are summarized in Table 2. Half-mouth examination revealed that the number of teeth in the type 2 diabetic subjects was significantly higher than in the non-diabetic. In addition, diabetic patients had a significantly greater level of plaque accumulation and percentage of bleeding on probing. Mean values for PD and CAL were similar in both study groups. The percentage of sites with PD ¡Ý 4 mm was greater in diabetics than in non-diabetic individuals; however, differences were not statistically significant.
Table 2: Comparison of periodontal parameters in diabetic and control groups.

Effect of Different Degree of Metabolic Control on Periodontal Parameters
Poorer periodontal parameters were observed as metabolic control decreased (Table 3). Particularly, plaque accumulation and percentage of bleeding on probing were significantly different among the four groups. A pairwise comparison of the modified plaque index demonstrated significant differences between non-diabetic and poorly-controlled diabetic subjects, p<0.02, and between non-diabetic and diabetic patients with fair control, p<0.04.
Table 3: Comparison of periodontal parameters among non-diabetic controls, well-controlled, fairly-controlled and poorly-controlled diabetic patients.

Differences in percentage of bleeding on probing were significant between nondiabetic and poorly-controlled diabetic individuals, p<0.009, non-diabetic and diabetic subjects with fair control, p<0.002, well- and poorly-controlled diabetic patients, p<0.01, and patients with diabetes under good and fair control, p<0.009. It is noteworthy that no clinically significant difference was found between non-diabetic and well-controlled diabetic individuals. No significant difference was found between groups for mean PD and CAL measurements. A trend toward a larger percentage of pockets ¡Ý 4 mm as metabolic control got worse was detected; however it was not statistically significant. Comparison for percentage of pockets ¡Ý 4 mm between non-diabetic and poorly-controlled diabetic subjects had p<0.14, while that between well-controlled and poorly-controlled had p<0.16. Correlation analysis revealed a significant correlation of time since diabetes diagnosis and CAL level: r=0.39; p<0.01.(Fig.1A) HbA1c percentage had several significant correlations with periodontal parameters, the greatest correlation occurring with percentage of bleeding on probing, r=0.33, p<0.05 (Fig 1B) followed by visible plaque score, r=0.28; percentage of periodontal pockets, r=0.26; and mean PD, r=0.25 (p<0.05).

Fig. 1: Significant correlations between medical and periodontal parameters. A :DxDM: Time since diabetes diagnosis in months vs. CAL: Clinical attachment level (mm). r=0.39; p<0.01. B: HbA1c: Percentage of glycated hemoglobin vs. BoP%: Percentage of bleeding on probing. r=0.33, p<0.05.
DISCUSSION
The results of this study demonstrated poorer periodontal conditions in patients affected by type 2 diabetes mellitus, in agreement with findings of larger, population-based epidemiological studies7, 10, 11. Among this sample of diabetic patients, degree of metabolic control was associated with poorer periodontal status. An epidemiological study in USA by Tsai et al. 7 used similar criteria regarding CAL loss and PD measurements to define severe periodontitis; findings showed that poorly controlled diabetic patients were 2.90 times, and better controlled were 1.56 times, as likely to have periodontitis, compared to non-diabetic subjects; however differences were only significant for patients with poor diabetic control. A population-based study by Mattout et al 9 performed in France found significant differences between diabetic and nondiabetic individuals for plaque index and gingival index, a smaller difference for CAL, and similar values for PD. In contrast, an epidemiological study in Germany by Kaur et al.11 found larger PD depth CAL loss in type 2 diabetic subjects, but no significant difference for type 1 diabetic individuals. Similarly to the epidemiological studies described, our study found differences between diabetic and control groups related to plaque and gingival bleeding; whereas non-significant differences were found for PD depth and CAL loss7, 10, 11. A meta-analysis of 23 studies by Khader et al.18 found significantly poorer periodontal status for diabetic subjects compared to controls; based on seven studies, overall difference regarding PD depth was 0.34 mm ( C.I. 0.19-0.49), and based on eight studies, overall difference regarding CAL loss was 0.69 mm (C.I. 0.46-0.84). Several reasons could be considered for the lack of significant differences regarding PD depth and CAL loss between diabetic and non-diabetic groups in our study. Most of the diabetic subjects studied exhibited good or fair control of the diabetic condition, having been chosen from a small group of closely supervised patients at the diabetes control program, not similar to the heterogeneous subjects included in population-based epidemiological studies. The report by Tsai et al.7 found no significant difference for severe periodontitis diagnosis between non-diabetic and well-controlled diabetic subjects. Moreover, time since diabetes diagnosis varied greatly in the studied patients; a significant correlation was found between time since diagnosis and CAL loss, probably because some of the recently diagnosed diabetic subjects had not developed the cumulative loss of periodontal support characteristic of affected individuals. Therefore, presence of confounding factors could affect the influence of diabetic status on periodontal parameters. Diabetic and control groups did not have statistically significant differences regarding age, gender and smoking status; however education level was significantly lower in the control group. Several references have described poorer periodontal conditions in subjects with a low education level21,22. Finally, a control group taken from subjects seeking treatment at the dental school might vary in health status from the general population; however, the large number of missing teeth in the control group is characteristic for this age population, according to Colombian epidemiological studies23.
A few studies have analyzed the prevalence of periodontitis in diabetic patients in Latin American countries, including mainly type 1 patients; results have shown a widespread or more severe presentation of periodontitis in diabetic patients24,25. A report by Patiño-Marín et al.12 on type 1 or 2 Mexican diabetic subjects found that type 2 diabetic individuals had a significantly larger number of missing teeth, calculus index, PD and CAL12. Compared to the results of our study, the control subjects in the study by Patiño-Marín et al.12 had better oral health, with a smaller number of missing teeth, probably associated with the inclusion of a younger age range for patients, who were 30-60 years old. Multiple clinical signs and symptoms of periodontitis have led to wide variations in prevalence estimates of disease, which has prompted the adoption of uniform criteria26, which is the reason why the CDC Periodontal Surveillance Workgroup definition19 was used for prevalence analysis. Nevertheless, a different classification criterion was developed by Offenbacher et al.20 in an effort to identify biologic phenotypes at the BGI, based on presence of pockets and percentage of bleeding on probing. A modification to the original criterion including a higher threshold for number of pockets was made to ensure selection of severe cases. Severe periodontitis prevalence was similar in diabetic compared to non-diabetic subjects using the CDC Working Group criterion19, but it differed when using the modified BGI. This is the consequence of greater bleeding on probing and percentage of pockets in diabetics. Cross-sectional studies on type 1 diabetics showed a greater tendency to gingival bleeding than controls, despite similar levels of plaque accumulation27-29.
Longitudinal and cross-sectional studies have described the influence of degree of metabolic control on periodontal parameters, finding poorer clinical conditions in poorly controlled diabetics13-16. Similar results were found in our study, particularly for percentage of bleeding on probing and visible plaque scores, in addition to a greater percentage of periodontal pockets. In particular, all subjects with HbA1c levels ¡Ý 10% showed a percentage of bleeding on probing ¡Ý 50%. A study on 181 diabetics by Lim et al.17 also found that inadequate metabolic control correlated with percentage of bleeding on probing and pockets ¡Ý 5 mm. A study on type 1 diabetics by Ternoven et al.30 found greater bone loss in type 1 diabetics as metabolic control worsened, but the differences were not statistically significant. In contrast, a study by Bridges et al.31 did not find any influence of degree of metabolic control on periodontal parameters; however this sample of type 1 and 2 diabetic subjects exhibited general poor metabolic control with HbA1c values ranging from 9.2 to 11.1%.
Within the limits of this study, it can be concluded that this sample of Colombian type 2 diabetic patients had poorer periodontal conditions than a group of non-diabetic individuals, the differences being significant for plaque accumulation and percentage of bleeding on probing. The prevalence of severe periodontitis varied considerably, depending on criteria for case selection. A worse degree of metabolic control level was significantly associated with greater severity of periodontal inflammatory parameters.
ACKNOWLEDGMENTS
The authors are grateful for the valuable collaboration of the following undergraduate research assistants, School of Dentistry, National University of Colombia: Ximena Gómez, Andrea Martínez, Angela Másmela and Sandra Zorro.
1. American Diabetes Association.org. Diabetes statistics: 2011 National Diabetes Fact Sheet, updated 26 January 2011; cited 8 June 2011, available from http://www.diabetes.org/diabetesbasics/diabetesstatistics [ Links ]
2. Townsend T. A decade of diabetes research and development. Int J Diabetes Metab 2000;8:88-92. [ Links ]
3. Wild S, Roglik G, Green A, Sicree R, King H. Global prevalence of diabetes. Diabetes Care 2004;27:1047-1053. [ Links ]
4. Adeghate E, Schattner P, Dunn E. An update in the etiology and epidemiology of diabetes mellitus. Ann N Y Acad Sci 2006;1084:1-29. [ Links ]
5. Stumvoll M, Goldstein BJ, van Haeften TW. Type 2 diabetes: principles of pathogenesis and therapy. Lancet 2005; 365: 1333-1346. [ Links ]
6. Zimmet P, Alberti KG, Shaw J. Global and societal implications on the diabetes epidemic. Nature 2001;414:782-787. [ Links ]
7. Tsai C, Hayes C, Taylor GW. Glycemic control of type 2 diabetes and severe periodontal disease in the US adult population. Community Dent Oral Epidemiol 2002; 30: 182-192. [ Links ]
8. Nelson RG, Shlossman M, Budding LM, Pettit DJ, Saad MF, Genco RJ, Knowler WC. Periodontal disease and NIDDM in Pima Indians. Diabetes Care 1990;13:836-846. [ Links ]
9. Emrich LJ, Shlossman M, Genco RJ. Periodontal disease in non-insulin dependent diabetes mellitus. J Periodontol 1991; 62:123-130. [ Links ]
10. Mattout C, Bourgeois D, Bouchard P. Type 2 diabetes and periodontal indicators: epidemiology in France 2002-2003. J Periodont Res 2006;41:253-258. [ Links ]
11. Kaur G, Holtfreter B, Rathmann WG, Schwahn C, Wallaschofski H, Schipf S, Nauck M, Kocher T.. Association between type 1 and type 2 diabetes with periodontal disease and tooth loss. J Clin Periodontol 2009;36:765-774. [ Links ]
12. Patiño-Marín N, Rodríguez Loyola JP, Medina Solis CE, Pontigo Loyola A, Reyes Macías JF, Ortega Rosado JC, Aradillas García C. Caries, periodontal disease and tooth loss in patients with diabetes mellitus types 1 and 2. Acta Odontol Latinoam 2008;21:127-133. [ Links ]
13. Ternoven T, Oliver RC. Long-term control of diabetes mellitus and periodontitis. J Clin Periodontol 1993;20:431-435. [ Links ]
14. Safkan-Seppala B, Ainamo J. Periodontal conditions in insulin-dependent diabetes mellitus. J Clin Periodontol 1992; 19:24-29. [ Links ]
15. Seppala B, Seppala M, Ainamo J. A longitudinal study on insulin-dependent diabetes mellitus and periodontal disease. J Clin Periodontol 1993;20:161-165. [ Links ]
16. Seppala B, Ainamo J. A site-by-site follow-up study on the effect of controlled versus poorly controlled insulin-dependent diabetes mellitus. J Clin Periodontol 1994;21: 161-165. [ Links ]
17. Lim LP, Tay FBK, Sum CF, Thai AC. Relationship between markers of metabolic control and inflammation on severity of periodontal disease in patients with diabetes mellitus. J Clin Periodontol 2007;34:118-123. [ Links ]
18. Loe H. The Gingival Index, the Plaque Index, and the Retention Index system. J Periodontol 1967;38:610-616. [ Links ]
19. Page RC, Eke PI. Case definitions for use in populationbased surveillance of periodontitis. J Periodontol 2007;78: 1378-1399. [ Links ]
20. Offenbacher S, Barros SP, Singer RE, Moss K, Williams RC, Beck JD. Periodontal disease at the biofilm-gingival interface. J Periodontol 2007;78:1911-1925. [ Links ]
21. Paulander J, Axelssson P Lindhe J. Association between level of education and oral health status in 35-, 50-, 65- and 75- year-olds. J Clin Periodontol 2003;30:697-704. [ Links ]
22. Siukosaari P, Ajwani S, Ainamo A, Wolf J, Närhi T. Periodontal health status in the elderly with difference level of education: a 5 year follow-up study. Gerodontology 2012; 29: e170-8. doi: 10.1111/j.1741-2358.2010.00437. [ Links ]
23. Franco AM, Suarez E, Tovar S, Jácome S, Ruiz JA. Indices CPO-D. In: Ministerio de Salud de Colombia, III Estudio Nacional de Salud Bucal. Bogotá: República de Colombia, Ministerio de Salud 1999: 90-96. [ Links ]
24. Pavez V, Araya V, Rubio A, Ríos L, Meza P, Martínez B. Periodontal health status in patients with diabetes mellitus type 1, from 18 to 30 years-old, from Santiago, Chile. Rev Med Chil 2002;130:402-408. [ Links ]
25. Novaes Jr AB, Pereira AL, de Moraes N, Novaes AB. Manfestations of insulin-dependet diabetes mellitus in the perio dontium of Young Brazilian patients. J Periodontol 1991;62:161-163. [ Links ]
26. Borrell LN, Papapanou PN. Analytical epidemiology of periodontitis. J Clin Periodontol 2005; 32:132-158. [ Links ]
27. de Pommereau V, Dargent-Paré C, Robert JJ, Brion M. Periodontal status in insulin-dependent diabetic adolescent. J Clin Periodontol 1992;19:628-632. [ Links ]
28. Karjalainen KM, Knuuttila MLE. The onset of diabetes and poor metabolic control increases gingival bleeding in children and adolescents with insulin-dependent diabetes mellitus. J Clin Periodontol 1996;23:1060-1067. [ Links ]
29. Salvi GE, Kandylaki M, Troendle A, Persson GR, Lang NP. Experimental gingivitis in type 1 diabetics: a controlled clinical and microbiological study. J Clin Periodontol 2005; 32:310-316. [ Links ]
30. Ternoven T, Karjalainen K, Knuuttila M, Huumonen S. Alveolar bone loss in type 1 diabetic subjects. J Clin Periodontol 2000;27:567-571. [ Links ]
31. Bridges RB, Anderson JW, Saxe SR, Gregory K, Bridges SR. Periodontal status of diabetic and non-diabetic men: Effects of smoking, glycemic control, and socioeconomic factors. J Periodontol 1996;67:1185-1192. [ Links ]














