Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Acta Odontológica Latinoamericana
versión On-line ISSN 1852-4834
Acta odontol. latinoam. vol.26 no.1 Buenos Aires abr. 2013
ARTÍCULOS ORIGINALES
Bruxism. Masticatory implications and anxiety
Anne C. Alves1, João C. Alchieri2, Gustavo A. S. Barbosa3
1 Speech Therapist, Federal University of Rio Grande do Norte, Brazil.
2 Psychology Department, Federal University of Rio Grande do Norte, Brazil.
3 Dentistry Department, Federal University of Rio Grande do Norte, Brazil.
CORRESPONDENCE Anne da Costa Alves Rua do Calcario, 100 - apt.203 - Lagoa Nova Natal, RN - Brazil. Postal Code: 59076-240 E-mail: annecalves@hotmail.com
ABSTRACT
In this study we investigate the phenomenon of bruxism, defined as the act of clenching and/or grinding the teeth, a habit that compromises the orofacial region. It is often associated with emotional aspects, such as anxiety and stress, and may result in alterations to orofacial structures, functional modifications and social repercussions. The aim of this study was to determine a possible association between bruxism and anxiety underscoring the primary complaints related to masticatory function. Eighty volunteers participated in the study. They were divided into bruxers (N=40) and non-bruxers (N=40) of both sexes. The diagnosis of bruxism was made by clinical examination. The Trait-State Anxiety Inventory was used to assess anxiety levels and a questionnaire with structured questions related to daily activities, focusing on masticatory function (for the bruxism group), was applied to evaluate psychosocial aspects. The results of the study show a significant difference in state anxiety. Mean and standard deviation of state anxiety in the bruxism and non-bruxism groups was 42.7}9.6 and 38.6}8.2 (p ≤0.04), respectively, while trait anxiety had a mean and standard deviation of 44.5}11.0 and 40.7}9.5 (p ≤0.11). The main complaints of bruxers during mastication were facial pain and headache while chewing as well as the presence of clicking sounds in the jaw joint. Findings demonstrate an association between emotional factors such as anxiety and bruxism, resulting in compromised masticatory function.
Key words: Anxiety; Bruxism; Mastication; Stomatognathic System.
Bruxismo implicações mastigatórias e ansiedade
RESUMO
Neste trabalho procuramos estudar o fenomeno do bruxismo, definido como o ato de apertar e/ou ranger os dentes, um habito prejudicial e destrutivo da regiao orofacial. O bruxismo e frequentemente associado aos aspectos emocionais, entre os mais ressaltados a ansiedade e o estresse, podendo implicar em alteracoes das estruturas orofaciais, modificacoes funcionais e repercussoes sociais. Verificar a associacao entre bruxismo e ansiedade ressaltando as principais queixas referentes a funcao mastigatoria. Participaram oitenta voluntarios, divididos entre grupo com bruxismo (N=40) e sem bruxismo (N=40), do sexo masculino e feminino. O diagnostico do bruxismo foi realizado atraves do exame clinico. Para avaliar os niveis de ansiedade empregou-se o "Inventario de Ansiedade Traco e Estado" e para os aspectos psicossociais um questionario com questoes estruturadas referentes as atividades diarias, focando a funcao mastigatoria (para o grupo com bruxismo). Foram evidenciadas diferencas significativas para a ansiedade estado entre os grupos analisados, verificou-se a media e desvio padrao de ansiedade estado no grupo com bruxismo, 42,7}9,6 e sem bruxismo 38,6}8,2 (p ≤0,04) e de ansiedade traco respectivamente 44,5}11,0 e sem bruxismo 40,7}9,5 (p ≤0,11). O relato dos participantes com bruxismo evidenciou como principais queixas durante a mastigacao a dor na face ao mastigar, cansaco muscular na face, cefaleia ao mastigar e presenca de ruidos articulares. Com base nos resultados evidenciamos uma associacao dos fatores emocionais como a ansiedade e o bruxismo e como resultante os pacientes apontam que a funcao mastigatoria encontrase depreciada.
Palavras-chave: Ansiedade; Bruxismo; Mastigacao; Sistema Estomatognatico.
INTRODUCTION
Bruxism is a nighttime or daytime parafunctional activity, characterized by clenching or grinding of the teeth1. It is considered the most harmful and destructive habit affecting the orofacial region2,3, due to the non-functional tooth wear that occurs in situations not involving mastication, swallowing and phonation4. The mandibular movements with no functional purpose observed in bruxism impose an abnormal demand on masticatory muscles, resulting in hyperfunction, generating painful symptoms and decreased coordination5 when the force exerted by the habit exceeds the adaptive capacity of the stomatognathic system6.
Tooth grinding involves a sliding movement of occlusal surfaces in eccentric contact, favoring tooth wear. During tooth clenching, the increased tension in centric occlusion, through the isometric contraction of jaw elevator muscles, may cause pain, fatigue and masticatory muscle hypertrophy. The neuromuscular system becomes compromised as a consequence of atypical functional demand imposed on the muscles involved, also affecting mastication7.
Although bruxism is a frequent habit in adults6, 8, 9, its causal factors are complex and still not fully understood2, 10. Until a few years ago peripheral factors, such as occlusal disorders and anatomical alterations, were the most commonly implicated. However, current research has questioned the action of occlusion on the origin of bruxism, promoting conceptual change that suggests the influence of central and psychogenic factors2, 4, 11, 12. Thus, it is believed that the multifactorial theory may be the most plausible hypothesis2, 10, 12-14.
The influence of emotional factors, such as anxiety, has been widely emphasized, for both triggering and perpetuating bruxism, resulting in an increase in muscle tension caused by emotional stress during moments of anxiety15, manifesting itself somatically, i.e., a form of body language that cannot be understood by the subject16. Anxiety is an emotional state triggered by the body, which includes both psychological and physiological components, becoming pathological when exaggerated or disproportional in relation to the trigger. This leads to disruption and failure to perform its role as a psychobiological alarm, with the potential to develop into a pathology when exceeding the individual's adaptive capacity17, 18. Based on this evidence and the non-conclusive data contained in the literature regarding the influence of emotional factors on bruxism, the aim of this study was to determine the association between bruxism and anxiety, underscoring the primary complaints related to masticatory function.
MATERIALS AND METHODS
This is a comparative cross-sectional descriptive study, approved by the Research Ethics Committee at the Federal University of Rio Grande do Norte, Brazil, under protocol No. 065/09. All participants provided informed written consent, after being informed of the objectives and methods to be used. Data were collected among all patients with bruxism who sought treatment at the Integrated Care Center for Patients with Stomatognathic Apparatus Dysfunction (CIADE) between April 2009 and April 2011, as part of an extension project for the Occlusion course in the Dentistry Department of the Federal University of Rio Grande do Norte.
The non-probabilistic sample was composed of 80 subjects of both sexes, divided into Group 1 - bruxism and Group 2 - non-bruxism. The inclusion criterion was that only adults would be considered for both groups. Exclusion criteria were individuals with neurological disorders and patients who had undergone orthognathic or disccondyle complex surgery. For the group with bruxism, individuals who reported clenching/ grinding their teeth, indicating the need for an occlusal splint and pain in the orofacial region, were included. The bruxism group was composed of 40 patients, (37 women and 3 men), mean age 33.4 } 11.5 years.
The non-bruxism group contained 40 individuals, (36 women and 4 men), mean age 36.3 } 10.1 years. In addition to clinical examination, bruxism was also evaluated through a self-report instrument, based on a previous study19, 20. The survey asked the following questions: Do you wake up in the morning or during the night clenching or grinding your teeth? (yes/no); Do you feel fatigue or masticatory muscle pain on awakening? (yes/no); Do you wake up in the morning or during the night with your jaws locked? (yes/no); Do you have recent history of chronic dislocation of permanent or temporary restorations? (yes/no); Do you have recent history of noises associated with nocturnal teeth grinding as reported by a third person? (yes/no).
Clinical examination revealed signs and symptoms of bruxism, as reported in the literature21, based on the patient's primary complaints. The evaluation was performed by dental students, previously trained and supervised by professors, recording the following: presence of tooth wear (yes/no); dental fractures (yes/no); periodontal trauma (yes/no); masseter and temporal muscle pain (yes/no); muscle hypertrophy (yes/no); restricted mandibular movement (yes/no); sensitivity in head and neck muscles (yes/no) and joint noise (clicking and/or popping) (yes/no).
A translated and validated Portuguese version22 of the State-Trait Anxiety Inventory (STAI), an instrument developed by Spielberg, Gorsuch and Lusheneem (1964), was used to identify and characterize the anxiety level of participants. It consists of two self-report questionnaires: 1) Stateanxiety and 2) Trait-anxiety. The survey, which assesses state-anxiety, consists of 20 statements in which patients indicate how they feel at a particular point in time. The trait-anxiety questionnaire contains 20 items and is designed to determine patient personality characteristics throughout their lives. It is important to point out that this instrument was used in both groups. Moreover, the State-Trait Anxiety Inventory was employed after application of the self-report instrument and assessment of clinical indicators of bruxism, prior to the dental procedure. Thus, intergroup differences in relation to state anxiety may result from administration of the State-Trait Anxiety Inventory after dental consultation. A structured questionnaire developed by the researchers was also applied. It contained closed questions related to the masticatory functions in daily activities (only for the bruxism group in order to investigate its implications and face pain symptoms), enquiring about type of teeth clenching and/or grinding and when it occurs (daytime, nighttime or both). Next, subjects were asked how bruxism-related face pain interferes in activities of daily living, (emphasizing masticatory function) such as sleep; appetite /eating; swallowing; speech; restricted mandibular movements and mastication - When chewing, do you experience facial pain, tired facial muscles, headache and joint noise?
Data were transcribed onto a standard patient record and inserted into a data bank for statistical analysis using SPSS 16.0 software. In the descriptive analysis, quantitative variables are presented as mean and standard deviation (sd), while categorical data are depicted in tabular form, as absolute and relative frequency. Student's t-test for independent samples was applied to compare the means of continuous independent variables in relation to the groups. Pearson's chi-square test (X2) was used to compare differences in the proportion of independent variables to dependent variables with respect to the groups. A p-value of 0.05 and confidence interval of 95% were adopted for all tests.
RESULTS
Analysis of sociodemographic aspects of the bruxism group demonstrated higher prevalence of women (37 = 92.5%) than men (3 = 7.5%), with mean age and standard deviation of 33.4}11.5, and prevalence of single individuals (18 = 45.0%). The non-bruxism group was composed of 36 (90.0%) women and 4 (10.0%) men, mean age 36.3} 10.1, the majority of whom are married (26=65.0%).
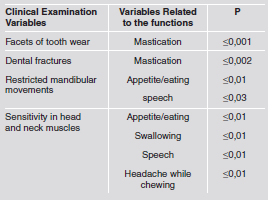
State-trait anxiety data for both groups are shown in Table 1. In relation to the characterization of bruxism with respect to the habit of clenching and/or grinding the teeth and the point in time at which it occurred can be seen in Table 2. Data from clinical examinations of bruxism related to daily functions and activities, (Table 3) showed a significant assocation in the following: tooth wear with impaired mastication (≤0.001); dental fractures with impaired mastication (≤0.002); restricted mandibular movements, influencing appetite/eating (≤0.01) and hindering speech (≤0.03); sensitivity in head and neck muscles, showing associations with appetite/eating (≤0.01), swallowing difficulties (≤0.01), speech difficulties (≤0.01) and headache while chewing (≤0.01). Based on the accounts of patients with bruxism and the main complaints observed during mastication, significant associations were found for appetite/ diet (≤0.004), facial pain when chewing (≤0.007), facial muscle fatigue(≤0.004), headaches (≤0.02) and joint noise (≤0.001).
Table 1: Distribution of means and standard deviations of anxiety in the bruxism and non-bruxism groups.

*≤0.05%
Table 2: Characterization of the bruxism group regarding the habit of clenching and grinding their teeth and when the habit occurs.

Table 3: A significant association between the clinical examination of bruxism and the variables related to daily functions activities.
DISCUSSION
Several recent studies have sought to determine the relationship between bruxism and emotional aspects, highlighting anxiety13, 23, 24 as one of the psychological factors that play an important role in triggering and perpetuating the parafunction. The greater prevalence of women with bruxism can be explained by different theories, including physiological and biological differences among molecular factors related to gender, somewhat associated to "facilitation" of pathologies involving the temporomandibular joint, such as cases of morphological, rheumatic and psychosocial diseases25; as to cognitive level, pain threshold may be lower in women than in men; with regard to social differences, different upbringing between girls and boys may make it more acceptable for women to externalize pain than men26. Moreover, women are more aware of the need to seek treatment25.
Bruxism is defined as "an anxiety response to environmental stress". Emotional factors such as anxiety, fear, frustration and emotional stress are related to muscle hyperactivity3, 27. Strengthening this hypothesis, Manfredini et al. determined that psychological traits such as anxiety, depression and maniacal symptoms, as well as stress sensitivity, show significant differences in individuals with bruxism, whereas occlusal factors showed no significant difference12, 28.
This study demonstrated a relationship between anxiety and bruxism, showing significant state anxiety differences in individuals with bruxism when compared to the control group. State anxiety is characterized as a transitory emotional reaction to everyday stressful events2. It consists of an unpleasant feeling of anxiety and stress activated by the autonomous central nervous system29 that can vary in time and intensity30. Increased stateanxiety in individuals with bruxism occurs when nociceptive stimuli reach the central nervous system, and are directed not only to the cerebral cortex, but also to the limbic structures, which assess and influence the painful experience on an emotional level. In other words, pain is caused by complex interactions in the higher centers. It is important to underscore that the face, an essential human structure, is the primary means of eating and communicating, allowing interaction with others to display our emotions, objectives and opinions, as well as providing sources of both physical and emotional gratification and satisfaction. Changes to the orofacial segments associated with pain symptoms may increase insecurity and threaten individual wellbeing. They result in altered body image and can be influenced by psychological aspects, including anxiety31. Thus, it is believed that high state-anxiety levels may be related to the presence of pain symptoms. No difference was found for trait anxiety, in contrast to findings in the literature - Da Silva et al.32 - which report greater propensity to trait anxiety in bruxers. Researchers such as Gungormus and Erciyas observed that people who grind their teeth have higher levels of anxiety and depression13. Along these lines, Kampe et al. found that individuals with bruxism had different personalities from the normal population, displaying greater tendency towards anxiety, increased vulnerability to psychosomatic disorders and difficulty in social relationships27. However, a study conducted by Manfredini et al. showed no association between bruxism and psychopathological anxiety23. Rompre et al. report that levels of anxiety and stress do not differ between control and experimental groups33. Clinical diagnosis of bruxism has provided a detailed description of psychosocial problems in individuals with bruxism, underscoring psychological issues, stress, anxiety, mood disorders, temperamental and emotional traits, as well as social matters such as work and personal relationships, all of which could have a negative effect on health2.
In addition to personality traits, the relationship between living conditions and bruxism has also been explored. It regularly manifests itself in individuals affected by stress, which determines the frequency, duration and severity of the condition3. The literature reports that individuals with sleep bruxism experience greater stress in their daily lives and at work, compromising their physical status and causing them to deal with stressful situations in a negative manner10. This opinion is also common among patients, who often report increased teeth grinding during sleep and at stressful moments in their life2, reacting with negative emotions. Although the relationship between bruxism and stress is still inconclusive, it is suggested that elevated levels of daily stressful events may be a risk factor23. However, Pierce et al. found no significant relationship between electromyographic measurements recorded over 15 consecutive nights and self-reports of stress in individuals with bruxism, demonstrating significance only for eight of the one hundred subjects evaluated34.
Diagnosis of bruxism is complex due to the various assessment criteria, such as self-reports, clinical evaluation, electromyography and polysomnography, with questionnaires being the most widely used method21. In this study, self-reports and clinical assessments were adopted as diagnostic criteria. Questionnaires to determine bruxism are generally used in epidemiological studies and clinical situations21 owing to their low cost and rapid diagnosis. However, this method does not distinguish between clenching and grinding teeth during sleep or during the day23. Polysomnography is the gold standard for diagnosing sleep bruxism, but the method is limited by its high cost. Diagnostic criteria do not clearly distinguish between sleep and daytime bruxism or its severity23. A recent literature review suggests that self-reports of bruxism may be adequate for detecting conscious teeth clenching during wakefulness, which may be associated with masticatory muscle sensitivity or fatigue, whereas analysis of tooth wear or sleep laboratory recordings are more appropriate for detecting teeth grinding, whose implications may be different from clenching35.
It is important to underscore that anxiety may manifest itself physiologically in different ways, including bruxism, caused by the increase in muscle tension, evidenced by hyperactive masticatory muscles, especially the masseter24. Bruxism is the most harmful and destructive habit to affect the orofacial region, due to the fact that mandibular movements with no functional purpose2, 12, 35 cause masticatory dysfunction8.
A large proportion of complaints from individuals with bruxism are related to the masticatory function, since the association between clinical data and psychosocial aspects of daily activities shows a significant correlation with chewing disorders. It is important to note that mastication occurs via interaction between morphological aspects of orofacial structures, muscle and joint functional capacity, as well as food characteristics36. The bilateral pattern of chewing favors the health of orofacial structures25. This indicates that constant bruxism generates alterations in the normal physiological process of masticatory muscles4. It is a parafunctional habit that threatens the integrity of oral structures, since the force exerted exceeds the adaptive capacity of the masticatory system and the functional equilibrium of the stomatognathic system may be altered, causing a series of signs and symptoms6, highlighting alterations in dental structures, joint noise and facial pain. The altered mastication observed implies that persistent bruxism prolongs the excitability of afferent nociceptors of the masticatory and facial muscles, resulting in sensitization. This increases the painful stimulus, particularly in areas close to the oral cavity and those related to chewing. As such, it is believed that bruxism can be detrimental to the masticatory function8. It is also a risk factor for temporomandibular dysfunctions (TMD) 12, 23, 35. Some authors have analyzed the association between bruxism, symptoms of temporomandibular dysfunction and pain, hypothesizing that bruxism may be one of the causes8, and a contributing factor for TMD4. A recent systematic literature review on the relationship between bruxism and temporomandibular dysfunction showed a positive association between them, based on clinical diagnostic or self-report methods, whereas quantitative methods for bruxism diagnosis - polysomnography and electromyography - demonstrate low association for TMD symptoms35.
Implications that patients report during mastication corroborate the findings of Sutin et al. who found that individuals with bruxism complained of joint noise and chewing difficulties37. In order to investigate the relationship between bruxism and craniofacial pain and masticatory symptomatology, Ciancaglini et al. demonstrated a complex association among the variables analyzed, underscoring difficulty with opening the mouth, joint noise, sensitivity or mandibular muscle fatigue and pain during mandibular movements8. Pizolato et al. analyzed maximum bite force in patients with temporomandibular dysfunction and bruxism, reporting that the presence of pain in the facial region is related to marked functional compromise4. It is believed that distribution of muscle strength in the teeth and temporomandibular joints of individuals with bruxism may result in tooth wear as well as hyperactivity and masseter muscle hypertrophy4.
Modification in orofacial muscles and the stomatognathic functions of chewing, swallowing and speaking characterize an orofacial myofunctional disorder. This may be associated with causal factors of the dysfunctions, provoking an imbalance in the functioning of the temporomandibular joint. It may also be the result of nociceptive stimulation caused by occlusion and/or the temporomandibular joint, which may provoke compensatory muscle behavior that can aggravate or perpetuate the problem25. Alterations in mastication and other orofacial behavior may provoke a significant change in mechanical load of one temporomandibular joint (TMJ) or the other. TMDs involve changes in stomagtognathic functions as well as in lip and tongue position owing to the presence of nociceptive stimuli, triggered by occlusion and/or TMJ. These modifications are considered a compensatory or adaptive response, aimed at facilitating masticatory function and preserving structures in order to minimize pain and avoid discomfort. Unilateral mastication in individuals with TMD causes irregular movement, such as slowness, altered direction of movement and increased pain when chewing, where individuals opt for the side with greater masticatory efficiency25. It is important to note that unilateral mastication in patients with TMD involves considerable risk of pain and increased signs and symptoms of dysfunction. Furthermore, compromised mastication occurs if functional adaptation exceeds structural and functional tolerance of TMJ, which may trigger dysfunction38.
Bruxism causes changes in stomatognathic functions and structures, negatively affecting wellbeing when painful symptoms are present. As stated in research by Macfarlane et al. on orofacial impact, the most prominent effects resulted in consulting a dentist or doctor, taking medication, sleep disturbances and changes in eating habits. In addition to more severe behavioral impacts, we also highlight the inability to work, need for bed rest and reduced social contact, where patients reported a less satisfactory life26, negatively affecting their emotional health.
In conclusion, individuals with bruxism displayed significant differences in state anxiety, in contrast to the non-bruxism group, showing an association between emotional factors and bruxism. The masticatory function in patients with bruxism was reduced, which may be the result of hyperactivity of the masticatory muscles caused by increased muscle tension. Due to the sample size and type of study employed, and considering the results observed, a limitation of this study was that its findings cannot be generalized. It is suggested that future investigations on masticatory function and orofacial myofunctional disorders should strive for better diagnostic and therapeutic methods, as well as employ interdisciplinary teams in a biopsychosocial context.
ACKNOWLEDGMENTS
The authors are grateful to the Department of Dentistry for its support and encouragement of research and development.
1. Lavigne GJ, Khoury S, Abe S, Yamaguchi T, Raphael K. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil 2008;35:476-494. [ Links ]
2. Manfredini D, Lobbezoo F. Role of psychosocial factors in the etiology of bruxism. J Orofac Pain 2009;23: 153-166. [ Links ]
3. Katayoun E, Sima F, Naser V, Anahita D. Study of the relationship of psychosocial disorders to bruxism in adolescents. J Indian Soc Pedod Prev Dent 2008; 26 Suppl 3:S91-97. [ Links ]
4. Pizolato RA, Gaviao MB, Berretin-Felix G, Sampaio AC, Trindade Junior AS. Maximal bite force in young adults with temporomandibular disorders and bruxism. Braz Oral Res 2007;21:278-283. [ Links ]
5. Blini CC, Morisso MF, Bolzan GP, Silva AMT. Relacao entre bruxismo e o grau de sintomatologia de disfuncao temporomandibular. Rev CEFAC 2010;12:427-433. [ Links ]
6. de la Hoz-Aizpurua JL, Diaz-Alonso E, Latouche- Arbizu R, Mesa-Jimenez J. Sleep bruxism. Conceptual review and update. Med Oral Patol Oral Cir Bucal 2011; 1:231-238. [ Links ]
7. Almeida FL, Silva AMT, Correa ECR, Busanello AR. Relacao entre dor e atividade eletrica na presenca de bruxismo. Rev CEFAC 2011;13:399-406. [ Links ]
8. Ciancaglini R, Gherlone EF, Radaelli G. The relationship of bruxism with craniofacial pain and symptoms from the masticatory system in the adult population. J Oral Rehabil 2001;28:842-848. [ Links ]
9. Castelo PM, Barbosa TS, Gaviao MB. Quality of life evaluation of children with sleep bruxism. BMC Oral Health 2010;10:16. [ Links ]
10. Giraki M, Schneider C, Schafer R, Singh P, Franz M, Raab WH, Ommerborn MA. Correlation between stress, stresscoping and current sleep bruxism. Head Face Med 2010;6:2. [ Links ]
11. Winocur E, Uziel N, Lisha T, Goldsmith C, Eli I. Selfreported bruxism - associations with perceived stress, motivation for control, dental anxiety and gagging. J Oral Rehabil 2011;38:3-11. [ Links ]
12. Bayar GR, Tutuncu R, Acikel C. Psychopathological profile of patients with different forms of bruxism. Clin Oral Investig 2012;16:305-311. [ Links ]
13. Gungormus Z, Erciyas K. Evaluation of the relationship between anxiety and depression and bruxism. J Int Med Res 2009;37:547-550. [ Links ]
14. Restrepo CC, Vasquez LM, Alvarez M, Valencia I. Personality traits and temporomandibular disorders in a group of children with bruxing behaviour. J Oral Rehabil 2008; 35:585-593. [ Links ]
15. Fissmer JFW, Garanhani RR, Sakae TM, Traebert JL, Filho EJS. Relacao entre ansiedade e bruxismo em academicos de odontologia. ACM Arq Catarin Med 2008;37:25-29. [ Links ]
16. Molina OF, Sobreira MA, Tavares PG, Dib JE, Aquilino RN. Anxiety in craniomandibular disorders and bruxing behaviour patients: the role of pain in single and multiple sites and severity of bruxing behaviour. Part I: inclusion of the extreme behaviour group and report of preliminary psychological data on anxiety. Rev Neurocienc 2006; 14:23-30. [ Links ]
17. Andrade LHSG, Gorenstein C. Aspectos gerais das escalas de avaliacao de ansiedade. Rev Psiquiatr Ciln 1998;25: 285-290. [ Links ]
18. Duarte D, Hubner MMC. Ansiedade, bruxismo e aprendizagem: uma analise comparativa em alunos da 7a serie do ensino fundamental. Psicol Teor Prat 1999;1:43-52. [ Links ]
19. Calderon Pdos S, Kogawa EM, Lauris JR, Conti PC. The influence of gender and bruxism on the human maximum bite force. J Appl Oral Sci 2006;14:448-453. [ Links ]
20. Molina OF, dos Santos Junior, Nelson SJ, Nowlin T. A clinical study of specific signs and symptoms of CMD in bruxers classified by the degree of severity. Cranio 1999; 17:268-279. [ Links ]
21. Koyano K, Tsukiyama Y, Ichiki R, Kuwata T. Assessment of bruxism in the clinic. J Oral Rehabil 2008;35: 495-508. [ Links ]
22. Gorenstein C, Andrade LH. Validation of a Portuguese version of the Beck Depression Inventory and the State-Trait Anxiety Inventory in Brazilian subjects. Braz J Med Biol Res 1996;29:453-457. [ Links ]
23. Manfredini D, Landi N, Fantoni F, Segu M, Bosco M. Anxiety symptoms in clinically diagnosed bruxers. J Oral Rehabil 2005;32:584-588. [ Links ]
24. Basson RA, Mwaba K, Rossouw RJ, Geerts GAVM, Kotze TJV, Stuhlinger ME. The significance of sub-threshold symptoms of anxiety in the aetiology of bruxism. S Afr J Psychol 2010;40:119-124. [ Links ]
25. Ferreira CL, Da Silva MA, de Felicio CM. Orofacial myofunctional disorder in subjects with temporomandibular disorder. Cranio 2009;27:268-274. [ Links ]
26. Macfarlane TV, Blinkhorn AS, Davies RM, Kincey J, Worthington HV. Oro-facial pain in the community: prevalence and associated impact. Community Dent Oral Epidemiol 2002;30:52-60. [ Links ]
27. Kampe T, Edman G, Bader G, Tagdae T, Karlsson S. Personality traits in a group of subjects with long-standing bruxing behaviour. J Oral Rehabil 1997; 24:588-593. [ Links ]
28. Manfredini D, Landi N, Romagnoli M, Bosco M. Psychic and occlusal factors in bruxers. Aust Dent J 2004;49: 84-89. [ Links ]
29. Bellini M, Marini I, Checchi V, Pelliccioni GA, Gatto MR. Self-assessed bruxism and phobic symptomatology. Minerva Stomatol 2011;60:93-103. [ Links ]
30. Guillen-Riquelme A, Buela-Casal G. Psychometric revision and differential item functioning in the State Trait Anxiety Inventory (STAI). Psicothema 2011;23: 510-515. [ Links ]
31. Okeson JP. A psicologia da dor. In: Okeson JP, editor. Dores Bucofaciais de Bell. Sao Paulo: Quintessence, 1998;93-102. [ Links ]
32. da Silva AM, Oakley DA, Hemmings KW, Newman HN, Watkins S. Psychosocial factors and tooth wear with a significant component of attrition. Eur J Prosthodont Restor Dent 1997;5:51-55. [ Links ]
33. Rompre PH, Daigle-Landry D, Guitard F, Montplaisir JY, Lavigne GJ. Identification of a sleep bruxism subgroup with a higher risk of pain. J Dent Res 2007;86:837-842. [ Links ]
34. Pierce CJ, Chrisman K, Bennett ME, Close JM. Stress, anticipatory stress, and psychologic measures related to sleep bruxism. J Orofac Pain 1995;9:51-56. [ Links ]
35. Manfredini D, Lobbezoo F. Relationship between bruxism and temporomandibular disorders: a systematic review of literature from 1998 to 2008. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:26-50. [ Links ]
36. Berretin-Felix G, Genaro KF, Trindade IEK, Trindade Junior AS. Masticatory function in temporomandibular dysfunction patients: electromyographic evaluation. J Appl Oral Sci 2005;13:360-365. [ Links ]
37. Sutin AR, Terracciano A, Ferrucci L, Costa PT. Teeth Grinding: Is Emotional Stability related to Bruxism? J Res Pers 2010;44:402-405. [ Links ]
38. de Felicio CM, de Oliveira MM, da Silva MA. Effects of orofacial myofunctional therapy on temporomandibular disorders. Cranio 2010;28:249-259. [ Links ]














