Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Acta Odontológica Latinoamericana
versión On-line ISSN 1852-4834
Acta odontol. latinoam. vol.27 no.2 Buenos Aires set. 2014
ARTÍCULOS ORIGINALES
The influence of mandibular ridge anatomy on treatment outcome with conventional complete dentures
Jaiane A.M. Ribeiro1, Camila M.B.M. de Resende1, Ana L.C. Lopes1, Arcelino Farias-Neto2, Adriana da F.P. Carreiro1
1 Department of Dentistry, Federal University of Rio Grande do Norte, Natal, Brazil.
2 Health School, Potiguar University – Laureate International Universities, Natal, Brazil.
CORRESPONDENCE Dr. Arcelino Farias-Neto Health School, Potiguar University– Laureate International Universities Rua dos Potiguares, 2421, Lagoa Nova, Natal – RN, Brazil e-mail: a.fariasneto@yahoo.com.br
ABSTRACT
Since prognostic indicators are likely to take on increasing importance as a diagnostic tool for selection of patients for implant provision, this study investigated the influence of the shape and resiliency of the mandibular alveolar ridge on the retention and stability of conventional complete dentures. Ninety- three edentulous patients wearing both maxillary and mandibular conventional complete dentures composed the sample. Data were collected regarding shape and resiliencyof the mandibular residual ridge. Dentures were assessed for retention and stability using an objective and reproducible tool.The associations between the clinical characteristics of the mandibular alveolar ridge and denture retention and stability were analyzed using chi-square and Fisher exact tests (a = 0.05). A significant association between ridge shape and denture stability (p < 0.05) was found, while ridge resiliency was significantly associated to denture retention (p < 0.001). Based on the results, mandibular ridge shape and resiliency influenced the retention and stability of conventional complete dentures.
Key words: Complete denture; Denture retention; Patient satisfaction.
RESUMO
Influência da anatomia do rebordo mandibular no tratamento com próteses totais convencionais
Visto que indicadores de prognostico sao uma ferramenta importante para a selecao de pacientes a serem tratados com protese total, este estudo investigou a influencia da forma e da resiliencia do rebordo alveolar mandibular sobre a retencao e estabilidade de proteses totais convencionais. Noventa e tres pacientes desdentados portadores de proteses totais superior e inferior compuseram a amostra. Os dados foram coletados quanto a forma e resiliencia do rebordo mandibular. As proteses foram avaliadas para a retencao e estabilidade utilizando-se uma ferramenta objetiva e reproduzivel. As associacoes entre as caracteristicas clinicas do rebordo alveolar mandibular e retencao e estabilidade das proteses foram analisados por meio dos testes qui-quadrado e exato de Fisher (a = 0.05). Observou-se associacao significativa entre a forma do rebordo e a estabilidade da protese (p <0,05), enquanto que a resiliencia foi associada significativamente com a retencao (p <0,001). Baseando-se nos resultados, a resiliencia e forma do rebordo mandibular influenciaram, respectivamente, a retencao e estabilidade de proteses totais convencionais.
Palavras-chave: Protese total; Retencao em protese total; Satisfacao do paciente.
INTRODUCTION
Successful treatment with conventional complete dentures depends to a great extent on the patient's ability to use the denture. The problem is how to identify, through oral examination, which patients have suitable conditions for denture use1. Denture stability is defined the resistance of a denture to movement on its tissue foundation, especially to lateral forces as opposed to vertical displacement (termed denture retention)2. Patients usually complain less about comfort and retention of the maxillary than of the mandibular denture2,3. The maxillary residual ridge often has a more favorable shape, and is less resorbed and resilient than its mandibular counterpart. According to Baat et al.,4 patient's adaptation to complete dentures is strongly related to the prosthetic condition, which combines denture quality and residual ridge characteristics. Thus, the discrepancy between the dentist's evaluation of denture quality and the patient's subjective judgment may result from inappropriate assessment of the quality of the denture-bearing surfaces4.
After attending 723 patients seeking complete denture treatment, Fenlon's group concluded that the shape of the residual edentulous ridge influences patients' satisfaction and the use of new dentures5,6. In another study, denture satisfaction correlated to submandibular/sublingual salivary flow rate, oral musculature characteristics and mandibular ridge shape7. Mandibular ridge shape has also been related to masticatory efficiency8 and ability9. It is seems obvious that better ridge shape will result in a more stable and retentive denture, and consequently better patient acceptance. However, some studies have found that residual ridge form has no influence on patient satisfaction10,11. According to a recent review of the literature, studieson this area are equivocal and lack standardized methodologies for direct comparison2.
Since prognostic indicators are likely to take on increasing importance as a diagnostic tool for selection of patients for implant provision, the need for further research in this area has never been higher2. Therefore, the purpose of this study was to investigate whether the shape and resiliency of the mandibular alveolar ridge are related to denture retention and stability using a standardized and reproducible methodology. The research hypothesis is that mandibular ridge anatomy may influence treatment outcome with conventional complete dentures.
MATERIAL AND METHODS
The study was approved by the institution's Research Ethics Committee. All edentulous patients treated at the Prosthodontics Clinic between 2004 and 2009 were invited to participate in this cross-sectional study. After a preliminary examination, patients were excluded if they exhibited xerostomia, severe oral manifestations of systemic diseases or psychological or psychiatric conditions that could influence data collection. In addition, dentures were evaluated by an experienced prosthodontist and patients were excluded if at least one of the following features was inappropriate: extension of the denture base in relation to the optimal available denture bearing area, peripheral seal, border extension, tissue fit, and balanced occlusion in retruded contact position. The sample was composed of 93 edentulous patients (18 male, 75 female), mean age 65.6 years (SD 9,2) wearing both mandibular and maxillary dentures for at least two months and less than 5 years. After providing informed consent, patients answered a personal information questionnaire (name, address, phone number, age, gender). Data were collected regarding shape (Cawood and Howell classification12) and resiliency7 of the mandibular residual ridge (Table 1).
Table 1: Clinical assessment of the oral condition and denture quality.
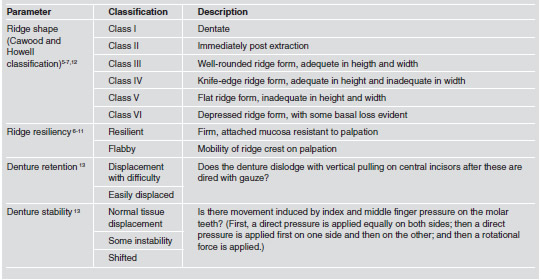
The factors and criteria for evaluation of retention and stability of the mandibular denture were set up according to Sato et al.13 (Table 1). Data were collected by a single examiner to avoid inter-examiner variability. Prior to the clinical examinations, the examiner participated in the calibration process, which was divided into theoretical discussions of codes and criteria for the study, as well as practical activities. Data were processed with SPSS software (V 17.0 for Windows, SPSS Inc, Chicago, IL, USA). The associations between the clinical characteristics of the mandibular alveolar ridge and denture retention and stability were analyzed using chi-square and Fisher exact tests. Confidence level was set at 95%.
RESULTS
The ridge resiliency was classified as flabby in 62 patients (63.3%) and resilient in 31 patients (31.6%). According to Cawood and Howell's classification12, seventy ridges were Class III (75.3%), 15 were Class IV (16.1%), and 8 were Class V (8.6%). Seventy-three mandibular dentures were easily displaced (78.5%), while 20 were displaced with difficulty (21.5%). Regarding denture stability, 43 were within normal tissue pattern (46.2%), 27 had some instability (29%), and 23 shifted (24.7%). Mandibular ridge shape was significantly associated to denture stability (p < 0.05), but did not influence denture retention (Table 2). Ridge resiliency was significantly associated to denture retention (p < 0.001), but not to denture stability (Table 3).
Table 2: Relationship between the shape of the mandibular ridge and denture stability and retention.

* Significantly associated to ridge shape (p< 0.05)
Table 3: Relationship between the resiliency of the mandibular ridge and denture retention and stability.
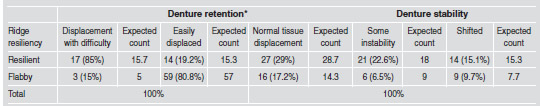
* Significantly associated to ridge resiliency (p< 0.05)
DISCUSSION
The results of this study support the research hypothesis that mandibular ridge anatomy may influence treatment outcome with conventional complete dentures. Mandibular ridge shape was significantly associated to denture stability (p < 0.05). Eighty-two percent of the dentures that shifted during the stability test were associated to a flat ridge (Class V). In addition, ridge resiliency was associated to denture retention (p < 0.001). Direct comparison of these results to other studies was not possible because no study with the same purpose was identified. However, these results corroborate previous findings regarding the influence of ridge shape on patient satisfaction6,7 and the use of new dentures5. Fenlon's group observed a strong influence of ridge shapeonmandibular denture stability and security which in turn strongly influenced jaw relations5,6. This was shown to have a significant influence on usage of and satisfaction with new dentures5,6.
It was expected that the shape and resiliency of the mandibular ridge would influence both denture retention and stability. However, ridge shape was associated only to denture stability (p < 0.05), but not to retention. In addition, ridge resiliency was associated to retention (p < 0.001), but not stability. These results may be related to the factors and criteria for evaluation of retention and stability. It is possible that the height and width of the alveolar ridge may be more relevant to prevent denture dislodgement under rotational forces, while a resilient ridge prevents dislodgement under vertical forces.
It seems logical to assume that better ridge shape would promote improved retention and stability, and consequently better patient acceptance2. However, some studies have found contradictory results10,11. Celebic et al.10 concluded that patients rated as having the best mandibular ridge shapes were the least satisfied with their new lower denture, and those given the best rating for maxillary ridge shape were more satisfied with their upper denture10. Another study examined a sample of 130 patients and found no influence of physical condition of the mouth on patients' satisfaction11. These contrasting results may be related to differences in the methodologies used to assess retention and stability, as well as the criteria adopted for ridge shape classification. Our study used clear, direct criteria for objective assessment of the functional factors of a dental prosthesis13. The method proposed by Sato et al.13 has been shown to be broad, trustworthy, reliable and reproducible13. Assessment of the ridge shape followed the classification proposed by Cawood and Howell.12 This ridge classificationsystem has been used in previous studies which reported similar results5-7.
According to Batt et al.,4 successful treatment with conventional complete dentures depends on both denture quality and oral conditions. Thus, it is reasonable to conclude that patients' rating of technically appropriate dentures may be low due to their residual ridge characteristics. The American College of Prosthodontists has developed a classification system for complete edentulism that is based on specific diagnostic criteria, such as mandibular bone height, morphologic features of the maxillary residual ridge, mandibular muscle attachment and maxillomandibular relationship. Edentulism is divided into 4 levels of difficulty or complexity, and the highest level designates patients who require the most difficult degree or complexity of treatment14. Several factors other than a patient's oral conditions may also influence denture retention and stability. Stability can be further improved with precise linear centric occlusion15. Denture instability may be caused by oblique forces during functional and parafunctional activities as well as errors during the recording of maxillo-mandibular relations1,5. Inadequate intermaxillary relationship may have a negative impact on denture retention16. In addition to the dentist's technical skills and clinical expertise, the patient's psychological profile may influence treatment outcome16. Psychological evaluation should be carried out to determine patient's attitudes regarding denture use2.
Patients with a negative opinion of their dentures are often less satisfied.11 In addition, subjects with no previous experience of denturesare less satisfied than those who have already worn one or more pairs of dentures2. To summarize, using a standardized and reproducible methodology, this study showed that mandibular ridge anatomy may influence treatment outcome with conventional complete dentures. The shape of the mandibular ridge may influence denture stability, while ridge resiliency may influence denture retention. Prognostic indicators are likely to take on increasing importance as a diagnostic tool for selection of patients for implant provision. Previous studies done in this area are equivocal and lack standardized methodologies for direct comparison2. However, it must be emphasized that successful prosthodontic therapy is likely to be multifactorial, and the clinical characteristics of alveolar ridges alone may not predict treatment outcomes4.
1. Wright CR. Evaluation of the factors necessary to develop stability in mandibular dentures. J Prosthet Dent 2004;92: 509-518. [ Links ]
2. Critchlow SB, Ellis JS. Prognostic indicators for conventional complete denture therapy: a review of the literature. J Dent 2010;38:2-9. [ Links ]
3. Wolff A, Gadre A, Begleiter A, Moskona D, Cardash H. Correlation between patient satisfaction with complete dentures and denture quality, oral condition, and flow rate of submandibular/ sublingual salivary glands. Int J Prosthodont 2003;16:45-48. [ Links ]
4. deBaat C, van Aken AA, Mulder J, Kalk W."Prosthetic condition" and patients judgment of complete dentures. J Prosthet Dent 1997;78:472-478. [ Links ]
5. Fenlon MR, Sherriff M, Walter JD. An investigation of factors influencing patients' use of new complete dentures using structural equation modelling techniques.Community Dent Oral Epidemiol 2000;28:133-140. [ Links ]
6. Fenlon MR, Sherriff M. An investigation of factors influencing patients' satisfaction with new complete dentures using structural equation modelling. J Dent 2008;36: 427-434. [ Links ]
7. Wolff A,Gadre A,Begleiter A, Moskona D, Cardash H. Correlation between patient satisfaction with complete dentures and denture quality, oral condition, and flow rate of submandibular/ sublingual salivary glands. Int J Prosthodont 2003;16:45-48. [ Links ]
8. Koshino H, Hirai T, Ishijima T, Ohtomo K. Influence of mandibular residual ridge shape on masticatory efficiency in complete denture wearers. Int J Prosthodont 2002;15: 295-298. [ Links ]
9. Koshino H, Hirai T, Yokoyama Y, Tanaka M, Toyoshita Y, Iwasaki K, Sudo E. Mandibular residual ridge shape and the masticatory ability in complete denture wearers. Nihon HotetsuShikaGakkaiZasshi 2008;52:488-493. [ Links ]
10. Celebic A, Knezovic-Zlataric D, Papic M, Carek V, Baucic I, Stipetic J. Factors related to patient satisfaction with complete denture therapy. J Gerontol A BiolSci Med Sci 2003; 58:M948-953. [ Links ]
11. Van Waas MA. The influence of clinical variables on patients' satisfaction with complete dentures. J Prosthet Dent 1990;63:307-310. [ Links ]
12. Cawood JI, Howell RA. A classification of the edentulous jaws. Int J Oral MaxillofacSurg 1988;17:232–236. [ Links ]
13. Sato Y, Tsuga K, Akagawa Y, Tenma H. A method for quantifying complete dentures quality. J Prosthet Dent 1998;80: 52-57. [ Links ]
14. Mazurat RD, Mazurat NM. Communicating complexity: using a diagnostic classification system for edentulous patients. J Can Dent Assoc 2003;69:511-514. [ Links ]
15. Gronas DG, Stout CJ. Lineal occlusion concepts for complete dentures. J Prosthet Dent 1974;32:122-129. [ Links ]
16. Laurina L, Soboleva U. Construction faults associated with complete denture wearers' complaints. Stomatologija 2006; 8:61-64. [ Links ]














