Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Acta Odontológica Latinoamericana
On-line version ISSN 1852-4834
Acta odontol. latinoam. vol.28 no.1 Buenos Aires Apr. 2015
ARTÍCULOS ORIGINALES
Do resin cements influence the cuspal deflection of teeth restored with composite resin inlays?
Helen C.V. da Rosa1, Maurem L. Marcondes1, Niélli C. de Souza1, João B. B. Weber2, Ana M. Spohr3
1 Department of Restorative Dentistry, School of Dentistry, Pontifical Catholic University of Rio Grande do Sul, Brazil.
2 Department of Preventive Dentistry, Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil.
3 Department of Dental Materials, School of Dentistry, Pontifical Catholic University of Rio Grande do Sul, Brazil.
CORRESPONDENCE Dr. Ana Maria Spohr PUCRS – School of Dentistry, Block 6 Avenida Ipiranga, 6681, 90619-900 Porto Alegre, RS, Brazil. E-mail: ana.spohr@pucrs.br
ABSTRACT
The aim of this study was to evaluate the influence of different resin cements on the cuspal deflection of endodontically treated teeth restored with composite resin inlays. Sixty upper premolars were randomly divided into five groups (n=12): 1 – sound teeth; 2 – cavity; 3 - Rely X ARC; 4 – RelyX Unicem; 5 – SeT. The teeth from groups 2, 3, 4 and 5 received a MOD preparation and endodontic treatment. Impressions were made with vinyl polysiloxane and poured using type IV die stone in groups 3, 4 and 5. Inlays with composite resin were built over each cast and luted with the resin cements. A 200 N load was applied on the occlusal surface, and cuspal deflection was measured using a micrometer. After 24 h, cuspal deflection was measured again using a 300 N load. The Student t-test showed that there was no statistically significant difference between the 200 N and 300 N occlusal loads only for the sound teeth group (p = 0.389) and the RelyX ARC group (p = 0.188). ANOVA and Tukey'test showed that the sound teeth had the lowest mean cuspal deflection, differing statistically from the other groups (p<0.05). The highest cuspal deflections were obtained in the SeT group and the cavity group, with no statistical difference between them. Intermediate values were obtained in RelyX ARC group and RelyX Unicem group, which differed statistically. The self-adhesive resin cements RelyX Unicem and SeT showed less capacity to maintain the stiffness of the tooth/restoration complex than the conventional resin cement RelyX ARC.
Key words: Endodontics; Resin cements.
RESUMO
Os cimentos resinosos influenciam a deflexão de cúspides de dentes restaurados com inlays em resina composta?
O objetivo deste estudo foi avaliar a influencia de diferentes cimentos resinosos na deflexao de cuspides de dentes tratados endodonticamente e restaurados com inlays em resina composta. Sessenta pre-molares foram divididos aleatoriamente em cinco grupos (n=12): grupo 1 – dentes higidos; 2 – cavidade; 3 - Rely X ARC; 4 – RelyX Unicem; 5 – SeT. Os dentes dos grupos 2, 3, 4 e 5 receberam preparos cavitarios MOD e tratamento endodontico. Foram realizadas moldagens com silicone por adicao nos grupos 3, 4 e 5, seguido de vazamento de gesso tipo IV. Inlays em resina composta foram construidas sobre os modelos de gesso, sendo as inlays cimentadas com os cimentos resinosos. Uma carga de 200 N foi aplicada na face oclusal, e a deflexao de cuspide foi medida usando um micrometro. Apos 24 h, a deflexao de cuspide foi medida novamente sob carga de 300 N. De acordo com o teste t-Student, nao houve diferenca estatistica na deflexao de cuspides apenas para o grupo dos dentes higidos (p = 0.389) e o grupo do RelyX ARC (p = 0.188) quando comparada as duas cargas. De acordo com ANOVA e o tese de Tukey, os dentes higidos tiveram a menor media de deflexao de cuspides, diferindo estatisticamente dos outros grupos (p<0.05). A maior deflexao de cuspides foi obtida com o grupo SeT e o grupo cavidades, nao diferindo estatisticamente entre si. Valores intermediarios foram obtidos para os grupos RelyX ARC e RelyX Unicem, diferindo estatisticamente entre si. Os cimentos resinosos autoadesivos RelyX Unicem e SeT mostraram menor capacidade de manter a rigidez do complexo dente/restauracao em comparacao com o cimento resinoso RelyX ARC.
Palavras-chave: Tratamento endodontico; Cimento resinoso.
INTRODUCTION
As a result of their structural design, posterior teeth naturally suffer cuspal deflection under load. When endodontic treatment and mesio–occlusal–distal (MOD) preparations are performed, this trend towards cuspal deflection under masticatory loads is increased 1,2 due to the decrease in the stiffness of the tooth 3. It is a consequence of the removal of dental tissues, which leads to greater fragility of the dental structure 4,5.
Numerous techniques and restorative materials have been indicated to recover the stiffness of endodontically treated teeth 6,7. The most frequently used materials are composite resins and ceramics, due to esthetic demands. In the case of composite resin restorations, the indirect technique is considered the best treatment option to restore teeth with large cavities and to overcome polymerization shrinkage 8. These indirect restorations are luted with adhesive materials, such as adhesive systems associated with resin cements, which favor reinforcement of the weakened tooth 9-11. The conventional adhesive luting procedure consists of applying an adhesive system followed by a resin cement. However, self-adhesive resin cements have gained popularity with clinicians because they are easy to use, and the luting procedure takes less time than resin cements, which require the application of an adhesive system. Without the adhesive system, part of the sensitivity of the technique is eliminated 12,13.
Self-adhesive resin cements interact superficially with tooth hard tissues, and the formation of a hybrid layer or resin tags was not observed 14-16. Self-adhesive resin cements have lower bond strength with enamel than do resin cements requiring an adhesive system 12, 17. In relation to dentin, studies have shown that self-adhesive resin cements perform comparably to multistep systems on coronal dentin 12, 14, 17- 19. In contrast, other studies have shown significantly lower bond strengths of these materials to dentin 20- 22.
In an inlay restoration, the luting material occupies the space between the restoration and the tooth, and is responsible for connecting these different substrates. Regardless of the luting technique, the tooth/restoration complex must be capable of restoring the stiffness of the original tooth to a certain degree, in order to decrease mechanical fatigue of the cusps 23, which increases with higher occlusal loads 1. However, there is no study showing the influence of resin cements on cuspal deflection under different occlusal loads. The aim of this study was to evaluate the influence of three resin cements on cuspal deflection, under two different occlusal loads, of endodontically treated maxillary premolars restored with composite resin inlays. This study was conducted under the hypotheses that there are differences in the amount of cuspal deflection between inlays luted with the different resin cements.
MATERIALS AND METHODS
MOD preparation
Sixty sound maxillary first premolars, extracted for therapeutic reasons, were obtained from a tooth bank after the approval of the Ethics Committee of the Pontifical Catholic University of Rio Grande do Sul. The teeth were cleaned and disinfected in 10% thymol for 24 h and stored in 4° C distilled water. The water was changed every week, and the teeth were used within 6 months. The buccal–palatal and mesio–distal dimensions of each tooth were measured with a digital caliper (Mitutoyo, Suzano, SP, Brazil). A variation of 0.5 mm was allowed for each measurement to standardize the dimensions of the teeth. Each tooth was mounted vertically in a plastic cylinder with self-cured acrylic resin (Jet Classico, Sao Paulo, SP, Brazil), up to 2 mm below the cement–enamel junction (CEJ). The teeth were randomly divided into 5 groups (n=12): Group 1, sound teeth (control); Groups 2, 3, 4, and 5, teeth with MOD preparation and endodontic treatment. Group 2 was not restored, and the other groups were restored with composite resin inlays, which were luted with RelyX ARC (Group 3), RelyX Unicem (Group 4), and SeT (Group 5). Table 1 shows the composition and manufacturer details of the materials used.
Table 1: Resin cements used in the study.

A single operator performed the MOD preparations using a standardized preparation machine. This device consisted of a high-speed handpiece (Kavo, Joinville, SC, Brazil) attached to a mobile base. The mobile base moves vertically and horizontally, in 3 mm increments, with the aid of a micrometer (Mitutoyo, Tokyo, Japan). The long axis of the tooth was positioned vertically on the preparation machine, and the tooth was cut using a #4159 diamond bur (KG Sorensen, Barueri, SP, Brazil) attached to the high-speed handpiece under constant water and air cooling. The preparations presented rounded internal angles, divergent walls, and an occlusal box width of two-thirds of the intercuspal distance. The depth of the proximal boxes was located 1 mm above the CEJ. The preparations had only buccal and palatal walls, and a common floor from mesial to distal, so that the pulp floor of the occlusal box and the gingival floor of the proximal boxes were unified on the same level. The diamond bur was replaced after every five preparations. After the preparations were completed, endodontic access was prepared with a #8 spherical carbide burr (SS White, Lakewood, NJ, USA). The preparation of the chamber was round and expulsive. Flexo-File files (Kerr, Orange, CA, USA) from number 15 to 40 were manually placed in the root canals to standardize the preparation.
A 2.5% sodium hypochlorite solution was used to irrigate and clean the root canal. After the root canal preparation, all teeth were filled with gutta-percha cones (Dentsply Maillefer, Ballaigues, Switzerland) and N-Rickert endodontic sealer (Inodon, Porto Alegre, RS, Brazil) using the lateral condensation technique. Excess sealer was removed from the cavity using a cotton pellet soaked in 70% ethanol. The access to root canals was covered with gutta-percha.
Restorative procedures
Impressions of the preparations were taken with Express XT polyvinyl siloxane (3M Espe, Saint Paul, MN, USA) using individual trays made from self-cured acrylic resin (Jet Classico, Sao Paulo, SP, Brazil) with the putty/wash one-step technique. The impression material was allowed to set for 10 min before removal from the preparation. After 1 h, the impressions were poured using Durone Type IV stone (Dentsply, York, PA, USA). After 1 h, the casts were removed from the impression, numbered according to their group, and placed in dry storage. Cavity surfaces were lined with two coats of a die spacer, maintaining a distance of 1.0 mm to the marginal areas. Four horizontal layers of Filtek Z250XT composite resin (3M Espe, Saint Paul, MN, USA) were inserted in the casts, with Thompson spatulas no. 2 and 12, which resulted in a 90° inclination between the internal slopes and cusps. Each resin layer was light cured for 40 s. Restorations were then light cured for 60 s on each free surface, followed by finishing with flexible disks (TDV, Pomerode, SC, Brazil) and 8093F and 8093 FF silicone tips (KG Sorensen, Cotia, SP, Brazil). Throughout the experiment, a quartz-tungsten-halogen curing unit (Optilux Plus, Ribeirao Preto, SP, Brazil) was used for photopolymerization. The light intensity was controlled by a radiometer (model 100, Demetron/Kerr, Danbury, CT, USA) in the interval between 450 and 500 mW/cm2.
Luting procedures
The internal surfaces of the inlays were sandblasted with 50 μm aluminum oxide for 5 s, followed by silane application (Ceramic Primer, 3M Espe, Saint Paul, MN, USA). In Group 3, Scotchbond Multi- Purpose adhesive system (3M Espe, Saint Paul, MN, USA) was applied. The tooth preparations were etched with 37% phosphoric acid for 15 s, followed by rinsing with air and water spray for 15 s. Excess water was removed with absorbent paper. A layer of primer was applied, followed by gentle air drying for 5 s. Then the bond was applied with a microbrush and light cured for 10 s. Equal lengths of base and catalyst pastes of RelyX ARC resin cement were mixed for 15 s and put on the inlay and preparation. In Group 4, equal quantities of base and catalyst pastes of RelyX Unicem were mixed and applied on the inlay and preparation. In Group 5, the internal content of a capsule of SeT was activated for 10 s and applied on the inlay and preparation. In Groups 3, 4, and 5, the inlay was placed on the preparation and a 10 N load was applied by means of a metallic tool. After 2 min, excess cement was removed with a microbrush, followed by light curing for 60 s on each free surface. The specimens were stored in distilled water at 37° C for 72 h and then submitted to the cuspal deflection test.
Cuspal deflection testing
Resin spheres (approximately 1.5 mm in diameter) were fixed with adhesive on both cusps. Following the methodology described by Gonzales-Lopez et al.2 the spheres were positioned on the cuspal apexes and served as reference points for measuring the intercuspal distance, using a precision micrometer (Mitutoyo, Suzano, SP, Brazil) to the nearest 1 μm. A device was used to fix the micrometer in the same position for every measurement. Each specimen was attached to the lower platen of a universal testing machine (Emic DL-2000, EMIC, Sao Jose dos Campos, PR, Brazil), and a steel sphere with an 8 mm diameter was used to apply a 200 N occlusal load at a cross-head speed of 0.5 mm/min. The load was applied parallel to the long axis of the tooth, simultaneously contacting the buccal and palatal cuspal inclines (Fig. 1). When the 200 N load was achieved, the machine was locked and three consecutive measurements of the cuspal deflection were made. The mean distance of the composite resin spheres prior to application of the load was subtracted from the mean distance of the spheres after application of the load. Thus, the cuspal deflection value was obtained. After 24 h, the cuspal deflection was measured again using a 300 N load.
Fig. 1: Schematic figure of the cuspal deflection test: a) tooth; b) resin spheres; c) micrometer.
Statistical analysis
All statistical analyses were performed using SPSS version 10.0 (SPSS Inc., Chicago, IL, USA). After data collection, cuspal deflection data were submitted to the Kolmogorov–Smirnov normality test. To compare the study groups under the same load, the ANOVA and Tukey parametric statistical tests were applied. To compare each group under the different loads, student t-test for dependent samples was applied. The significance level was 5%.
RESULTS
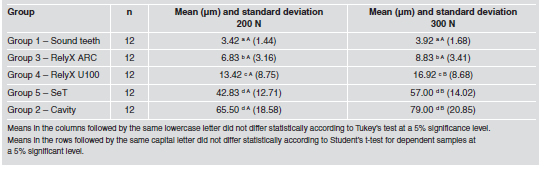
The ANOVA showed that there were statistically significant differences among the groups (p<0.05). For both occlusal loads, the sound teeth had the lowest mean cuspal deflection, differing statistically from the other groups. The highest cuspal deflections were obtained in SeT group and cavity group, with no statistical difference between them. Intermediate values were obtained in RelyX ARC group and RelyX Unicem group, which differed statistically. The Student t-test showed that there were statistically significant differences between the 200 N and 300 N occlusal loads for the cavity group (p = 0.002), the RelyX Unicem group (p = 0.000), and the SeT group (p = 0.004). There was no statistical difference for the sound teeth group (p = 0.389) or the RelyX ARC group (p = 0.188) (Table 2).
Table 2: Mean cuspal deflection and standard deviation of the groups under 200 N and 300 N loads.
DISCUSSION
The hypothesis was accepted, as there were differences in cuspal deflection among the experimental groups. Premolars were used in this study because they have an unfavorable anatomic shape, crown volume and crown/root proportion, making them more susceptible to cusp fractures than other posterior teeth when submitted to occlusal load 24. The dimensions of the cavity preparation were standardized in all groups, representing a clinical situation of advanced caries, for which preparation becomes extensive. Cuspal deflection is a non-destructive methodology that verifies the deformation of the cusps when a load is applied in the occlusal region. In this study, a 200 N occlusal load was applied to perform the cuspal deflection test. The 200 N load is the intermediate value between 100 and 300 N, which corresponds to the range of normal biting force for maxillary premolars 25,26. Cuspal deflection under a 300 N load was also verified. According to Jantarat et al.1, a load of up to 300 N can be applied without the risk of tooth fracture. The results showed that the application of greater occlusal load produced an increase in intercuspal distance, in agreement with the study by Gonzalez-Lopez et al. 2. This finding proves that the deformation depends on the intensity of the force applied 1.
The highest cuspal deflection was obtained for the cavity group, and the lowest values for the sound teeth. This small cuspal deflection in sound teeth is due to the very stiff behaviour of sound teeth under load 1. Intact teeth with a complete enamel covering are very stiff, and an occlusal load causes only a small deformation. Sound teeth distribute loadgenerated stress more homogeneously, because the enamel is not appreciably deformed and the deformation is transferred to the more resilient dentin 27. When the continuity of the enamel is lost as a result of preparation, the properties of the dentin play a major role in cusp behaviour 28. Loss of dental structure causes a decrease in tooth stiffness, and consequently there is an increase in cuspal deflection under occlusal loads 1,2. It is important to recover the stiffness of the teeth after restoration. Nevertheless, when the teeth were restored with composite resin inlays and luted with RelyX ARC, RelyX Unicem or SeT, none of the groups replicated the stiffness of natural teeth.
Among the restored groups, RelyX ARC had the lowest cuspal deflection. RelyX ARC is a conventional resin cement that is applied with an adhesive system. In this study, the preparation was etched with 37% phosphoric acid, followed by primer and bond applications, which allow hybrid layer formation on enamel 29 and dentin 30. The micro-mechanical retention obtained with the hybrid layer may explain the smaller cuspal deflection in the RelyX ARC group than in the RelyX Unicem and SeT groups. RelyX Unicem had the third lowest value of cuspal deflection. It is a self-adhesive resin cement that consists of alkaline fillers and specific multifunctional phosphoric-acid methacrylates, which are ionized at the time of mixing and which react with the hydroxyapatite of the mineral tissues of the tooth 31. On dentin, this material was unable to demineralize or dissolve the smear layer completely, no decalcification and infiltration of dentin occurred and no hybrid layer or resin tag was observed 14,17,32. The bond mechanism of RelyX Unicem to the tooth appears to be more chemical rather than micromechanical in nature. As RelyX Unicem have lower bond strength to enamel 12,19 and dentin 20- 22 than do multistep systems, the bond to the dental tissues may not have been as strong as the bond encountered at the DEJ or when a hybrid layer is formed. This may explain the higher mean cuspal deflection of the RelyX Unicem than of the sound teeth and RelyX ARC groups.
An alternative for increasing the bond strength of self-adhesive resin cements was to apply phosphoric acid etching on the enamel 12,19,33, and polyacrylic acid on the dentin 32,34 before the application of selfadhesive resin cements. The presence of the smear layer has been recognized as the weak link in bonding self-adhesive resin cements 18,32. These pretreatments represent an additional step in the application of self-adhesive resin cements, which were developed with the aim of simplifying the application procedure. However, it would be interesting to conduct the same study of cuspal deflection when specific pretreatments are applied on enamel and dentin before luting with RelyX Unicem, once all the inlay margins of the prepared teeth were within enamel, and a significant quantity of dentine was exposed by the inlay preparation. The self-adhesive resin cement SeT contains an acid monomer that is responsible for etching the tooth surface. However, it is not known specifically what type of acid monomer is used, or whether it has a chemical interaction with the tooth. In the study conducted by Stona et al.32, the adhesion of SeT to dentin did not withstand the cutting methodology used to obtain the test specimens (beams) for evaluating microtensile bond strength. It probably presented less interaction with dental substrates than RelyX Unicem, explaining the highest cuspal deflection.
Comparing 200-N and 300-N occlusal loads, RelyX ARC was the only resin cement that allowed an increase in cuspal deflection without statistical difference. The micro-mechanical retention obtained with the hybrid layer formed on enamel and dentin by the 37% phosphoric acid etching and subsequent adhesive polymerization is probably important for bond stability when the load is increased. In the case of inlay restoration, the stiffness of the tooth tends to be restored when the material used for luting bonds strongly with the tooth tissues and restorative material, with the formation of a monobloc restoration, in which two bond interfaces are formed, corresponding to the tooth/luting material and restoration/luting material. Among the experimental groups in the present study, variation occurred only at the tooth interface. The same treatment was used at the restoration interface, which consisted of sandblasting with 50 μm aluminum oxide, followed by silane application. According to Zang and Degrange 35, the adhesion of self-adhesive resin cements to the restorative material depends on the nature of the multifunctional monomer contained in the formulation, and these luting agents have potential for specific adhesion to selective restorative substrates. In addition, the different viscosities and the different penetration capabilities of the RelyX ARC, RelyX Unicem and SeT into surface irregularities may have influenced the adhesion of the resin cements to the inlay restoration.
The clinical importance of cuspal deflection is that the greater the magnitude of this deflection, the greater the deformation, and consequently, the greater the possibility of fatigue failure. This type of failure, characterized by fracture in the presence of stress far below the maximum strength of the restored tooth, occurs in most dental fractures 36. The result obtained for cuspal deflection showed that the self-adhesive resin cements RelyX Unicem and SeT showed less capacity to maintain the stiffness of the tooth/restoration complex than did the conventional resin cement RelyX ARC, which may foster greater longevity of the restored tooth. However, clinical studies are necessary to confirm this supposition.
1. Jantarat J, Palamara J, Messer H. An investigation of cuspal deformation and delayed recovery after occlusal loading. J Dent 2001;29:363–370.
2. Gonzalez-Lopez S, De Haro-Gasquet F, Vilchez-Dias MA, Ceballos L, Bravo M. Effect of restorative procedures and occlusal loading on cuspal deflection. Oper Dent 2006; 31:33-38. [ Links ]
3. Reeh ES, Messer HH, Douglas WH. Reduction in tooth stiffness as a result of endodontic and restorative procedures. J Endod 1989;15:512-516. [ Links ]
4. Shahrbaf S, Mirzakouchaki B, Oskoui SS, Kahnamoui MA. The effect of marginal ridge thickness on the resistance of endodontically-treated, composite restored maxillary premolars. Oper Dent 2007;32:285-290. [ Links ]
5. Bitter K, Meyer-Lueckel H, Fotiadis N, Blunck U, Neumann K, Kielbassa AM, Paris S. Influence of endodontic treatment, post insertion, and ceramic restoration on the fracture resistance of maxillary premolars. Int Endod J 2010;43:469-477. [ Links ]
6. Yamada Y, Tsubota Y, Fukushima S. Effect of restoration method on fracture resistance of endodontically treated maxillary premolars. Int J Prosthodont 2004;17:94-98. [ Links ]
7. Monga P, Sharma V, Kumar S. Comparison of fracture resistance of endodontically treated teeth using different coronal restorative materials: an in vitro study. J Conserv Dent 2009;12:154-159. [ Links ]
8. Reeves GW, Lentz DL, O'Hara JW, McDaniel MD, Tobert WE. Comparison of marginal adaptation between direct and indirect composites. Oper Dent 1992;17:210-214. [ Links ]
9. Dalpino PH, Francischone CE, Ishikiriama A, Franco EB. Fracture resistance of teeth directly and indirectly restored with composite resin and indirectly restored with ceramic materials. Am J Dent 2002;15:389-394. [ Links ]
10. Santos MJMC, Bezerra RB. Fracture resistance of maxillary premolars restored with direct and indirect adhesive techniques. J Can Dent Assoc 2005;71:585-585d. [ Links ]
11. Camacho GB, Goncalves M, Nonaka T, Osorio AB. Fracture strength of restored premolars. Am J Dent 2007;20:121-124. [ Links ]
12. Abo-Hamar SE, Hiller KA, Jung H, Federlin M, Friedl KH, Schmalz, G. Bond strength of a new universal self-adhesive resin luting cement to dentin and enamel. Clin Oral Investig 2005;9:161-167. [ Links ]
13. Burke FJT. Trends in indirect dentistry: 3. Luting materials. Dent Update 2005;32:257-260. [ Links ]
14. De Munck J, Vargas M, Van Landuyt K, Hikita K, Lambrechts P, Van Meerbeek B. Bonding of auto-adhesive luting material to enamel and dentin. Dent Mater 2004;20: 963-971. [ Links ]
15. Monticelli F, Osorio R, Mazzitelli C, Ferrari M, Toledano M. Limited decalcification/diffusion of self-adhesive cements into dentin. J Dent Res; 2008;87:974-979. [ Links ]
16. Vaz RR, Hipolito VD, D´Alpino PH, Goes MF. Bond strength and interfacial micromorphology of etch-and-rinse and self-adhesive resin cements to dentin. J Prosthodont 2012;21:101-111. [ Links ]
17. Goracci C, Cury AH, Cantoro A, Papacchini F, Tay FR, Ferrari M. Microtensile bond strength and interfacial properties of self-etching and self-adhesive resin cements used to lute composite onlays under different seating forces. J Adhes Dent 2006;8:327-335. [ Links ]
18. Al-Assaf K, Chakmakchi M, Palaghias G, Karanika-Kouma A, Eliades G. Interfacial characteristics of adhesive luting resins and composites with dentine. Dent Mater 2007;23: 829-839. [ Links ]
19. Hikita K, Van Meerbeek B, De Munck J, Ikeda T, Van Landuyt K, Maida T, Lambrechts P, Peumans M. Bonding effectiveness of adhesive luting agents to enamel and dentin. Dent Mater 2007;23:71-80. [ Links ]
20. Viotti RG, Kasaz A, Pena CE, Alexandre RS, Arrais CA, Reis AF. Microtensile bond strength of new self-adhesive luting agents and conventional multistep systems. J Prosthet Dent 2009;102:306-312. [ Links ]
21. Luhrs AK, Guhr S, Gunay H, Geurtsen W. Shear bond strength of self-adhesive resins compared to resin cements etch and rinse to enamel and dentin in vitro. Clin Oral Investig 2010;14:193-199. [ Links ]
22. De Angelis F, Minnoni A, Vitalone LM, Carluccio F, Vadini M, Paolantonio M, D'Arcangelo C. Bond strength evaluation of three self-adhesive luting systems used for cementing composite and porcelain. Oper Dent 2011;36: 626-634. [ Links ]
23. Cerutti A, Flocchini P, Madini L, Mangani F, Putignano A, Docchio F. Effects of bonded composite vs. amalgam on resistance to cuspal deflection for endodontically-treated premolar teeth. Am J Dent 2004;17:295-300. [ Links ]
24. Schwartz RS, Robbins JW. Post placement and restoration of endodontically treated teeth: a literature review. J Endod 2004;30:289-299. [ Links ]
25. Widmalm SE, Ericsson SG. Maximal bite force with centric and eccentric load. J Oral Rehabil 1982;9:445-450. [ Links ]
26. Tortopidis D, Lyons MF, Baxendale RH, Gilmour WH. The variability of bite force measurement between sessions, in different positions within the dental arch. J Oral Rehabil 1998;25:681-686. [ Links ]
27. Ausiello P, Apicella A, Davidson CL. Effect of adhesive layer properties on stress distribution in composite restorations – a 3D finite element analysis. Dent Mater 2002;18: 295-303.
28. Sakaguchi RL, Brust EW, Cross M, DeLong R, Douglas WH. Independent movement of cusps during occlusal loading. Dent Mater 1991;7:186-190. [ Links ]
29. Gwinnett AJ, Matsui A. A study of enamel adhesives. The physical relationship between enamel and adhesives. Arch Oral Biol 1967;12:1615-1619. [ Links ]
30. Nakabayashi N, Kojima M, Masuhara E. The promotion of adhesion by the infiltration of monomers into tooth substrate. J Biomed Mater Res 1982;16:265-273. [ Links ]
31. Gerth HUV, Dammaschke T, Zuchner H, Schafer E. Chemical analyses and bonding reaction of Relyx Unicem and Bifix composites – a comparative study. Dent Mater 2006; 22:934-941.
32. Stona P, Borges GA, Montes MA, Junior LH, Weber JB, Spohr AM. Effect of polyacrylic acid on the interface and bond strength of self-adhesive resin cements to dentin. J Adhes Dent 2013;15:221-227. [ Links ]
33. Duarte S Jr, Botta AC, Meire M, Sadan A. Microtensile bond strengths and scanning electron microscopic evaluation of self-adhesive and self-etch resin cements to intact and etched enamel. J Prosthet Dent 2008;100:203-210. [ Links ]
34. Pavan S, dos Santos PH, Berger S, Bedran-Russo AK. The effect of dentin pretreatment on the microtensile bond strength of self-adhesive resin cements. J Prosthet Dent 2010;104:258-264. [ Links ]
35. Zhang C, Degrange M. Shear bond strengths of self-adhesive luting resins fixing dentine to different restorative materials. J Biomater Sci Polym Ed 2010;21:593-596. [ Links ]
36. Anusavice KJ: Phillips - Dental Materials. Rio de Janeiro, Brazil: Guanabara, 1998:23-68. [ Links ]














