Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Acta Odontológica Latinoamericana
On-line version ISSN 1852-4834
Acta odontol. latinoam. vol.28 no.2 Buenos Aires Aug. 2015
ARTÍCULOS ORIGINALES
Correlation between gingival thickness and gingival recession in humans
Frederico B. Maroso1, Eduardo J. Gaio1, Cassiano K. Rösing1, Marilene I. Fernandes1
1 Department of Periodontology, Federal University of Rio Grande do Sul, Brazil
CORRESPONDENCE Dr.Marilene Issa Fernandes Rua Ramiro Barcelos, 2492 90035-003 - Porto Alegre RS, Brazil marileneissafernandes@gmail.com
ABSTRACT
Gingival recession is characterized by the apical migration of the gingival margin, exposing the root surface. Studies have demonstrated several etiological factors for gingival recession such as periodontitis, traumatic toothbrushing, use of oral piercing, and past orthodontic therapy, among others. It might not be possible to identify and quantify the influence of each factor, and gingival recession at some sites may be the result of the combination of these factors. Gingival recession affects individuals at all ages, with prevalence increasing as time passes. The aim of this study was to observe whether there is correlation between gingival thickness and gingival recession. Fifty-five subjects of both genders aged 18-35 years participated in the study. The volunteers were under treatment at the School of Dentistry of the Federal University of Rio Grande do Sul. Buccal gingival thickness was measured on incisors, canines and bicuspids, under anesthesia, following inclusion and exclusion criteria. Statistical analysis was performed with STATA version 10.1. The results had a Pearson Correlation Coefficient of -0.216. Linear regression had a statistically significant pvalue of 0.025. It may be concluded that there is weak negative correlation between gingival thickness and gingival recession.
Key words: Gingival recession; Gingival thickness.
RESUMO
Correlação entre espessura do tecido gengival e recessão gengival
A recessao gengival e caracterizada pelo deslocamento apical da margem gengival, expondo a superficie radicular. Pesquisas tem apresentado varios fatores relacionados a etiologia da recessao gengival como: periodontite, escovacao traumatica, uso de piercing oral, tratamento ortodontico passado, entre outros. Pode nao ser possivel identificar e quantificar a influencia de cada fator, e a recessao gengival, em determinados sitios, pode ser o resultado da confluencia de varias causas. A prevalencia da recessao gengival atinge individuos de todas as idades, aumentando significativamente com o passar dos anos. O objetivo do presente estudo foi observar se existe correlacao entre a espessura do tecido gengival e a recessao gengival. Participaram da pesquisa pacientes de ambos os generos, com idade entre 18 e 35 anos, que estavam em tratamento nas clinicas odontologicas da Faculdade de Odontologia da Universidade Federal do Rio Grande do Sul. Foram medidas a espessura e recessao gengival das faces vesti - bulares dos dentes incisivos, caninos e pre-molares, previamente anestesiados, seguindo os criterios estabelecidos para inclusao e exclusao no estudo. Para avaliacao e comparacao dos resultados foi utilizado o programa estatistico STATA versao 10.1. Os resulta - dos mostraram que a correlacao de Pearson entre a espessura gengival e a recessao foi de -0.216. A regressao linear apresentou um p= 0.025, estatisticamente significativo. Pode-se concluir que existe uma correlacao fraca e inversa entre espessura gengival e recessao gengival.
Palavras-chave: Recessao gengival; Espessura gengival.
INTRODUCTION
Gingival recession is characterized by the apical relocation of the gingival margin, exposing the root surface. Multiple factors are involved in its etiology, including anatomical, physiological, pathological and traumatic factors which probably do not act simultaneously or to the same degree,1 and it is probably impossible to identify which the most important factor is. The development of gingival recession seems to be associated to inflammatory processes of different origins2.
The occurrence of gingival recession varies widely, from 3 to 100%, depending of the population, diagnostic criteria and methods of analysis3. A study on a representative sample of subjects in a city in Brazil showed that the prevalence of gingival recession increases with age. The prevalence of at least one site with gingival recession ≥ 1 mm is 29.5% in youths aged 14-19 years and 99% in adults older than 40 years4. In France, it was demonstrated that 84.6% of individuals present at least one site with gingival recession5. Gingival thickness seems to be an important risk and prognostic factor for the occurrence of future gingival recession6. Studies have shown that the gingival biotype is also a determinant of esthetic results in different therapies7. A thick gingival unit is associated with better results, especially concerning the stability of the gingival margin over time. However, most studies do not look at gingival thickness, particularly in healthy individuals. The aim of this study was thus to correlate gingival thickness and gingival recession in adults without history of periodontitis.
MATERIALS AND METHODS
A convenience sample of fifty-five adults (24 male and 31 female) aged 18-35 years participated in this cross-sectional study. Mean age (}SD) was 24.82 5.17. The study included non-smokers, without history of periodontitis, under treatment at the School of Dentistry of the Federal University of Rio Grande do Sul, Brazil. Diabetic patients, pregnant and lactating women, individuals under orthodontic therapy, with history of periodontal surgery, presenting cervical restorations or under medication affecting the periodontium such as cyclosporin A, calcium channel blockers and phenytoin were not included. The research protocol was approved by the Institutional Review Board and all participants signed an informed consent form. The study followed the guidelines of the Declaration of Helsinki.
Sample size estimation
In order to estimate the sample size, data from the prevalence of gingival recession in the metropolitan area of Porto Alegre in the same age range were used4. Considering a prevalence of gingival recession higher than 70%, alpha and beta errors of 5 and 10%, it was determined that 43 individuals were necessary for the study. Twenty percent oversampling was used.
Clinical examination
Clinical periodontal parameters and gingival thickness were evaluated in upper or lower teeth (15- 25 or 35-45) previously anesthetized for dental treatment. A previously trained examiner performed all clinical measurements. The following parameters were evaluated:
a) Visible Plaque Index (VPI)8: absence or presence of visible plaque after drying was scored.
b) Gingival Bleeding Index (GBI)8: absence or presence of gingival bleeding was scored after gentle probing of the gingival margin.
c) Gingival Recession (GR): the distance from the cemento-enamel junction (CEJ) to the gingival margin was measured in millimeters and rounded to the nearest millimeter. When the CEJ was not clinically visible, the measurement was given a negative sign.
d) Probing Depth (PD): the distance between the gingival margin and the most apical probeable part of the crevice was measured in millimeters and rounded to the nearest millimeter. A Williams periodontal probe was used.
e) Bleeding on Probing (BoP): absence or presence of bleeding after probing the bottom of the crevice up to 30 seconds after probing was recorded.
f) Clinical Attachment Level (CAL): obtained by adding PD and GR.
Measurement of gingival thickness
Gingival thickness (GT) was evaluated by piercing with a needle with a rubber stent perpendicular to the root surface at the mid-point between the gingival margin and the muco-gingival junction. The stent was pressed until it touched the gingival surface. After removing the needle, the distance from the end of the needle to the stent was measured with a digital caliper. All measurements were performed by the same examiner9.
Reliability
Before the study began, the examiner was trained and calibrated for the GW measurements by measuring 5 individuals twice, with a 40-minute interval. The Intraclass Correlation Coefficient (ICC) was 0.98. During the study, trans-experimental reliability was tested in 5 patients, with the same methodology, and the ICC was 0.99.
Statistical analysis
Data analysis comprised descriptive and analytical approaches. Outcome values of all continuous parameters are shown as mean and standard devia - tion (SD). Correlations between gingival thickness and gingival recession were calculated using the Pearson correlation coefficient with the corresponding 95% confidence intervalthickness. After analysis of data distribution, linear regression models were analyzed (STATA 10.1 for Macintosh).
RESULTS
Full mouth periodontal clinical conditions of the individuals included in the study are shown in Table 1. Participants had good standards of oral health, with an average of 29.18 existing teeth. Plaque control showed values of visible plaque, gingival bleeding and bleeding on probing of approximately 15-20%. It was observed that 11.5% of existing teeth exhibited some degree of loss of attachment. Table 2 shows periodontal clinical parameters at sites where gingival thickness was measured. At these sites, mean probing depth was 1.2 mm (range 0.95 - 3.00 mm). Gingival recession had a mean value of 1.01mm (range 0 - 3.5mm). Mean gingival thickness varied from 1 to 1.97mm, with a mean of 1.40mm.
Table 1: Full mouth periodontal clinical variables of the subjects.
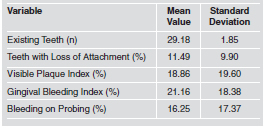
Table 2: Clinical periodontal parameters at sites where gingival thickness was measured.
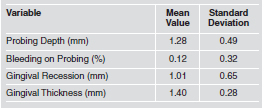
Fig. 1 is the main outcome of the present study and demonstrates the correlation between gingival thickness and gingival recession: the smaller the gingival thickness, the greater the gingival recession. The Pearson correlation coefficient was -0.22. The simple linear regression model demonstrates a statistically significant relationship (p= 0.02).

Fig. 1: Correlation between gingival thickness and gingival recession.
DISCUSSION
This study evaluated possible association between gingival thickness and gingival recession, finding a statistically significant correlation between them. These results should be interpreted in the light of the literature and taking into account the strengths and limitations of the study. This is a cross-sectional study, therefore causality cannot be claimed. However, a series of method - ological principles were taken into consideration in order to increase the validity of the results. The study comprises a sample of young adults aged 18- 35 years. The restriction to a specific age range relates to the fact that it has been demonstrated that the prevalence, extent and severity of gingival recession increase with age.10,11 Susin et al.4 demonstrated, in the same area where our study was performed, that in individuals 20-29 years old, 18% of teeth had gingival recession ≥ 1 mm. In our study, the mean extension of gingival recession was 13.6 teeth (range 6-26). Individuals with previous exposure to periodontitis were excluded in order to focus attention on recession unrelated to periodontal disease. However, this potential confounder cannot be ruled out. On the other hand, even in individuals with loss of attachment due to periodontal disease, whether or not gingival recession occurred could have the gingival biotype as a predisposing factor.9
Studies demonstrate that the presence of oral biofilms and periodontal breakdown are associated with gingival recession. In this study, approximately 18% of the examined surfaces without recession presented visible plaque, sites with gingival recession did not present visible plaque. Moreover, it should be noted that examined sites presented less bleeding on probing than full mouth scores (16.25 vs. 0.12%). Virtually no inflammation was observed at examined sites, suggesting that traumatic brushing could be part of the causal chain. Additionally, this study did not include smokers, in order to reduce the potential confounder, since smoking has been strongly associated with higher degrees of loss of periodontal attachment4. Severity of gingival recession in this study was relatively low, with a range of 0-3.5mm and mean value 1.01mm. This finding is in accordance with the study by Susin et al.4, where higher degrees of recession affected a very small proportion of individuals younger than 40 years of age. This study restricted the examination to non-molars because anterior teeth tend to present higher degrees of gingival recession2,3,4. In addition, it is easier to measure gingival thicknessthickness on them, increasing the chances of higher reliability. Moreover, the sample size was estimated in order to ensure that the number of individuals included would be sufficient for drawing conclusions. It should be noted that gingival recession is not an unavoidable physiological process due to aging, but may be explained by the cumulative effects of trauma and/or inflammation of the periodontium3,4. In this context, gingival thickness could play a role that should not be ruled out.
Vandana and Savitha12 demonstrated that gingival thickness varies according to age, gender and dental arch. Younger individuals, men and upper jaws tend to present thicker gingiva. This would suggest a separate analysis for these factors. However, in this age range it was not possible to demonstrate differences in these aspects, therefore a combined analysis was performed4. Mean gingival thickness in our study was 1.40 mm, similar to that in the literature.12 In the study by Vandana and Savitha12, for example, mean gingival thickness was 1.63 - 1.73mm (1.59-1.78mm in 16- to 24-year-olds and 0.93-1.07mm in 25- to 38-year olds). thicknessThey suggest that alterations in the oral epithelium caused by aging may thin the epithelium and diminish keratinization. Gingival thickness may be measured by invasive and non-invasive methods, but there are few studies comparing them. Savitha and Vandana13 demonstrated that trans-gingival probing and ultrasound are both reliable. In our study, reliability was ensured by double measurements with an excellent intra-class correlation coefficient both prior to and during the experiment. Gingival recession as a multifactorial entity has been extensively studied. Among possible etiological/ predisposing factors, the amount of keratinized gingiva has been suggested. However, studies failed to demonstrate causality in this respect.14 Evidence suggests that even in the absence of keratinized gingiva, gingival recession is not a natural consequence.14
On the other hand, studies that associate gingival recession with gingival thickness are few and controversial. Our study found that the lower the gingival thickness, the higher the degree of gingival recession. However, due to data dispersion, a low Pearson Correlation Coefficient was observed among these variables. On the other hand, the statistically significant correlation suggests a consistent association. The regression line demonstrated a statistically significant p-value (0.025). This means that even though the correlation could be interpreted as low, a negative linear relationship exists among gingival recession and gingival thickness. The limitations of our study should be taken into consideration in the conclusion process. These limitations include the fact that the study was crosssectional and restricted to young adults. However, it is within the age range of our subjects that preventive strategies could be implemented. Follow-ups of cohorts starting early in adolescence could be an interesting way of overcoming these limitations. In conclusion, gingival thickness is inversely correlated to gingival recession in young adults with lower degrees of gingival inflammation.
1. Smith RG. Gingival recession. Reappraisal of an enigmatic condition and a new index for monitoring. J Clin Periodontol 1997; 24:201-205. [ Links ]
2. Toker H, Ozdemir H. Gingival recession: epidemiology and risk indicators in a university dental hospital in Turkey. Int J Dent Hyg 2009; 7:115-120. [ Links ]
3. Litonjua LA, Andreana S, Bush PJ, Tobias TS et al. Wedged cervical lesions produced by toothbrushing. Am J Dent 2004;17:237-240. [ Links ]
4. Susin C, Haas AN, Oppermann RV, Haugejorden O et al.. Gingival recession: epidemiology and risk indicators in a representative urban Brazilian population. J Periodontol 2004;75:1377-1386. [ Links ]
5. Sarfati A, Bourgeois D, Katsahian S, Mora F et al. Risk assessment for buccal gingival recession defects in an adult population. J Periodontol 2010;81:1419-1425. [ Links ]
6. Nguyen-Hieu T, Ha Thi BD, Do Thu H, Tran Giao H. Gingival recession associated with predisposing factors in young vietnamese: a pilot study. Oral Health Dent Manag 2012;11:134-44. [ Links ]
7. Goldberg PV, Higginbottom FL, Wilson TG. Periodontal considerations in restorative and implant therapy. Periodontol 2000 2001;25:100-109. [ Links ]
8. Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J 1975;25:229-235. [ Links ]
9. Olsson M, Lindhe J, Marinello CP. On the relationship between crown form and clinical features of the gingiva in adolescents. J Clin Periodontol 1993; 20:570-577. [ Links ]
10. Marini MG, Greghi SL, Passanezi E, Sant'ana AC. Gingival recession: prevalence, extension and severity in adults. J Appl Oral Sci 2004;12:250-255. [ Links ]
11. Chang LC. Comparison of age and sex regarding gingival and papillary recession. Int J Periodontics Restorative Dent 2012;32:555-561. [ Links ]
12. Vandana KL, Savitha B. Thickness of gingiva in association with age, gender and dental arch location. J Clin Periodontol 2005;32:828-830. [ Links ]
13. Savitha B, Vandana KL. Comparative assesment of gingival thickness using transgingival probing and ultrasonographic method. Indian J Dent Res 2005;16:135-139. [ Links ]
14. Closs LQ, Branco P, Rizzatto SD, Raveli DB, Rosing CK. Gingival margin alterations and the pre-orthodontic treatment amount of keratinized gingiva. Braz Oral Res 2007;21:58-63. [ Links ]














