Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Acta Odontológica Latinoamericana
versión On-line ISSN 1852-4834
Acta odontol. latinoam. vol.29 no.2 Buenos Aires set. 2016
ARTÍCULOS ORIGINALES
Lower incisor inclination regarding different reference planes
Brenda Zataráin, Josué Avila, Angeles Moyaho, Rosendo Carrasco, Carmen Velasco
Department of Orthodontics, School of Dentistry, Meritorious Autonomous University of Puebla, Mexico.
CORRESPONDENCE Dr. Angeles Moyaho 31 Poniente Núm. 1304 col. Volcanes. Puebla, Pue. México moyaho3@gmail.com
ABSTRACT
The purpose of this study was to assess the degree of lower incisor inclination with respect to different reference planes. It was an observational, analytical, longitudinal, prospective study conducted on 100 lateral cephalograms which were corrected according to the photograph in natural head position in order to draw the true vertical plane (TVP). The incisor mandibular plane angle (IMPA) was compensated to eliminate the variation of the mandibular plane growth type with the formula “FMApx.– 25 (FMA) + IMPApx. = compensated IMPA (IMPACOM)”. As the data followed normal distribution determined by the KolmogorovSmirnov test, parametric tests were used for the statistical analysis, Ttest, ANOVA and Pearson coefficient correlation test. Statistical analysis was performed using a statistical significance of p <0.05. There is correlation between TVP and NB line (NB) (0.8614), Frankfort mandibular incisor angle (FMIA) (0.8894), IMPA (0.6351), Apo line (Apo) (0.609), IMPACOM (0.8895) and McHorris angle (MH) (0.7769). ANOVA showed statistically significant differences between the means for the 7 variables with 95% confidence level, P=0.0001. The multiple range test showed no significant difference among means: APoNB (0.88), IMPAMH (0.36), IMPANB (0.65), FMIAIMPACOM (0.01), FMIATVP (0.18), TVPIMPACOM (0.17). There was correlation among all reference planes. There were statistically significant differences among the means of the planes measured, except for IMPACOM, FMIA and TVP. The IMPA differed significantly from the IMPACOM. The compensated IMPA and the FMIA did not differ significantly from the TVP. The true horizontal plane was mismatched with Frankfort plane in 84% of the sample with a range of 19°. The true vertical plane is adequate for measuring lower incisor inclination.
Key words: Orthodontics; Incisor; Reference standards.
RESUMEN
Inclinación del incisivo inferior respecto a diferentes planos de referencia
El propósito del estudio fue concordar el grado de inclinación del incisivo inferior medido con los diferentes planos de referencia. Estudio observacional, analítico, longitudinal y prospectivo en 100 radiografías laterales que fueron corregidas con base en la fotografía en posición natural de la cabeza, para trazar el plano vertical verdadero (PVV). Se compensó el ángulo del plano incisivo mandibular (IMPA) para eliminar la variación del plano mandibular respecto al tipo de crecimiento con la fórmula “FMApx. – 25 (FMA) + IMPApx. = IMPA compensado (IMPACOM)”. Los datos tuvieron una distribución normal de acuerdo a la prueba KolmogorovSmirnov, por lo tanto se aplicaron pruebas paramétricas, T para medias de una muestra, coeficiente R de Pearson y ANOVA. El análisis estadístico fue realizado con una significancia estadística de p<0.05. Existe correlación entre el PVV con la línea NB (NB) (0.8614), ángulo de Frankfort incisivo mandibular (FMIA) (0.8894), IMPA (0.6351), línea Apo (APo) (0.609), IMPACOM (0.8895) y ángulo de McHorris (MH) (0.7769). De acuerdo al análisis de ANOVA existen diferencias estadísticamente significativas entre las medias de las 7 variables con un nivel de 95% de confianza p=0.0001. Mediante la prueba de múltiples rangos para determinar diferencias entre medias, se demostró que no existen diferencias significativas entre: APoNB (0.88), IMPAMH (0.36), IMPANB (0.65), FMIAIMPACOM (0.01), FMIAPVV (0.18), PVVIMPACOM (0.17). Todos los planos de referencia presentaron correlación entre ellos. Las mediciones derivadas de éstos tuvieron diferencias estadísticamente significativas, a excepción de FMIA, IMPACOM Y PVV. Existen diferencias estadísticamente significativas entre el ángulo IMPA y éste con su compensación. No se encontraron diferencias significativas entre el IMPACOM y PVV. El plano de Frankfort y el PHV no son coincidentes en un 84%, con un rango de 19 grados.
Palabras clave: Ortodoncia; Incisivo; Estándares de referencia.
INTRODUCTION
In orthodontics, the position of the lower incisor is considered essential to reaching an appropriate diagnosis and designing a treatment plan. It even defines certain aspects such as whether extractions are needed and what type of anchorage should be used.13 Lower incisor position has a significant functional effect. It must resist incisal overeruption and provide harmony and functionality to the temporomandibular joint, providing an appropriate anterior guide and protrusive movements, which are crucial to mutually protected organic occlusion.4 It also affects stability, because when the incisors are within the cortical bone, rather than outside it or at the biological limit, there is less risk of relapse.5 Tweed advocated placing the mandibular incisors upright to achieve balance and harmony in the lower facial third6 Angle held that lower lip curvature is determined by incisor position7, and many authors have emphasized that the effect of lower incisor position is crucial to dental and facial aesthetics.8,10 Lower incisor position was formerly considered so important that the course of the treatment plan was based only on its initial and final position, considered the key to successful treatment.8,13 Although it is currently known that a correct diagnosis must consider multiple factors in addition to the lower incisor, there is no doubt regarding its major effect in terms of function, stability and aesthetics. 13, 9, 14
It is important to assess the position of the lower incisor not only on all three planes of space in relation to the mandibular alveolar bone and chin, but also in relation to the vertical and horizontal composition of the face.15 Unlike the vertical and transversal plane, the anteroposterior plane has a very restricted field anatomically, therefore, in order to achieve optimal incisor position, it is important to assess its angulation. Excessive inclination can cause recession of the gingival margin or bone dehiscence, and insufficient angulation can cause fenestration.16,18 The lower incisor has thus been the object of much attention for many years. Many authors have tried to establish an optimal position, taking as reference different planes involving both hard and soft tissues. With the implementation of radiography in the dental field, several cephalometric analyses have emerged. They have been extraordinarily useful to diagnostic procedures by enabling accurate assessments of skeletal and dental relationships occurring in different types of malocclusion.19 For cephalometric study, the vertical and horizontal true planes have also been implemented, which are obtained from the Natural Head Position (NHP).20,23
There are currently multiple reference planes to measure incisor angulation; however, they are all affected by the other anatomical structures of each patient, so that their interpretation is highly variable. The bases of all cephalometric analysis were pro posed years ago, and despite further contributions from different studies, current research establishes that a valid cephalometric reference should include the following features: reliability, intraindividual reproducibility, low interindividual variability and average orientation close to the vertical or horizontal true plane.
Downs related incisor inclination to its upper antagonist, the mandibular plane and the occlusal plane. In addition to the use of the Frankfort mandibular plane, he introduced the APo line as a reference. However, unlike Tweed, he highlighted the importance of positioning the incisors in relation to the occlusal plane, and not necessarily in relation to the mandibular plane.27,29 Schudy confirmed this and reported that the lower incisor is more consistently related to the occlusal than the mandibular plane in all types of facial morphology30. Knosel et al. found that third order angulation of fixed orthodontic appliances dictates incisal inclination, which refers to a perpendicular to the occlusal plane, and incisor inclination presents no correlation with craniofacial cephalometric measurements. 31, 32 Steiner’s cephalometric analysis associated the lower incisor to the middle facial third, and suggested individualizing the position of the lower incisor according to the relative prominence of the chin and the patient’s maxillarymandibular discrepancy. To this end, he proposed the line NB, formed by the union of Nasion and point B, as a reference.33
Tweed reaffirmed the standards of the proposed angles in his diagnostic triangle, and took the FMA angle variation (formed by the mandibular plane and the Frankfort horizontal plane) from 16 to 35 degrees with a standard value of 25; the IMPA angle (lower incisor with respect to mandibular plane) from 8085 with norm of 90, and the FMIA angle (lower incisor with regard to Frankfort Horizontal plane) ideally as 65, though in rare cases it requires 75 degrees to achieve better facial balance.34,35 An important consideration when applying these measurements is the compensation that IMPA requires with regard to FMA. As the inclination of the mandibular plane with regard to Frankfort plane increases or decreases, the measure of lower incisor with respect to the mandibular plane will also vary but in the opposite direction. In other words, for each degree by which the FMA exceeds the norm of 25°, the mandibular incisors must be positioned a lower number of the norm of 90°, and vice versa, in case of a decrease of FMA, the mandibular incisors must be positioned a higher number of the IMPA’s norm of 90°.35 Another outstanding author, Ricketts, established that the APo line represents a relationship of bony bases which can be affected by movements of the lower incisor, the APo line itself, or both, which should be considered when estimating the direction and degrees of desired movement in order to functionally place anterior teeth. His norm of incisal inclination differs from Downs’, which is 21sup5 degrees. 36,38 McHorris proposed using the CI angle, formed by the radius of the mandibular hinge axis and the longitudinal axis of the lower incisor, at the intersection with the incisal edge of the latter. He acknowledged that the CI line was not affected by the mandibular position relative to the maxilla or the cranial base. He also pointed out the importance of condylar position in harmony with the teeth, because since they are at the service of the condyles in both static and dynamic relationship, there is more harmonious occlusion.39, 40. In 1950 there was an important introduction: the natural head position, defined as an innate, physiological, reproducible head position, obtained when the patient is relaxed, sitting or standing, with the horizontal visual axis at eye level. It is known as the selfbalance position of the head or natural orientation.41 Also, this position offers the advantage of the cephalometric evaluation being based on the same standards as the clinical evaluation.20,23,42
It is difficult to define a reference plane to set the ideal position of the lower incisor because there are multiple factors that affect and modify it. In addition, cephalometric analyses were obtained from dentures considered ideal, with the confluence of skeletal and dental features that usually do not occur in malocclusions, therefore they have been the subject of criticism and disagreement in the orthodontic field.43
The aim of this study was to match the degree of inclination of the lower incisor measured with different reference planes under the hypothesis that there is agreement among them. The reference planes considered were: (1) the Frankfort horizontal plane (FH) (which gives rise to FMIA angle), (2) the Nasion Point B line (NB), (3) the Point APogonion line (APo), (4) the mandibular plane (PM), (which gives rise to IMPA angle), (5) the McHorris plane (MH), and (6) the true vertical plane (TVP).
MATERIAL AND METHODS
Prior authorization was obtained from the Division of Postgraduate Studies of the School of Dentistry of the Meritorious Autonomous University of Puebla (FEBUAP) for the biological and method ological requirements. An observational, analytic, longitudinal, prospective study was conducted. Using a nonprobabilistic convenience sample, 100 lateral cephalograms were analyzed from patients who visited the orthodontic clinic in 2014 and met the selection criteria. Selection criteria were: fully erupted dentition up to first molar; with initial panoramic and cephalogram radiographs with sufficient sharpness to identify the lower incisors and other anatomical structures that are part of the reference planes; without previous orthodontic or orthopedic treatment; without supernumerary teeth, prosthetic dentures or missing teeth, and without craniofacial deformities or syndromes. A profile photograph of the patients in lateral head position (NHP) was taken in order to draw a true vertical and the radiograph was corrected based on this photograph. The lower incisor was measured taking as reference the NB, APo, IMPA, FMIA, TVP and McHorris plane. The FMA angle (Frankfort plane and mandibular plane) was also measured, to establish the patient’s mandibular growth type.
To standardize the researchers, 10 radiographs were taken randomly and retraced two weeks later to avoid memory bias. The measurements were compared to those from the first trace and Pearson’s R coefficient test was performed to determine measurement error. No statistically significant difference was found between the two measurements. Subsequently, all radiographs were measured using cephalometric paper, 0.05mm pencil and an Ormco brand protractor. IMPA compensation was performed as described by Tweed34,35 with the formula proposed by the researchers (Fig 1). Statistical analysis was conducted using SPSS version 20 and STATGRAPHICS Centurion XVI.II, with a statistical significance of p< 0.05. The data had normal distribution, which was determined with the KolmogorovSmirnov test, therefore parametric tests were applied, T test for sample means, Pearson’s R coefficient and ANOVA.
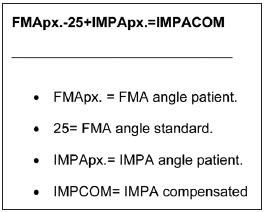
Fig. 1: Formula to compensate the IMPA.
RESULTS
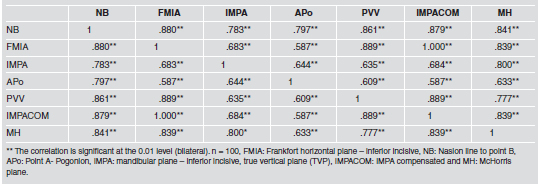
A total 100 lateral cephalograms were included. Pearson’s R coefficient test showed correlation between lower incisor inclination and all planes studied, including the true vertical plane (Table 1).
Table 1.
Comparison of the 7 variables with ANOVA showed statistically significant differences between means with a 95% level of confidence p=0.0001 (Table 2). A multiple range test was used to determine in which groups these differences are significant. It is important to mention that there were no differences between the TVP, IMPACOM and FMIA (Table 3). The StudentT test for means was applied to determine the differences between the means of the studied planes and the TVV, finding no statistically significant difference between the TVP and the FMIA and IMPACOM planes (Table 4). Finally, StudentT test for means comparing IMPA to IMPACOM found statistically significant differences with p<0.0001 (Table 5). The Frankfort plane matches the Horizontal True only in 16% of the cases, and the measurements obtained vary between 8 and 11 (Fig 2).
Table 2.
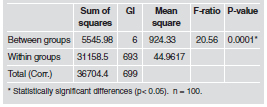
Table 3.
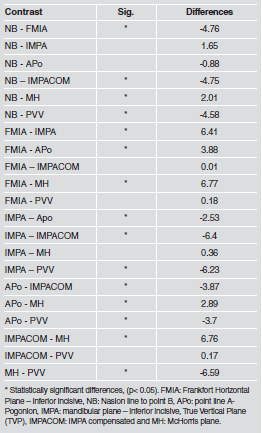
Table 4.
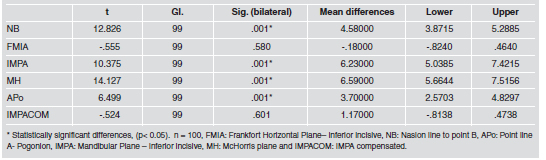
Table 5.
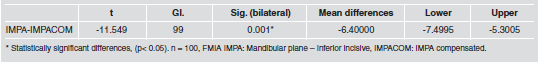
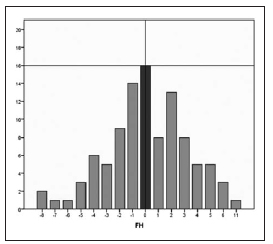
Fig. 2: The Frankfort plane matches the Horizontal True correlation.
DISCUSSION
With the development of orthodontic science, diagnostic accuracy and treatment plan detail have both increased, resulting in the need to evaluate the methods used. In order to apply cephalometric measurements properly, it is important to determine their specificity and sensitivity with regard to the position of teeth and their bony bases, and the relationship between them, the jaws and other cranial structures. If cephalometric measurements are interpreted inappropriately, they can lead in the wrong direction.44
Similarly, the literature has emphasized the impor tance of timely, accurate diagnosis of the lower incisor by analyzing its position and inclination, as well as of other structures that influence and affect its measurement.24, 27, 29, 34,38 This information influences decisions for the treatment plan, such as whether extractions or stripping will be performed and what anchorage type and biomechanics will be used, among other aspects. 13 It is also relevant in presurgical orthodontics because the measurements used are often based on surgically repositioned structures. Cephalometric analysis should therefore be objective and consider each factor that may change or influence the measurement result.44 Based on the reference planes used in the present study, the lower incisor had an average proclination of 4.8°, lower than reported by Gutermann16 (6.6°) and Asad45 (7.7°), in similar samples. However, the variations among the means obtained for each plane were considerable, with the McHorris and FMIA angles indicating the lowest and highest procli nation, respectively (1.2° sup 7 y 8°sup 6). This shows how altered incisor measurement can depend on the reference plane used.44
There was correlation among all the reference planes analyzed. Aldreeset al.46 reported similar results in terms of correlation between the mandibular plane and NB line, contrary to what was reported by Linder and Cornelius.47 The weakest correlation was observed for the APo line with regard to other planes, including FMIA (.587), IMPA (.644) and TVP (.609). Another low correlation was for IMPA with regard to FMIA (.683) and TVP (.644). This is due to the great influence of the horizontal and vertical position of the jaw on the APo line38,44 and IMPA angle, highlighting the need for appropriate compensation in the latter in order to eliminate this variability factor.34, 35 The FMIA angle derives from the Frankfort plane, and is therefore strongly influenced by it. Ideally, the position of the Frankfort plane should be as close as possible to a true horizontal, however, in the present study this only occurred in 16% of the samples, with a minimum value of 8°, maximum of 11° and a broad range of 19°, similar to values reported by Madsen20 and Shetty21, at 23° and 16°, respectively. The low correlation between FMIA and the other planes and its large difference with measurements of other groups is due to the fact that it is also affected by the position and rotation of the mandible, as stated by Williams48,49 (1969, 1985). The IMPA measurement was compensated following Tweed (1952, 1964), to remove the variation of the vertical and horizontal position of the jaw. The following formula is proposed:
FMApx – 25 + IMPApx = compensated IMPA
i.e., for each degree by which the FMA angle exceeds the norm of 25°, the mandibular incisors must be positioned a lower number of the IMPA’s norm of 90°, and vice versa, in case of a decrease in FMA, the mandibular incisors must be positioned a higher number of the IMPA’s norm of 90°.34, 35 The true vertical plane has not been used previously to measure lower incisor inclination. However, in the sample analyzed in our study, the true vertical plane showed correlation with the other reference planes, and measurements of incisal inclination did not differ significantly from the FMIA angle and IMPACOM. The planes with greatest differences in the proclination or retroclination degrees were the McHorris plane with regard to TVP (6.59) and FMIA (6.77), and the IMPA angle with regard to TVP (6.23), FMIA (6.41) and IMPACOM (6.4). It is thus feasible to state that the most consistent measurements are derived from the true vertical planes, FMIA and IMPA with its compensation, since without it the differences are heightened considerably.
CONCLUSION
There was correlation among all reference planes. The differences were statistically significant except for FMIA, IMPACOM and TVP. There were statistically significant differences between the IMPA angle and the compensated angle. No significant difference was found between the IMPACOM and the incisive measurement derived from the TVP. The Frankfort horizontal plane and the true horizontal plane are mismatched in 84% of the sample population, with a range of 19°.
1. Richmond S, Klufas ML, Sywanyk M. Assessing incisor inclination: a noninvasive technique. Eur J Orthod 1998; 20: 721-726. [ Links ]
2. Allais D, Melsen B. Does labial movement of lower incisors influence the level of the gingival margin? A case–control study of adult orthodontic patients. Eur J Orthod 2003; 25: 343-352.
3. Hernandez Sayago E, Espinar Escalona E, Barrera Mora JM, Ruiz Navarro MB, Llamas Carreras JM, Solano Reina E. Lower incisor position in different malocclusions and facial patterns. Medicina Oral S. L 2013; 18: 343-50. [ Links ]
4. Andrews LF. The diagnostic system: Occlusal analysis. Dent. Clin. North Am 1976; 20: 671-690. [ Links ]
5. Profit WR. Equilibrium theory revisited: factors influencing position of the teeth. Angle Orthod 1978; 48: 175-186. [ Links ]
6. Klontz HA. Facial balance and harmony: An attainable objective for the patient with a high mandibular plane angle. Am J Orthod Dentofacial Orthop 1998; 114: 176-188. [ Links ]
7. Schullhof RJ, Allen RW, Walters RD, Dreskin M. The mandibular dental arch: Part I, lower incisor position. Angle Orthod 1977; 47: 280-287. [ Links ]
8. Margolis HI. Axial inclination of mandibular incisors. Am J Orthod 1943; 29: 571-594. [ Links ]
9. Wylie WL. The mandibular incisor—its role in facial esthetics. Angle Orthod 1955; 25: 32-41.
10. Hezberg. BL. Facial esthetics in relation to Orthodontic treatment. Angle Orthod 1952; 22: 3-22 URL: http://www.angle.org/doi/pdf/10.1043/00033219(1952)022%3C0003:FEIRTO%3E2.0.CO%3B2 [ Links ]
11. Tweed, CH. The application of the principles of the edgewise arch in the treatment of malocclusions: II. Angle Orthod 1941; 11: 12-67. [ Links ]
12. Williams P. Lower incisor position in treatment planning. Br J Orthod 1986; 13: 3341. [ Links ]
13. Metzdorf, DW. A cephalometric study of cranial, mandibular and lower incisor morphology in the adult face. Angle Orthod 1977; 47: 288-292. [ Links ]
14. Ceylan I, Baydas B, Bolukbasi B. Longitudinal cephalo metric changes in incisor position, overjet, and overbite between 10 and 14 years of age. Angle Orthod 2002; 72: 246-250. [ Links ]
15. Hasund A, Boe O. Floating norms as guidance for the position of the lower incisors. Angle Orthod 1980; 50:165-168. [ Links ]
16. Gutermann C, Peltomaki T, Markic G, Hanggi M, Schatzle M, Signorelli L, Patcas R. The inclination of mandibular incisors revisited. Angle Orthod 2014; 84:109-119. [ Links ]
17. Yared KF, Zenobio EG, Pacheco W. Periodontal status of mandibular central incisors after orthodontic proclination in adults. Am J Orthod Dentofacial Orthop 2006; 130: 18. [ Links ]
18. Dorfman HS. Mucogingival changes resulting from mandibular incisor tooth movement. Am J Orthod 1978; 74: 286-297. [ Links ]
19. Kuramae M, Borges M, Nouer D, Bovi G, Inoue R. Analysis of Tweed’s facial triangle in black Brazilian youngsters with normal occlusion. Braz J Oral Sci 2004; 3:401-403.
20. Madsen D, Sampson W, Townsend G. Craniofacial reference plane variation and natural head position. Eur J Orthod 2008; 30: 532-540. [ Links ]
21. Shetty D, Bagga DK, Goyal S, Sharma P. A cephalometric study of various horizontal reference planes in natural head position. J Ind Orthod Soc 2013; 47: 143-147. [ Links ]
22. El Hayeck E, Bou Assi S, Bou Serhal J. Clinical study of orientation and reference planes in cephalometry. Orthod Fr 2005; 76: 217-227. [ Links ]
23. Foster TD, Howat AP, Naish PJ. Variation in cephalometric reference lines. Br J Orthod 1981; 8: 183-187. [ Links ]
24. Tweed CH. The Frankfortmadibular plane Angle in orthodontic diagnosis, Classification, Treatment Planning and Prognosis. Am J Orthod and Oral Surg 1946; 32: 175-221. [ Links ]
25. Riedel RA. Esthetics and its relation to orthodontic therapy. Angle Orthod 1950; 20: 168-178. [ Links ]
26. Ellis E 3rd, McNamara J Jr. Cephalometric reference planessella nasion vs Frankfort. Int J Adult Orthod Orthognath Surg 1988; 3: 81-87. [ Links ]
27. Downs WB. Variations in facial relationships: Their significance in treatment and prognosis. Am J Orthod 1948; 34: 812-840. [ Links ]
28. Downs WB. The role of cephalometrics in orthodontic case analysis and diagnosis. Am J Orthod 1952; 38: 162-182. [ Links ]
29. Downs WB. Analysis of the Dentofacial Profile. Angle Orthod 1956; 26: 191-212. [ Links ]
30. Schudy F. Cant of the occlusal Plane and Axial Inclinations of Teeth. Angle Orthod 1963; 33: 69-82. [ Links ]
31. Knosel M, Engelke W, Attin R, Kubein Meesenburg D, Sadat Khonsari R, Gripp Rudolph L. A method for defining targets in contemporary incisor inclination correction. Eur J Orthod 2008; 30: 374-380. [ Links ]
32. Knosel M, Attin R, Kubein Meesenburg D, Sadat Khonsari R. Cephalometric assessment of the axial inclination of upper and lower incisors in relation to the thirdorder angle. J Orofac Orthop 2007; 68: 199-209. [ Links ]
33. Steiner CC. Cephalometrics for you and me. Am J Orthod 1953; 39: 729-755. [ Links ]
34. Tweed CH. The Frankfort Mandibular Incisor Angle (FMIA) In Orthodontic Diagnosis, Treatment Planning and Prognosis. Angle Orthod 1954; 24: 121-169. URL: http://www.angle.org/doi/pdf/10.1043/00033219%281954%29024%3C0121%3ATFIAFI%3E2.0.CO%3B2 [ Links ]
35. Tweed CH. Was the development of the diagnostic facial triangle as an accurate analysis based on fact or fancy? Am J Orthod 1962; 48: 823-840. [ Links ]
36. Ricketts RM. Cephalometric Analysis and Synthesis. Angle Orthod 1961; 31: 141-156. [ Links ]
37. Ricketts RM. Planning treatment on the basis of the facial pattern and an estimate of its growth. Angle Orthod 1957; 27: 14-37. [ Links ]
38. Ricketts RM. Perspectives in the clinical application of cephalometrics. Angle Orthod 1981; 51: 115-150. [ Links ]
39. McHorris WH. Occlusion with particular emphasis on the functional and parafunctional role of anterior teethpart 1. J Clin Orthod 1979; 13: 606-620. [ Links ]
40. McHorris WH. Occlusion with particular emphasis on the functional and parafunctional role of anterior teethpart 2. J Clin Orthod 1979; 13: 684-701. [ Links ]
41. Moorees CF. Natural head position – a revival. Am J Orthod Dentofacial Orthop 1994; 105: 512-513.
42. Lundstrom F, Lundstrom. A Natural head posture as a basis for cephalometric analyses. Am J Orthod Dentofacial Orthop 1992; 101: 244-247. [ Links ]
43. Houston WJB, Edler R. Longterm stability of the lower labial segment relative to the APog line. Eur J Orthod 1990; 12: 302-310. [ Links ]
44. McNamara JA, Ellis EE. Cephalometric evaluation of incisor position. Angle Orthod 1986; 56: 324-344. [ Links ]
45. Asad S, Naeem S, UlHamid W, Rcsed M. Relationship between lower incisor inclination, lower lip prominence& vertical pattern of the patient. Pakistan Oral & Dental J 2009; 29: 55-58. URL: http://www.podj.com.pk/Jul_2009/12PODJ.pdf [ Links ]
46. Aldress M. Evaluation of incisors inclination in five cephalo metric analysis methods. Pakistan Oral & Dental J 2010; 30: 419-424. URL: http://hdl.handle.net/123456789/14547 [ Links ]
47. Cornelius M, Linder Aronson S. The relationship between lower incisor inclination and various reference lines. Angle Orthod, 1976; 46: 111-117. [ Links ]
48. Williams R. Eliminating lower retention. J Clin Orthod 1985; 19: 342-349. [ Links ]
49. Williams R. The diagnostic line. Am J Orthod 1969; 55: 458-475. [ Links ]














