Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Acta Odontológica Latinoamericana
On-line version ISSN 1852-4834
Acta odontol. latinoam. vol.29 no.3 Buenos Aires Dec. 2016
ARTÍCULOS ORIGINALES
Temporomandibular joint involvement in rheumatoid arthritis patients: association between clinical and tomographic data
Patrícia C. F. Cordeiro1, Josemar P. Guimaraes1, Viviane A. de Souza2, Isabela M. Dias1, Jesca N. N. Silva1, Karina L. Devito1, Leticia L. Bonato3
1 School of Dentistry, Federal University of Juiz de Fora, Juiz de Fora, Minas Gerais, Brazil.
2 School of Medicine, Federal University of Juiz de Fora, Juiz de Fora, Minas Gerais, Brazil.
3 Estácio Juiz de Fora University, Juiz de Fora, Minais Gerais, Brazil.
CORRESPONDENCE Dr. Patricia Cataldo de Felipe Cordeiro Doutor Constantino Paleta St., 30/1301, Center Juiz de Fora/MG - CEP: 36015450, Brazil patricia.cataldo@hotmail.com
ABSTRACT
Rheumatoid arthritis (RA) is a systemic autoimmune disease characterized by chronic inflammation and synovial hyperplasia, which usually affects multiple joints. The temporomandibular joint (TMJ) becomes susceptible to the development of changes resulting from RA. The aim of this study was to evaluate the presence of TMD and degenerative bone changes in TMJ in patients diagnosed with RA (rheumatoid arthritis). The Research Diagnostic Criteria for Temporomandibular Disorders (RDC/ TMD) questionnaire was used for clinical evaluation of the TMJ and for TMD classification of 49 patients of both sexes and all ages. Individuals who had already undergone prior treatment for TMD and/or with a history of craniofacial trauma were excluded. The participants underwent cone beam computed tomography (CBCT) exams to assess possible degenerative changes in the mandibular condyle and the articular eminence. The frequencies of the changes found are presented and the possible associations between clinical and CT findings analyzed using the chisquare test. It was found that 75% of the patients had complaints of pain in the orofacial region, including arthralgia, myalgia or both. As for the diagnoses, 100% of the sample was diagnosed as RDC/TMD Group III (arthralgia, osteoarthritis or osteoarthrosis). The presence of degenerative bone changes was found in 90% of the subjects, the most prevalent being flattening (78.7%) and osteophytes (39.3%). The association test suggested a greater tendency to develop degenerative changes in asymptomatic individuals (p = 0.01). The asymptomatic nature of the involvement of the TMJ in RA can hide structural damage seen in imaging. Thus, the importance of early diagnosis and treatment to reduce structural and functional damage is emphasized.
Key words: Rheumatoid arthritis; Temporomandibular joint; Cone beam computed tomography; Temporomandibular disorder.
RESUMO
Envolvimento da articulação temporomandibular em pacientes com artrite reumatoide - associação entre dados clínicos e tomográficos
A artrite reumatoide (AR) é uma doença sistêmica, autoimune, caracterizada por inflamação crônica e hiperplasia sinovial, que usualmente afeta múltiplas articulações. Dentre estas, a articulação temporomandibular (ATM), tornase susceptível ao desenvolvimento de alterações. O estudo objetiva avaliar a presença de desordem temporomandibular (DTM) e altera ções ósseas degenerativas da ATM (articulação temporo man di bu lar) de pacientes diagnosticados com AR (artrite reumatóide). Como metodologia, aplicouse o questionário Research Diagnostic Criteria for Temporomandibular Disorder (RDC/ TDM) em para avaliação clínica da ATM e classificação da desordem temporomandibular em 49 pacientes de ambos os sexos e idade variável. Foram excluídos os indivíduos que já haviam realizado tratamento prévio para DTM e/ou com histórico de traumatismo crâniofacial. Posteriormente os participantes foram submetidos a exames de tomografia computadorizada de feixe cônico (TCFC) para avaliação de possíveis alterações degenerativas no côndilo mandibular e na eminência articular. Foram apresentadas as frequências das alterações encontradas e verificouse a associação entre os achados clínicotomográficos por meio do teste do Quiquadrado. Após a avaliação clínica verificouse que 75% dos pacientes possuíam queixas de dor na região orofacial, variando entre a presença de artralgia, mialgia ou ambas. Quanto aos diagnósticos, 100% da amostra apresentou diagnóstico do Grupo III do RDC/TMD (artralgia, osteoartrite ou osteoartrose). A presença de alterações ósseas degenera tivas foi encontrada em 90% dos indivíduos avaliados, sendo que as mais prevalentes foram aplainamento (78,7%) e osteófito (39,3%). O teste de associação sugeriu uma maior tendência de desenvolvimento de alterações degenerativas nos indivíduos assintomáticos (p = 0.01). O caráter assintomático do envolvimento da ATM na AR pode ocultar danos estruturais vistos em imagem. Assim, ressaltase a importância do diagnóstico e tratamento precoces para redução de danos estruturais e funcionais.
Palavras-chave: Artrite reumatoide; Articulação temporoman dibular; Tomografia computadorizada de feixe cônico.
INTRODUCTION
Rheumatoid arthritis (RA) is an autoimmune systemic disease characterized by chronic inflammation and synovial hyperplasia which usually affects multiple joints. Currently, it is considered the main inflammatory joint disorder, with a prevalence of 0.51% in the general population1. The incidence is higher in women, with varying proportions documented in the literature: 4:12, 7:13, and 9:14. While its autoimmune pattern is emphasized, various factors contribute to development of the disease, such as genetic predisposition, micro biological, hormonal and environmental factors5-8. Extensive infiltration of immune cells occurs, with high levels of inflammatory mediators in synovial tissue of peripheral joints9,10, and the abnormalities in the structure and function of such joints appear as the primary and characteristic manifestations in these patients.
The temporomandibular joint (TMJ) becomes susceptible to the development of changes resulting from RA. However, it is rarely the first joint to be affected5,6,11,12. It is estimated that more than half of the patients with RA present clinical evidence of involvement of the TMJ5,7,9,10, the most frequent being bilateral involvement. Clinically, the involvement of the TMJ follows the same destructive path as the other joints, correlating directly with the severity and duration of the RA that has taken hold7,13. In the initial phase, there may be synovial hyperemia, lymphocyte infiltration, fibrinoid degeneration and pannus formation (granulation tissue). The cartilage is destroyed and the granulation tissue can be seen in the joint cavity. From that point on, there may be fibrosis and scarring, generating fibrous adhesion. Fibrous ankylosis is the rarest and final stage that the TMJ affected by RA can attain10,14.
The most common clinical signs and symptoms in the TMJ are arthralgia, swelling, stiffness during mouth opening and upon waking, weakness of the masticatory muscles with decreased bite force, joint noises, and limited joint function2,57,10,15. Studies using cone beam computed tomography (CBCT), considered the gold standard for the analysis of degenerative bone changes of the TMJ, demonstrated that it is possible to find, in the TMJ of patients with RA, high prevalence of reduced joint space and serious erosion of cortical or subcortical bone, which can lead to destruction of the mandibular condyle11,16. Bone sclerosis, osteophytes and subcortical cysts may also occur6,7. However, the presence of changes in the TMJ of RA patients is often ignored by rheumatologists and even by patients, especially when treatment is focused on other joints of the upper extremities and/ or weightsupporting extremities. These changes in the TMJ may lead to complications and disability, making its treatment and monitoring extremely important.
The aim of this study was to evaluate the presence of TMD and degenerative bone changes in TMJ in patients diagnosed with RA by performing a clinical examination and analysis of CBCT images.
MATERIAL AND METHODS
This is a crosssectional, observational, descriptive study, approved by the Research Ethics Committee of the Federal University of Juiz de Fora (UFJF), under code number 771.869. Being an observational study, the sample was consisted of patients recruited randomly in one year, totalizing 49 volunteers. The study assessed patients previously diagnosed with RA treated at the Rheumatology Clinic of the University Hospital, UFJF. The diagnosis of RA was based on criteria established by the American College of Rheumatology, 1987, and ACR/EULAR 201017.
The patients diagnosed with RA were informed about the study and we included those who agreed to participate. All patients signed informed consent prior to participating in the research. Participation in the study was open to patients of both sexes and all ages. Exclusion criteria were pregnant women, individuals who had already undergone prior treatment for TMD and/or with a history of cranio facial trauma. The assessment was divided into two stages: assessment of clinical signs and symptoms in the TMJ and analysis of CBCT images. To assess the clinical signs and symptoms, we used Axis I of the Research Diagnostic Criteria for Temporomandi bular Disorders (RDC/TMD), the gold standard for clinical diagnosis of TMD18, which enabled patients to be classified into distinct groups according to the type of disorder: Group I) muscle disorders; Group II) disk displacement, and Group III) arthralgia, osteoarthritis and osteoarthrosis. The questionnaire was administered to all patients by a single trained and calibrated examiner according standards established by RDC/TMD18. CBCT images were obtained using theiCat Next Generation system (Imaging Sciences International, Hatfield, Pennsylvania, USA) operating at 120 kV and 38 mA, with the following acquisition protocol: 26.9 s exposure time, 8 cm FOV and 0.25 mm voxel. All images were obtained in the closed mouth position (maximum habitual intercuspation MHI). For the examination of each TMJ, a representative coronal section (most central region) of the condyle was selected, obtained via the TMJ window of the ICatVision software (Imaging Sciences International, Hatfield, Pennsylvania, USA). From this coronal section, sequential parasagittal sections were generated, where the articular bone changes were evaluated.
The bone surfaces of the mandibular condyle and the articular eminence of each TMJ were classified as: healthy (no change); flattening (loss of rounded contour of surfaces); with erosion (loss of continuity in cortical bone); with osteophytes (exophytic forma tion growing from surfaces); and with sclerosis (any increase in cortical thickness in loadbearing areas). Each possible change could appear alone or in combination. To identify the presence of bone changes, the condition had to be observed in at least two sequential parasagittal sections19.
This evaluation was performed by a radiologist with experience in TMJ CBCT images, without knowledge of the patient's clinical data. The evaluation was based on established criteria for tomographic analysis of the TMJ19. The absolute and relative frequencies of the changes found were presented and the association between clinical and CT findings were verified using the chisquare test. Calculations were performed using version 14.0 of the SPSS for Windows software, with a significance level of 5% (p≤0.05) and a 95% confidence interval.
RESULTS
Initially, 49 individuals who were undergoing clinical examination (RDC/TMD) for diagnosis of TMD were included in the study. Sixteen of them did not return to the institution for the CBCT exam, and were therefore excluded, with 33 subjects remaining in the study. All participants were female, with mean age 59.4 (± 10.3) years. Mean RA duration was 12.04 (± 8.57) years, being 13.36 (± 8.48) years in participants with presence of degenerative bone changes, and 3.66 (± 1.24) in individuals with no changes observed in CT. Through the combination of the RDC/TMD and the CBCT images, it was possible to observe that all subjects were diagnosed with TMD, presenting at least one diagnosis of Group III (arthralgia, osteoarthritis or osteoarthrosis). Of the 33 participants, 8 (24.2%) presented osteo arthritis, 21 (63.6%) had osteoarthritis, and 4 (12.1%) presented arthralgia. In association with the diagnosis of Group III changes, 13 (39.3%) individuals were also diagnosed with muscular disorder (Group I), and only 1 (3.0%) participant was diagnosed with Group II TMD (disc displacement).
In relation to the degenerative bone changes in the TMJ diagnosed in CBCT examinations, there was greater involvement of the condyle than the articular eminence, particularly from the flattening of the bone surfaces. It is also worth noting that a greater number of individuals with associated conditions of degenerative bone changes was observed. Considering the combined assessment of condyle and articular eminence, only 3 (9%) of the patients presented healthy structures, 11 (33.3%) had only one isolated bone change, and most (19 / 57.5%) presented more than one bone change simultaneously. Table 1 shows the prevalence of the degenerative bone changes of the TMJ, classified into flattening, osteophytes, erosion, and sclerosis. A total of 12 (36.36%) participants were considered as having arthralgia: four diagnosed with arthralgia alone and eight who also had osteoarthritis. Among the 30 (90.9%) individuals who had bone changes, nine (27.27%) also had arthralgia and 21 (60%) were asymptomatic. The three (9.09%) individuals without degenerative bone changes had joint pain, and no participant was free of the two conditions simultaneously. From the chisquare test, there was a significant association between the groups (p=0.01), suggesting a greater tendency to develop degenerative bone changes in asymptomatic indivi duals, compared to those who felt pain (Table 2).
Table 1: Prevalence of degenerative bone changes of the TMJ by individual.

Table 2: Association between the presence of degenerative change and arthralgia.

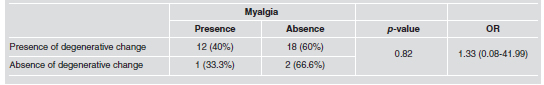
Similarly, the association was tested between the presence of degenerative changes and the cases of myalgia (Group I). Among the patients whose images showed condylar and/or articular eminence changes, 40% had muscle pain while 60% were asymptomatic. Among the patients with healthy bone structures, 66.6% presented no pain symptoms. As shown in Table 3, there was no significant association between the groups (p=0.82).
Table 3: Association between the presence of degenerative change and myalgia.
DISCUSSION
Rheumatoid arthritis acts as a systemic etiological factor with major impact on the development of temporomandibular disorders. However, since its clinical manifestations are often silent, the involvement of the TMJ in patients with RA has been ignored5,20. However, it was observed that 75% of the patients had complaints of pain in the orofacial region including arthralgia, myalgia, or both. In addition, 100% of the sample was diagno sed as RDC/TMD Group III, with impairment of the TMJ.
By means of the association between the clinical (RDC/TMD) and the CT exams −considered the gold standard for the diagnosis of degenerative bone changes associated with Group III21− the presence of changes was found in 90% of the participants. Flattening of the condylar surface, the bone change with the highest prevalence in the study, can be understood as a sign of adaptation and remodeling due to the person's age and/or degree of disk displacement; however the degree of flattening observed may be related to condylar destruction in these individuals19. The presence of osteophytes is directly related to the progression of osteoarthritis21. Erosion, observed in eight participants, seen as a cortical bone discontinuity, is characteristic of inflammatory degenerative processes such as in RA. While subcortical sclerosis of the condylar surface or fossa is considered a variation, especially when it comes to aging, remo deling, or association with mandibular hyperfunction as an attempt at protection. However, manifestation of generalized sclerosis of the subchondral bone is associated with joint degradation and may be a result of the presence of RA19. The duration of RA, especially when it is more than five years, is regarded as an aggravating factor for the involvement of the TMJ5,22. Degenerative bone changes such as the
presence of erosion and flattening in the mandibular condyle, are usually noticed in CT scans 5 to 10 years after the onset of symptoms4. Corroborating this statement, in the present study the patients with degenerative changes had an average RA duration of 13.36 (± 8.48) years, while patients with bilaterally healthy bone surfaces had an average RA duration of 3.66 (± 1.24) years. Therefore, the study suggests that the involvement of the articular bone structures occurs in more advanced stages of the disease. Nevertheless, it is worth noting that among patients with degenerative changes, the presence of joint pain in the TMJ was not proportional to the presence of bone changes. Of the 30 participants who had imagological changes, only nine complained of pain in the joint region, and 12 reported myalgia. Results show that the presence of arthralgia in the TMJ is associated with the early stages of the disease, acting as a signal of impairment in this joint in RA patients, as patients with advanced joint damage reported no pain. Similarly, one study7 showed images of the TMJ which revealed erosions in RA patients who had only mild discomfort or appeared free from symptoms in the TMJ, characterizing the silent manifestation in this joint. It should be considered, however, that the TMJ is structurally different from all the other joints, since it has retrodiscal tissue, rich in blood vessels, which can act as a highly efficient drainage system for common exudate. Thus, joint effusion and pain can be minimized or even extinguished in this joint5,6. However, the absence of pain in the RA patient does not mean the absence of TMJ impairment.
Temporomandibular disorders generally have prevalence characteristics similar to those affecting patients with RA, higher prevalence in females and the most common age group is 30 to 65 years, and thus may cause dentists to disregard the presence of RA. Similarly, due to the silent manifestation of TMJ, rheumatologists dismiss recommendations and treatments for this joint5,20. Thus, the quality of life and the pain levels in these patients may become compromised, making their treatment even more complex. A multidisciplinary team should work on this complex type of patient in an attempt to reduce the physical and psychological consequences of RA23. In addition, casecontrol studies and longitudinal studies on larger samples would help understand the involvement of the TMJ and its evolution in patients with RA, with the aim of helping them to achieve better quality of life.
CONCLUSION
According to this study, arthralgia of the TMJ in patients with RA acts as a signal of the onset of an active inflammatory process, in an attempt at protection, since individuals with advanced lesions did not complain of pain. The asymptomatic nature of the involvement of the TMJ in RA can hide structural damage seen in imaging. Therefore, the importance is emphasized of early diagnosis and treatment to reduce structural and functional damage.
1. Silman AJ, Pearson JE. Epidemiology and genetics of rheumatoid arthritis. Arthritis Res 4 2002;Suppl 3:S265-272. [ Links ]
2. Aliko A, Ciancaglini R, Alushi A, Tafaj A, Ruci D. Temporo mandibular joint involvement in rheumatoid arthritis, systemic lupus erythematosus and systemic sclerosis. Int J Oral Maxillofac Surg 2011; 40: 704-709. [ Links ]
3. Helenius LM, Tervahartiala P, Helenius I, Al-Sukhun J, Kivisaari L, Suuronen R, Kautiainen H, Hallikainen D, et al. Clinical, radiographic and MRI findings of the temporo man dibular joint in patients with different rheumatic diseases. Int J Oral Maxillofac Surg 2006; 35: 983-989. [ Links ]
3. Bessa-Nogueira RV, Vasconcelos BC, Duarte AP, Goes PS, Bezerra TP.Targeted assessment of the temporomandibular joint in patients with rheumatoid arthritis. J Oral Maxillofac Surg 2008; 66: 1804-1811. [ Links ]
4. Lin YC, Hsu ML, Yang JS, Liang TH, Chou SL, Lin HY. Temporomandibular joint disorders in patients with rheumatoid arthritis. J Chin Med Assoc 2007; 70: 527-534. [ Links ]
5. Mehra P, Wolford LM, Baran S, Cassano DS. Singlestage comprehensive surgical treatment of the rheumatoid arthritis temporomandibular joint patients. J Oral Maxillofac Surg 2009; 67: 1859-1872. [ Links ]
6. Yilmaz HH, Yildirim D, Ugan Y, Tunc SE, Yesildag A, Orhan H, Akdag C. Clinical and magnetic resonance imaging findings of the temporomandibular joint and masticatory muscles in patients with rheumatoid arthritis. Rheumatol Int 2012; 32: 1171-1178. [ Links ]
7. Symmons DP, Barrett EM, Bankhead CR, Scott DG, Silman AJ. The incidence of rheumatoid arthritis in the United Kingdom: results from the Norfolk Arthritis Register. Br J Rheumatol 1994;33: 735-739. [ Links ]
8. Hajati A, Nasstrom K, Alstergren P, Bratt J, Kopp S. Temporomandibular joint bone tissue resorption in patients with early rheumatoid arthritis can be predicted by joint crepitus and plasma glutamate level. Mediators Inflamm 2010; 627-803. DOI: 10.1155/2010/627803. [ Links ]
9. Ueno T, Kagawa T, Kanou M, Ishida N, Fujii T, Fukunaga J, Mizukawa N, Sugahara T. Pathology of the temporomandibular joint of patients with rheumatoid arthritis. Case reports of secondary amyloidosis and macrophage populations. J Craniomaxillofac Surg 2003; 31:252-256. [ Links ]
10. Klareskog L, Gregersen PK, Huizinga TW. Prevention of autoimmune rheumatic disease: state of the art and future perspectives. Ann Rheum Dis2010; 69: 2062-2066. [ Links ]
11. Moen K, Kvalvik AG, Hellem S, Jonsson R, Brun JG. The longterm effect of anti TNFalpha treatment on temporomandibular joints, oral mucosa, and salivary flow in patients with active rheumatoid arthritis: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 100: 433-440. [ Links ]
12. Sasaguri K, IshizakiTakeuchi R, Kuramae S, Tanaka EM, Sakurai T, Sato S. The temporomandibular joint in a rheumatoid arthritis patient after orthodontic treatment. Angle Orthod 2009; 79: 804-811. [ Links ]
13. Cunha CO, Pinto LM, de Mendonca LM, Saldanha AD, Conti AC, Conti PC. Bilateral asymptomatic fibrousankylosis of the temporomandibular joint associated with rheumatoid arthritis: a case report. Braz Dent J 2012; 23: 779-782. [ Links ]
14. Delantoni A, Spyropoulou E, Chatzgiannis J, Papademitriou P. Sole radiographic expression of rheumatoid arthritis in the temporomandibular joints: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 102: e37-40. [ Links ]
15. Kobayashi R, Utsunomiya T, Yamamoto H, Nagura H. Ankylosis of the temporomandibular joint caused by rheumatoid arthritis: a pathological study and review. J Oral Sci 2001; 43: 97-101. [ Links ]
16. Kay J, Upchurch KS. ACR/EULAR 2010 rheumatoid arthritis classification criteria. Rheumatology 2012; 51: vi59. [ Links ]
17. Dworkin SF, Le Resche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomand Disord 1992; 6: 301-355. [ Links ]
18. Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach RK, Truelove EL, John MT, Schiffman EL. Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD): Development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: 844-860. [ Links ]
19. Melchiorre D, Calderazzi A, Maddali-Bongi S, Cristofani R, Bazzichi L, Eligi C, Maresca M, Ciompi M. A comparison of ultrasonography and magnetic resonance imaging in the evaluation of temporomandibular joint involvement in rheumatoid arthritis and psoriatic arthritis. Rheumatology 2003; 42: 673-676. [ Links ]
20. Look JO, Schiffman EL, Truelove EL, Ahmad M. Reliability and validity of Axis I of the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) with proposed revisions. J Oral Rehabil 2010; 37: 744-759. [ Links ]
21. Celiker R, GokceKutsal Y, Eryilmaz M. Temporo mandibular joint involvement in rheumatoid arthritis. Relationship with disease activity. Scand J Rheumatol 1995; 24:22-25. [ Links ]
22. Sidebottom AJ, Salha R: Management of the temporoman dibular joint in rheumatoid disorders. Br J Oral Maxillofac Surg 2013; 51:191-198. [ Links ]














