Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Acta Odontológica Latinoamericana
versión On-line ISSN 1852-4834
Acta odontol. latinoam. vol.31 no.1 Buenos Aires abr. 2018
ORIGINAL ARTICLE
Inflamatory response in pregnant women with high risk of preterm delivery and its relationship with periodontal disease. A pilot study
Respuesta inflamatoria en pacientes embarazadas con alto riesgo de parto pretérmino y su relación con la enfermedad periodontal. Estudio piloto
Francina Escobar-Arregoces1, Catalina Latorre-Uriza1, Juliana Velosa-Porras1, Nelly Roa-Molina1, Alvaro J Ruiz2, Jaime Silva3, Estefania Arias4, Juliana Echeverri4
1 Pontificia Universidad Javeriana. Facultad de Odontología. Centro de Investigaciones Odontológicas, CIO. Bogotá D. C. Colombia,
2 Pontificia Universidad Javeriana. Facultad de Medicina, Departamento de Epidemiologia Clínica. Bogotá D. C. Colombia.
3 Hospital San Ignacio. Departamento de Ginecología y Obstetricia, Bogotá D. C. Colombia.
4 Practica Privada en Periodoncia, Colombia.
ABSTRACT
Periodontal disease and its inflammatory response have been related to adverse outcomes in pregnancy such as preterm birth, preeclampsia and low birth weight. This study analyzed systemic inflammatory response in patients with high risk of preterm delivery and its relationship to periodontal disease. A pilot study was conducted for a case and control study, on 23 patients at risk of preterm delivery and 23 patients without risk of preterm delivery as controls. Exclusion criteria were patients who had received periodontal treatment, antibiotic or antimicrobial agents within the past three months, or with infections or baseline diseases such as diabetes or hypercholesterolemia. All patients underwent periodontal assessment, laboratory tests (complete blood count, lipid profile, baseline glycemia) and quantification of cytokines (IL-2, IL-4, IL-6, IL-10, TNF-α and TNF-γ). Higher levels of pro-inflammatory cytokines (IL-2, IL-4, IL-6, IL-10, TNF-α and TNF-γ) were found in patients with chronic periodontitis than in patients with gingivitis or periodontal health. These cytokines, in particular IL-2, IL-10 and TNF-α, were higher in patients at high risk of preterm delivery. Patients with high risk of preterm delivery had higher severity of periodontal disease as well as higher levels of the pro-inflammatory markers IL-2, IL-4, IL-6, IL-10, TNF-α and TNF-γ.
Key words: Chronic periodontitis; Pregnancy; Preterm birth; Preterm labor; Cytokines.
RESUMEN
La enfermedad periodontal y su repuesta inflamatoria ha sido relacionada con desenlaces adversos del embarazo como el parto pretérmino, preeclampsia y bajo peso al nacer. La presente investigación analizó la respuesta inflamatoria sistèmica en pacientes embarazadas con alto riesgo de parto pretérmino y su relación con la enfermedad periodontal. Se realizó un estudio piloto de casos y controles, en el cual se contó con 23 pacientes que presentaban riesgo de parto pretérmino como casos y 23 pacientes sin riesgo de parto pretérmino como controles. Fueron excluidas las pacientes que hubieran recibido tratamiento periodontal, antibióticos o antimicrobianos en los últimos tres meses, que tuvieran infecciones, o enfermedades de base como diabetes o hipercolesterolemia. A todas las pacientes se les hicieron valoración periodontal, exámenes de laboratorio (cuadro hemático, perfil lipídico, glucemia basal) y cuanti-ficación de citocinas (IL-2, IL-4, IL-6, IL-10, TNF-α e TNF-γ). En las pacientes con periodontitis crónica se encontraron niveles más elevados en las citocinas proinflamatorias (IL-2, IL-4, IL-6, IL-10, TNF-α e TNF-γ) en comparación con las pacientes con gingivitis o sanas periodontales. Estas citocinas se encontraron más elevadas en las pacientes con alto riesgo de parto pretérmino, en especial la IL-2, IL-10 y TNF-α. Las pacientes con alto riesgo de parto pretérmino presentaron mayor severidad de la enfermedad periodontal y adicionalmente niveles aumentados de los marcadores pro inflamatorios IL-2, IL-4, IL-6, IL-10, TNF-α e TNF-γ.
Palabras clave: Periodontitis crónica; Embarazo; Nacimiento prematuro; Parto prematuro; Citocinas.
INTRODUCTION
Periodontal disease is a chronic infectious disease around the teeth which triggers a local and systemic inflammatory response1. The bacterial challenge generates an inflammatory infiltrate of polymorphonuclear neutrophils, monocytes, B-lymphocytes and T-lymphocytes with release of cytokines such as IL-1, IL-6 IL-8, IL-10 and PGE2, among others, which upon entering the bloodstream can reach the uterus and pass through the fetal placental barrier 2-4. Normal labor is controlled by inflammatory signaling. As the pregnancy progresses, PGE2, TNF-α and IL-1P levels increase to critical levels, which induce the rupture of the amniotic sac, followed by the beginning of uterine contractions and delivery5,6 This immune process, which is self-regulated up to the ninth month, may be modified by external stimuli such as periodontal infection, which by triggering a systemic inflammatory response during pregnancy, could induce labor earlier than necessary. Preterm birth is defined as birth at fewer than 37 weeks gestational age 7. Global incidence of preterm birth is about 9.6%, which is equivalent to 12.9 million preterm babies 7-9. It is a frequent problem which even affects high-income countries and has a strong impact on maternal and child morbidity and mortality, affecting both families and healthcare systems10,11.
The aim of this study was to analyze the systemic inflammatory response in pregnant patients with high risk of preterm delivery and its relationship with periodontal disease.
MATERIALS AND METHODS
A pilot test was conducted for a case and control study. The sample consisted of 46 patients - 23 at risk of preterm delivery and 23 without that risk as controls. Risk of preterm delivery was diagnosed following the Clinical Practice of the Obstetrics and Gynecology Service at Hospital San Ignacio12, which define preterm delivery as follows: 1. Risk of preterm delivery: patients with uterine activity without cervical changes. 2. Preterm labor, initial phase: patients with regular uterine activity and cervical changes less than 4 cm y 3. Preterm labor, advanced phase: patients with uterine activity with cervical changes greater than 4 cm.
The patients who took part in the study as cases were hospitalized and at risk of phase 1 and 2 preterm labor. The patients in the control group were pregnant women who attended their normal prenatal checkup as outpatients at the same hospital and Javesalud. Exclusion criteria for both groups were having received periodontal treatment, antibiotics or antimicrobial agents within the past three months, or having active infections or baseline diseases such as diabetes or hypercholesterolemia. According to Colombia's Ministry of Health13 and the CIOMS14, this study was classified as investigation with minimum risk and was approved by the research ethics committees of the School of Medicine (FM-CIE 841215) and the School of Dentistry (CIEFOUJ OD 0131) of Universidad Javeriana. Before enrolling in the study, each patient signed an informed consent. Blood samples were taken to determine full blood count, glycemia, total cholesterol, triglycerides, cHDL, cLDL and quantification of the inflammatory markers IL-2, IL-4, IL-6, IL-10, TNF-α and TNF-γ using the BD Cytometric Bead Array Human Th1/Th2 Cytokine Kit II. The Beckton Dickinson FACSCanto II flow cytometer acquired 50,000 events and the data were analyzed using FCAP Array software. Concentrations were expressed in pg/ml. Periodontal disease was diagnosed based on the Armitage classification, 1999. 15 (Fig. 1).
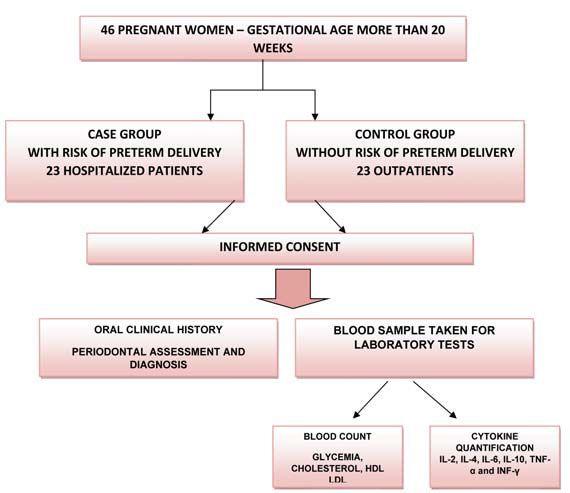
Fig. 1: Flow diagram showing patient enrollment and testing. The flow diagram shows patients enrolled in the study, with the subgroups formed for Cases (pregnant women with risk of preterm delivery) and controls (pregnant women without risk of preterm delivery). All patients signed informed consent, underwent periodontal clinical assessment and had a blood sample taken for full blood count, glycemia, total cholesterol, HDL, LDL and cytokine quantification.
To analyze the information, a description was made of the demographics, results of periodontal evaluation and systemic inflammatory markers using means, medians, ranges, standard deviations and 95% confidence intervals. For the bivariate analysis, the Chi-square test was used to establish associations and the ANOVA test to establish differences between the averages for the variables of interest. In addition, the Kolmogorov-Smirnov test was performed to establish whether the inflammatory markers had normal behavior. Variables in which behavior was not normal were compared using the U-Mann Whitney test. A difference of p < 0.05 (two-tailed) was considered significant.
RESULTS
General characteristics
Forty-six patients were analyzed. Average age was 25.91 ± 6.4 years and average gestational age was 29.46 ± 4.3 weeks. For periodontal status, 50.0% had chronic periodontitis, 45.7% had gingivitis associated to biofilm and 4.3% periodontal health. Upon describing according to groups, average age for both groups was 26 years, and gestational age was 31 weeks for the group with high risk and 28 weeks for the group without risk (p = 0.466).
Oral clinical characteristics
No statistically significant difference was found for number of teeth or O'Leary's plaque index. The group with high risk of preterm delivery included a larger number of patients diagnosed with chronic periodontitis than the group without risk (Table 1).
Table 1: Clinical characteristics of pregnant women with high risk and without risk of preterm delivery.

Cytokine quantification
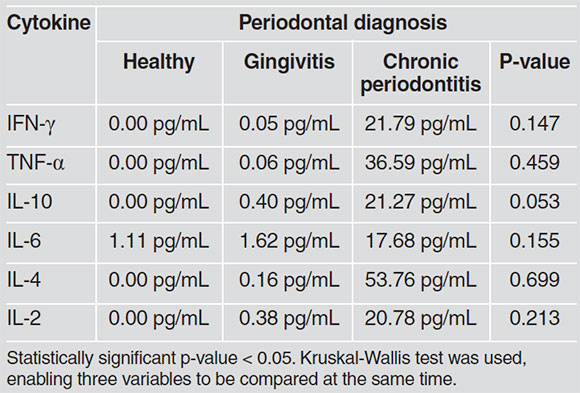
Patients in the group with high risk of preterm delivery had higher levels of cytokines than patients without risk, with significant statistical differences for TNF-α, IL-10 and IL-2 (Table 2). For relationship between cytokines and periodontal diagnoses, patients with chronic periodontitis tended to have higher levels of pro-inflammatory cytokines than patients with gingivitis or periodontal health. Although the trend was towards higher values of cytokines in patients with periodontitis, it should be noted that there was no significant statistical difference in cytokine concentration according to diagnosis. Since the variables did not have normal behavior, a Kruskall Wallis test was used, which showed no significant difference in distribution between groups (Table 3).
Table 2: Cytokine quantification in pregnant women with high risk and without risk of preterm delivery.

Table 3: Relationship between cytokines and periodontal diagnosis.
DISCUSSION
Current evidence suggests that preterm delivery originates mainly from ascending infections from the vagina or uterine cervix, or blood-borne propagation from non-genital sources. Maternal periodontitis is a non-genital source of microorganisms which are known to routinely enter the bloodstream and to have potential to influence the health of the fetoplacental unit7.
This study evaluated systemic inflammatory response in pregnant patients with and without risk of preterm delivery and its relationship with periodontal disease. The results showed that patients with high risk of preterm delivery had higher levels of cytokines IL-2, IL-4, IL-6, IL-10, TNF-α and TNF-γ. These findings are in agreement with Inglis et al. 16, Gursoy et al. 17, von Minckwitz et al. 18 and Turhan et al. 19, which associate increased systemic inflammatory marker levels with adverse events in pregnancy.
Inflammatory cytokines play a key role in the mechanisms that trigger labor. This study found increased quantities of IL-6 and IL-10 in patients with risk of preterm delivery, in agreement with Arntzen et al. 20, Romero et al. 21 and Wommack et al. 22. The current study also found that the group with risk of preterm delivery included a larger number of patients diagnosed with chronic periodont itis than the group without risk. This is in agreement with Offenbacher et al. 23, who report for the first time a relationship between maternal periodontal disease and preterm birth.
Upon analyzing presence of cytokines with relation to periodontal status, it was found that the group of patients with periodontitis tended to have higher levels of cytokines IL-2, IL-4, IL-6, IL-10, TNF-α and TNF-γ; in agreement with Kelso24 and Zadeh et al. 25, who relates periodontal infection to a systemic inflammatory response, reporting an increase in IL-5, IL-6, IL-4, IL- 10 IL-13 IL-3 and TNF-α in patients with periodontitis. Similarly, Perunovik et al. 26 found that women with preterm delivery had significantly more periodontitis and higher levels of IL-6 and PGE2 in crevicular fluid than the term delivery group.
Studies in recent years have focused on the effect of periodontal treatment on the reduction of proinflammatory markers and its relationship with preterm delivery. Offenbacher et al. 27 report that periodontal treatment showed a reduction in preterm delivery rate by 3.8 times, and a decrease in IL-1P and IL-6. Penova-Veselinovic,28 found that in the group with periodontal treatment there was a significant reduction in levels of IL-1P, IL-10, IL-12p70 and IL-6 compared to controls. Da Silva et al. 29 report in a meta-analysis that non-surgical periodontal therapy during pregnancy reduced the level of inflammatory biomarkers in gingival crevicular fluid and serum, without influence on the level of inflammatory biomarkers in umbilical cord blood and without reducing the occurrence of adverse gestational outcomes.
However, in contrast to the above, studies such as Michalowicz et al. 30, Fiorini T, et al. 31 and Pirie M, et al. 32 report that non-surgical periodontal treatment in pregnant women did not reduce systemic inflammation markers.
Considering that preterm delivery is a public health issue, preventive measures should be taken, including promoting periodontal health in pregnant women. Unfortunately, as reported by Duque et al. 33 in 2011, physicians' knowledge and attitudes regarding periodontal disease and general health status are still deficient. Greater efforts are therefore needed to raise awareness among the different groups of scientists and specialists regarding the importance of maintaining good periodontal health during the gestation period, given the biological plausibility for etiology of preterm delivery shown by periodontal disease.
Within the limitations of the current study, it may be concluded that patients with high risk of preterm delivery presented greater severity of periodontal disease as well as increased levels of the proinflammatory markers IL-2, IL-4, IL-6, IL-10, TNF-α and TNF-γ, with statistically significant differences for IL-2, IL-10 and TNF-α.
ACKNOWLEDGMENTS
The authors thank Javesalud for help with obtaining the sample, the clinical laboratory Hospital Universitario San Ignacio, Flow Cytometry department, and Beckton Dickinson for advice and technical support. This study was financed by the Office of the Vice-Rector of Research at Pontificia Universidad Javeri-ana, Bogotá, Colombia.
CORRESPONDENCE
Dr. Francina Maria Escobar Arregoces
Carrera 7 # 40-62 Universidad Javeriana, Facultad de Odontología Bogotá, Colombia
escobar.f@javeriana.edu.co
1. Contreras A, Herrera JA, Soto JE, Arce RM, et al. Periodontitis is associated with preeclampsia in pregnant women. J Periodontol. 2006; 77:182-188. [ Links ]
2. Van Dyke TE, Van Winkelhoff AJ. Infection and inflammatory mechanisms. J Clin Periodontol. 2013; 40:S1-7. [ Links ]
3. Page RC, Offenbacher S, Schroeder HE, Seymour GJ, et al. Advances in the pathogenesis of periodontitis: summary of developments, clinical implications and future directions. Periodontol 2000. 1997; 14:216-248. [ Links ]
4. Ardila CM, Lafaurie GI. Asociación entre porphyromona gingivalis y proteína C reactiva en enfermedades sistémicas inflamatorias. Av Periodon Implantol 2010; 22:45-53. [ Links ]
5. Armitage GC. Bi-directional relationship between pregnancy and periodontal disease. Periodontol 2000. 2013; 61:160-176. [ Links ]
6. Madianos PN, Bobetsis YA, Offenbacher S. Adverse pregnancy outcomes (APOs) and periodontal disease: pathogenic mechanisms. J Clin Periodontol 2013; 40:S170-180 doi:10.1111/jcpe. 12082 [ Links ]
7. Sanz M, Kornman K. Periodontitis and adverse pregnancy outcomes: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J Clin Periodontol 2014; 40:S164-169. doi:10.1111/jcpe. 1208 [ Links ]
8. Saini N. , Walia M. Relationship between periodontal diseases and preterm birth: Recent epidemiological and biological data. Int J Appl Basic Med Res 2015; . 5, 2. doi: 10.4103/2229-516x. 149217 [ Links ]
9. Villanueva L, Contreras AK, Pichardo M, Rosales J. Perfil epidemiológico del parto prematuro. Artículo de revisión. Ginecol Obstet Mex 2008; 76:542-548. [ Links ]
10. Ide M, Papapanou PN. Epidemiology of association between maternal periodontal disease and adverse pregnancy outcomes- systematic review. J Clin Periodontol 2013; 40: 181-194. [ Links ]
11. Castaldi JL, Bertin MS, Giménez F, Roberto L. Enfermedad periodontal: ¿es factor de riesgo para parto pretérmino, bajo peso al nacer o preeclampsia? Rev Panam Salud Pública. 2006; 19:253-258. [ Links ]
12. Guía Institucional Hospital Universitario San Ignacio. Intranet Almera. Guía Práctica Clínica Parto Pretérmino. 2014. [ Links ]
13. Normas científicas, técnicas y administrativas para la investigación en salud, Resolución 8430 de 1993, República de Colombia. Ministerio de Salud, (1993). URL: www.dib.unal.edu.co/promocion/etica_res_8430_1993.pdf [ Links ]
14. Consejo de las Organizaciones Internacionales de Ciencias Médicas (CIOMS). Guías Éticas Internacionales para la Investigación Biomédica que involucra Seres Humanos.[Programa Regional de Bioética OPS/OMS]. 2-8-2010. URL: www.paho.org/Spanish/BIO/CIOMS
15. Armitage G. Diagnóstico y clasificación de las enfermedades periodontales. Periodontol 2000. 2005; 9:9-21. [ Links ]
16. Inglis SR. Biochemical markers predictive of preterm delivery. Infect Dis Obstet Gynecol. 1997; 5:158-164. [ Links ]
17. Gürsoy M, Kononen E, Gürsoy UK, Tervahartiala T, et al . Periodontal Status and Neutrophilic Enzyme Levels in Gingival Crevicular Fluid During Pregnancy and Postpartum. J Periodontol 2010; 18:1790-1796. [ Links ]
18. von Minckwitz G, Grischke EM, Schwab S, Hettinger S, et al. Predictive value of serum interleukin-6 and -8 levels in preterm labor or rupture of the membranes. Acta Obstet Gynecolo Scand. 2000; 79:667-672. [ Links ]
19. Turhan NO, Karabulut A, Adam B. Maternal serum interleukin 6 levels in preterm labor: prediction of admission-to-delivery interval. J Perinat Med. 2000; 28:133-139. [ Links ]
20. Arntzen KJ, Kjollesdal AM, Halgunset J, Vatten L, et al. TNF, IL-1, IL-6, IL-8 and soluble TNF receptors in relation to chorioamnionitis and premature labor. J Perinat Med. 1998; 26:17-26. [ Links ]
21. Romero R, Avila C, Santhanam U, Sehgal P. Amniotic fluid Interleukin 6 in preterm labor. Association with infection. J Clin Invest. 1990; 85:1392-1400. [ Links ]
22. Wommack JC, Ruiz RJ, Marti CN, Stowe RP, et al. Interleukin-10 predicts preterm birth in acculturated hispanics. Biol Res Nurs. 2013; 15:78-85. [ Links ]
23. Offenbacher S, Jared HL, O'Reilly PG, Wells SR, et al. Potential pathogenic mechanisms of periodontitis associated pregnancy complications. Ann Periodontol. 1998; 3:233-250. [ Links ]
24. Kelso A. Th1 and Th2 subsets: paradigms lost? Immunol Today. 1995; 16:374-379. [ Links ]
25. Zadeh HH, Nichols FC, Miyasaki KT. The role of the cell-mediated immune response to Actinobacillus actinomycetemcomitans and Porphyromonas gingivalis in periodontitis. Periodontol 2000. 1999; 20:239-288. [ Links ]
26. Perunovic ND, Rakic MM Nikolic LI, Jankovic SM, et al. The Association Between Periodontal Inflammation and Labor Triggers (Elevated Cytokine Levels) in Preterm Birth: A Cross-Sectional Study. J Periodontol 2016^ Mar; 87:248-256. [ Links ]
27. Offenbacher S, Lin D, Strauss R, McKaig R, et al. Effects of periodontal therapy during pregnancy on periodontal status, biologic parameters, and pregnancy outcomes: a pilot study. J Periodontolol 2006; 77:2011-2024. [ Links ]
28. Penova-Veselinovic B, Keelan JA, Wang CA, Newnham JP, et al. Changes in inflammatory mediators in gingival crevicular fluid following periodontal disease treatment in pregnancy: Relationship to adverse pregnancy outcome. J Reprod Immunol 2015; 112:1-10. [ Links ]
29. Da Silva HEC, Stefani CM, de Santos Melo N, de Almeida de Lima A, et al. Effect of intrapregnancy nonsurgical periodontal therapy on inflammatory biomarkers and adverse pregnancy outcomes: a systematic review with meta-analysis. Syst Rev. 2017 Oct 10;6:197. doi: 10.1186/s 13643-017-0587-3. [ Links ]
30. Michalowicz BS, Novak MJ, Hodges JS, DiAngelis A, et al. Serum inflammatory mediators in pregnancy: changes after periodontal treatment and association with pregnancy outcomes. J Periodontol 2009; 80:1731-1741. [ Links ]
31. Fiorini T, Susin C, da Rocha JM, Weidlich P, et al. Effect of nonsurgical periodontal therapy on serum and gingival crevicular fluid cytokine levels during pregnancy and postpartum. J Periodontal Res 2013; 48 :126-133. [ Links ]
32. Pirie M, Linden G, Irwin C. Intrapregnancy non-surgical periodontal treatment and pregnancy outcome: a randomized controlled trial. J Periodontol 2013; 84:1391-1400. [ Links ]
33. Duque A, Tirado M, Arbelâez C, Garcia, S Conocimientos y actitudes sobre periodontitis como factor de riesgo de algunas enfermedades y condiciones médicas en médicos. Rev Colomb Investig en Odontol 2011; 12:262-272. URL:https://www.rcio.org/index.php/rcio/article/viewFile/9/90 [ Links ]














