Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Acta Odontológica Latinoamericana
On-line version ISSN 1852-4834
Acta odontol. latinoam. vol.31 no.3 Buenos Aires Dec. 2018
ORIGINAL ARTICLE
Relation between periapical lesions and sinus membrane thickening assessed by Cone Beam Computed Tomography
Lesiones periapicales y engrasamiento de la membrana sinusal, su relación y valoración a través de Tomografía Computarizada de Haz Cónico
Gisela V. Brañas1, Brenda G. Grisolia1, Romina G. Iuliano1, Ariel Gualtieri2, Ariel Lenarduzzi1, Sandra J. Renou3, Pablo A. Rodríguez1
1 Universidad de Buenos Aires, Facultad de Odontología, Cátedra de Endodoncia, Hospital Odontológico Universitario.
2 Universidad de Buenos Aires, Facultad de Odontología, Cátedra de Biofísica y Bioestadística, Hospital Odontológico Universitario.
3 Universidad de Buenos Aires, Facultad de Odontología, Cátedra de Anatomía Patológica, Hospital Odontológico Universitario.
ABSTRACT
The aim of this study was to evaluate thickening of the Schneiderian membrane and to determine its association with periapical pathologies, using computerized cone beam tomography. An observational, analytical, cross-sectional retrospective study was conducted. A total 179 maxillary sinuses were evaluated using CBCT. The presence of sinus membrane thickening and its association with unhealthy teeth was analyzed. Results are shown as percentages with 95% confidence intervals (95%CI); Chi square test was used with a significance level of 5%.
Sinus membrane thickening was detected in 70 cases (39%; 95%CI=32% to 46%) and no sinus membrane thickening was observed in 109 (61%; 95%CI = 54% to 68%) (p<0.05). The 70 cases showing sinus membrane thickening included 46 of odontogenic origin (66%; 95%CI = 54% to 76%) and 24 (34%; 95%CI = 24% to 46%) of non odontogenic origin (p<0.05). The frequency of odontogenic causes followed a heterogeneous distribution (p<0.05): penetrating caries, failing endodontic therapy, root remnants, deep restorations, implants, periodontal pathology. The main cause was caries (46%; 95%CI=32% to 60%) followed by failing endodontic therapy (26%, 95% CI=16% to 40%). The frequency distribution of involved teeth was uneven (p<0.05), with tooth 16 (33%; 95%CI=21% to 47%) being the most frequently involved, followed by tooth 26 (30%; 95%CI=19% to 45%).
The high incidence of sinus pathology of odontogenic origin shows the need for interdisciplinary work involving dentists and ear-nose-throat specialists. Caries, inadequate restorations, periodontal lesions, implants, and the presence of root remnants are the main causes of Schneiderian membrane thickening. The use of CBCT for diagnosis and treatment planning allows detecting maxillary sinus membrane thickening and determining its association with an odontogenic etiology.
Key words: Maxillary sinus; Periapical tissues; Cone beam computerized tomography; Schneiderian membrane.
RESUMEN
El objetivo del presente trabajo fue evaluar el engrosamiento de la membrana de Schneider y determinar su asociación con patologías periapicales, mediante tomografía computarizada cone beam (CBCT). Se realizó un estudio observacional, analítico, retrospectivo y transversal. Un total de 179 senos maxilares fueron evaluados utilizando CBCT. Se analizó la presencia de engrosamiento de la membrana sinusal y su asociación con piezas dentarias sin vitalidad pulpar. Los resultados se muestran como porcentajes con intervalos de confianza del 95% (IC del 95%). Se utilizó la prueba de Chi cuadrado con un nivel de significación del 5%.
Se detectó engrosamiento de la membrana sinusal en 70 casos (39%; IC del 95% = 32% a 46%) y no se observó engrosamiento de la membrana sinusal en 109 (61%; IC del 95% = 54% a 68%) (p < 0.05). Los 70 casos que mostraron engrosamiento de la membrana sinusal incluyeron 46 de origen odontogénico (66%; IC del 95% = 54% a 76%) y 24 (34%; IC del 95% = 24% a 46%) de origen no odontogénico (p <0,05). La frecuencia de las causas odontogénicas siguió una distribución heterogénea (p <0.05): caries penetrantes, tratamiento endodóntico deficiente, restos radiculares, restauraciones profundas, implantes, patología periodontal. La principal causa fue la caries (46%; IC 95% = 32% a 60%), seguida por endodoncia deficiente (26%, IC 95% = 16% a 40%). La frecuencia se distribuyó en forma heterogénea entre las distintas piezas (p<0,05). Las piezas más afectadas fueron la 16 (33%; IC95=21% a 47%) y la 26 (30%; IC95=19% a 45%). La alta incidencia de patología sinusal de origen odontogénico implica la necesidad del trabajo interdisciplinario entre odontólogos y otorrinolaringólogos. Caries, restauraciones inadecuadas, lesiones periodontales, implantes y la presencia de restos radiculares son las principales causas del engrosamiento de la membrana de Schneider. El uso de CBCT para el diagnóstico y la planificación del tratamiento permite detectar el engrosamiento de la membrana del seno maxilar y determinar su asociación con una etiología odontogénica.
Palabras clave: Seno maxilar; Tejidos periapicales; Tomografía computada cone beam; Membrana de Schneider.
INTRODUCTION
The maxillary sinus is the main paranasal sinus, and is located in the body of the maxilla. At the end of dento-maxillo-facial growth, the floor of the maxilla presents its final anatomical features. At this point, the teeth and the sinus floor are in close anatomical proximity, and this close anatomical relationship only differs among individuals1. Accurate knowledge of the anatomy of the maxillary sinus is paramount to the general dentist, since it allows recognizing the diversity of sinus pathologies of oral origin, and preventing iatrogenic complications associated with dental and surgical procedures.
The maxillary sinuses are anatomically located in an intermediate position between the nasal and oral cavities, and are therefore susceptible to invasion by pathogenic bacteria through the nasal ostium or the oral cavity2.
The maxillary sinuses consist of two pairs of symmetrical cavities that occupy the central part of the maxilla. The lower wall extends from the roots of the upper premolars to the roots of the molars. The canine roots may occasionally project into the sinus. The premolar and molar roots are generally immediately below the floor of the maxillary sinus; this proximity explains the causal relationship between dental pathology and pathologies of the maxillary sinus, such as sinusitis3. Sinus pathology is common in patients presenting dental pathologies such as periapical lesions, cysts, and tumors4. Alterations in the Schneiderian membrane can manifest as uniform thickening and hypertrophy, and/or the presence of polyps and solid or cystic masses, which can be observed by computed tomography. The finding of mucosal thickening in cone beam computerized tomography (CBCT) per se does not allow establishing differential diagnosis between acute and chronic disease, and clinical evaluation is necessary for accurate diagnosis5. Radiographic techniques, such as panoramic radiographs, Waters radiograph, computed tomography, magnetic resonance imaging, and CBCT, are frequently used to diagnose maxillary sinus pathology. Cone beam computed tomography is considered the "gold standard" for diagnosing maxillary sinus pathology because of its high resolution and ability to visualize bone and soft tissues4.
Maxillary sinusitis is a common pathology worldwide, and has significant health impacts. A substantial proportion of maxillary sinus cases is of odontogenic origin, given the proximity of the roots of maxillary posterior teeth to the sinus floor6.
The bony wall that separates the maxillary sinus from the tooth roots can vary in thickness, reaching up to 12 mm. In some cases the wall is absent, and the roots are only covered by a membrane7.
Dental pathologies of infectious origin are very common, though they account for only 5 to 10% of all cases of maxillary sinusitis. Sinus membrane integrity can be disrupted in a number of situations, as is the case of trauma causing iatrogenic displacement of a tooth or implant, treatment of periapical lesions, periodontal pathologies, teeth with extensive caries, and teeth with apical infections. Certain materials, such as gutta-percha, are inert and therefore cause no reaction in the sinus. Hence, no treatment is necessary in the absence of symptoms. However, in the event that chronic or acute sinusitis develops, the condition will not be resolved satisfactorily until the cause is eliminated8.
The aims of the present work were to evaluate thickening of the Schneiderian membrane and to determine its association with periapical pathologies, using computerized cone beam tomography.
MATERIALS AND METHODS
Cone beam computed tomography scans performed for diagnosis of pathology and treatment planning of patients seen at the Department of Endodontics of the School of Dentistry, University of Buenos Aires, between March 2016 and September 2016 were analyzed. The project was approved by the Ethics Committee of the School of Dentistry of the University of Buenos Aires (Res N° 921/14).
CBCT scans of male and female patients over the age of18 years, requested for treatment (assessment of missing teeth for implant treatment) or diagnostic purposes (evaluation of existing pathologies, endodontic evaluation), and which allowed visualization of the entire maxillary sinus in the coronal and axial sections were included in the study. CBCT scans corresponding to patients who smoked, had systemic disease, abused drugs, were taking some type of medication at the time of the CBCT, and/or failed to sign the informed consent form to participate in the study were excluded from the study.
All CBCT scans were taken with the same Scanner (Kodak 9000C 3D, FOV 5 X3.75 cm), at the Imaging diagnosis Department of the School of Dentistry, University of Buenos Aires.
The present observational, analytical, crosssectional, retrospective study was conducted by a single operator, who evaluated the computerized images, first observing the panorex and then thoroughly examining the para-axial sections of the involved teeth. In keeping with the analyzed bibliography, sinus alteration was considered sinus mucosa thickening when membrane thickness was greater than 2mm 9-12.
Membrane thickness was determined on coronal sections, taking the maximum thickness as reference (Fig. 1). Odontogenic origin was evaluated taking into account the following 4 situations: 1) teeth with penetrating caries, root remnants with periapical lesions, and teeth with endoperiodontal lesions (with severe attachment loss); 2) teeth with restorations and recurrent caries; 3) endodontically treated teeth with unsuccessful treatment outcome (visible periapical lesions/lesions on CBCT scan), or with filling material inside the sinus; 4) no dental cause; this group comprised all cases of nonodontogenic origin13,14.
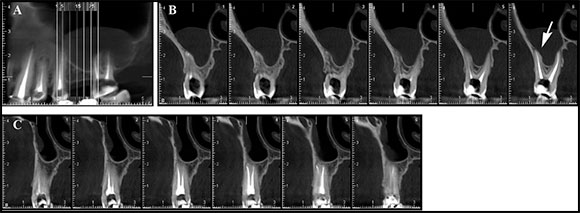
Fig. 1: A Panorex shows membrane alteration in the right sector. B and C The images of the corresponding sections allow evaluating the close relation between the root and the maxillary sinus floor, and the increase in the thickness of the Schneiderian membrane (↑).
The recorded data were analyzed to obtain absolute frequencies and percentages. Ninety-five percent confidence intervals (95%CI) for percentages were obtained using the Wilson score method15. Frequencies were compared using Chi square test Statistical significance was set at 5%.
RESULTS
A total 179 CBCT scans were analyzed; significant sinus membrane thickening was observed in 70 cases (39%; 95%CI = 32% to 46%, Chi-square = 8.50; gl = 1; p < 0.05, Fig. 2). A significantly higher number of cases of membrane thickening were of odontogenic origin (66%; 95%CI = 54% to 76%), accounting for 46 cases as compared to 24 cases of non-odontogenic etiology 34%; 95%CI = 24% to 46%). With regard to cases of sinus pathology of odontogenic origin, an uneven frequency distribution of the different causes was observed (Chi-square = 36.96; gl = 5; p < 0.05; Fig. 3). Specifically, the frequency of caries and endodontic treatment (72%; 95%CI = 57% to 83%) was significantly higher than that of the remaining causes (Chi-square = 8.70; gl = 1; p < 0.05); however, no statistically significant differences were observed between caries and endodontic treatment (Chi-square = 2.45; gl = 1; p = 0.12), nor when comparing root remnants, restorations, implants, and periodontal pathology (Chi-square = 2.69; gl = 3; p = 0.44).
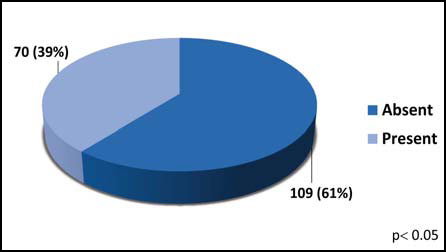
Fig. 2: Presence of sinus membrane thickening. Absolute frequencies are shown with corresponding percentage in brackets (Chisquare: p < 0.05).

Fig. 3: Frequency distribution of odontogenic causes of sinus pathology. Absolute frequencies are shown with the corresponding percentage in brackets (Chisquare: p < 0.05).
An uneven frequency distribution was also observed when analyzing the frequency of affected teeth in cases of sinus pathology of odontogenic origin (Chi-square = 42.00; gl = 7; p < 0.05; Fig. 4). In this group of cases, the tooth most frequently associated with sinus pathology was tooth 1.6 (33%; 95%CI = 21% to 47%), and was significantly more involved than teeth 1.4 (Chi-square = 15; gl = 1; p < 0.05), 15 (Chi-square = 12.25, gl = 1; p < 0.05), 1.7 (Chi-square = 5.00; gl = 1; p < 0.05), 2.4 (Chi-square = 8.00; gl = 1; p < 0.05) and 2.5 (Chi-square = 12.25, gl = 1; p < 0.05); no significant differences were observed between the frequency of tooth 1.6 and teeth 2.6 (Chi-square = 0.03; gl = 1; p = 0.85) and 2.7 (Chi-square = 2.91; gl = 1; p = 0.09).

Fig. 4: Frequency distribution of teeth associated with sinus pathology of odontogenic origin Absolute frequencies are shown with the corresponding percentage in brackets (Chisquare: p < 0.05).
DISCUSSION
Maxillary sinusitis is a frequent pathology, and is associated with odontogenic etiologies in a number of situations. Thus, dentists must be familiar with its diagnosis and prevention. The present article sought to evaluate cases of sinus mucosal thickening greater than 2mm, considered a sign of pathology in keeping with the literature, associated with dental pathology.
Although odontogenic maxillary sinusitis has traditionally been reported to account for approximately 10 to 12% of all cases of maxillary sinusitis, a review of more recent reports suggests a higher prevalence, ranging between 30 and 40%13. According to a study on 770 cases, the percentage of maxillary sinusitis cases of odontogenic origin was 37-40.6%. In the present study, 66% of cases showed membrane thickening associated with odontogenic causes. Therefore, development of caries could be considered the major cause of sinus pathology. The second most frequent cause in the series of cases studied here was endodontic treatment, with no statistically significant differences in frequency as compared to caries. Usually, the roots of premolars and molars are separated from the floor of the maxillary sinus by a dense cortical bone of varying thickness. Sometimes, however, only the mucoperiosteum separates the sinus from the teeth14. Clearly, this anatomical proximity could explain the origin and development of an inflammatory process that could cause thickening of the sinus mucosa.
A number of studies found iatrogenic injury during dental procedures and chronic periodontitis to be the most common cause of spread of oral pathogens into the maxillary sinus, and considered them the main cause of sinus mucosa thickening15. According to a review of 35 studies, iatrogenic etiology accounted for 55.9% of cases. Extrusion of dental filling materials during endodontic treatment accounted for 22.27% of iatrogenic etiology7. In the present study, endodontic pathology was the second cause of sinus membrane thickening, though no significant differences were observed with regard to the frequency of caries-related cases. Examination of the CBCT scans included in the present study allowed detecting cases of overfilling with materials, such as guttapercha, with no sinus alteration. This could be an indication of the biocompatibility of said material, which would account for the absence of an inflammatory process at the apical level.
Proper chemical preparation, maintaining apical permeability, and use of the corono-apical technique for endodontic treatment, contribute to decreasing the likelihood of spread of microorganisms to the maxillary sinus.
Periodontal disease has long been reported as an etiological factor of sinus mucosa inflammation. For example, in their 1943 study in human cadavers, Bauer et al. demonstrated direct diffusion of oral sepsis to the maxillary sinus. More recently, Abrahams et al.16 reported the incidence of sinusitis in patients with periodontal disease to be two-fold that of patients without periodontal disease. Recognition of the close relationship between inflammation of periapical tissues and damage to the sinus membrane led to describing the pathological entity referred to as the "endo-antral syndrome. In recent years, however, the incidence of these effects has decreased, likely due to factors such as improved oral hygiene and preventive techniques related with periodontal disease. In the present study, periodontal lesions accounted for 2% of cases of sinus membrane thickening associated with direct spread of pathogens to the maxillary sinus.
According to Panico and Adell17,18 development of sinusitis associated with implant placement is infrequent. Reviews published in the literature found that maxillary sinus floor augmentation prior to surgical placement of a dental implant resulted in sinus alteration in 4.17% of cases, and in inadequate implant position or implant migration in 0.92% of cases7. In the present study on a total 179 maxillary sinuses analyzed using CBCT, sinus thickening was observed in 39% of cases, 6% of which were associated with the presence of implants in close proximity to the affected maxillary sinus.
None of the cases studied here showed signs of apicoectomy. It is of note that the latter procedure can lead to a complication that is observed less frequently than expected, likely because most professionals prefer extracting the tooth rather than performing this technique in view of the associated high risk of accidental perforation to the sinus due to its proximity19. Nevertheless, reports such as that by Freedman et al. involving 472 apicoectomies, none of which resulted in sinusitis, show that there is no contraindication to performing apicoectomy in antral teeth, despite their proximity to the maxillary sinus 20.
A review of 35 articles on maxillary sinusitis of odontogenic origin showed the upper molar region to be more frequently associated with maxillary sinus alterations (47.68%). The first upper molar was the molar tooth most frequently associated with maxillary sinusitis, with a 22.51% incidence, followed by the third molar tooth (17.21%) and the second molar tooth (3.97%). With regard to the upper premolar region, it was affected in 5.96% of cases only; the second premolar was the most affected premolar tooth (1.98%), and the canine was involved in only 0.66% of cases of maxillary sinusitis of odontogenic origin7.
In keeping with the aforementioned study, the results obtained here showed that the tooth most frequently involved in sinus alteration was tooth 1.6, accounting for 33% of cases. It was significantly more affected than teeth 1.4 (0%), 1.5 (2%), 1.7 (11%), 2.4 (7%) and 2.5 (2%), but did not differ significantly compared to teeth 2.6 (30%) and 2.7 (15%).
Examination of sinus membrane thickening by cone beam computed tomography allows detecting the presence of sinus pathology. Findings must be correlated with the clinical condition of the patient. Thorough examination of the para nasal sinuses and visualization of the osteomeatal complex on axial and coronal sections obtained by computed tomography without contrast is essential to evaluate permeability of the ostium and for proper treatment planning. The retrospective nature of the present study does not allow establishing a "cause-effect" relationship between periapical pathology and changes in the maxillary sinus. Further prospective studies are necessary to correlate clinical and radiographic data and confirm the present findings. Lastly, a larger sample size and including cases classified according to disease severity could reveal more significant associations between periapical and/or periodontal pathologies and changes in the sinus mucosa.
CONCLUSION
According to the results obtained in the present study, the high incidence of sinus pathology of odontogenic origin implies the need for interdisciplinary work involving dentists and ear-throat specialists. Carious processes, poor restorations, periodontal lesions, implants, and the presence of root remnants are the main causes of sinus mucosa thickening. The use of CBCT for diagnosis and treatment planning allows identifying the presence of maxillary sinus membrane thickening and determining whether it is associated an odontogenic origin.
ACKNOWLEDGEMENTS
The authors thank Dr. Carlos Marino, Ear-throat specialist and lecturer at the Specialization in Oral-maxillofacial prostheses, University of Buenos Aires, for his valuable assistance and guidance in performing the present study, and DDS Jonathan Saiegh, from the Department of Imaging Diagnosis of the School of Dentistry of the University of Buenos Aires, for his assistance in evaluating the samples.
FUNDING
None
CORRESPONDENCE
Dr. Pablo A. Rodríguez
Cátedra de Endodoncia, Facultad de Odontología
Marcelo T. de Alvear 2142, 1°A, (C1122AAH) CABA. Argentina
pablorodriguez@dentalmedicine.com.ar
1. Clavería R, Peña M, Gutiérrez I, Paredes M, Fouces Y. Comunicación bucosinusal por extracciones dentales. Medisan 2010; 14: 346-352. URL:http://scielo.sld.cu/scielo.php?script=sci_arttext%26pid=S1029-30192010000300010%26lng=es. [ Links ]
2. Nagar AC, Gautam A. Maxillary Sinusitis of Odontogenic Origin: A Review. Int J Adv Res 2015; 3: 1323-1328. [ Links ]
3. Kilic C, Kamburoglu K, Yuksel SP, Ozen T. An Assessment of the Relationship between the Maxillary Sinus Floor and the Maxillary Posterior Teeth Root Tips Using Dental Cone-beam Computerized Tomography. Eur J Dent 2010; 4: 462-467. [ Links ]
4. Raghav M, Karjodkar FR, Sontakke S, Sansare K. Prevalence of incidental maxillary sinus pathologies in dental patients on cone-beam computed tomographic images. Contemp Clin Dent 2014; 5: 361-365. [ Links ]
5. Pérez-Piñas I, Sabaté J, Ruiz T, Jimeno L, Cueto L, Ventura J. Semiología de la patología inflamatoria nasosinusal mediante TC. Patrones de afectación. Radiología 2001; 43: 387-393. https://doi.org/10.1016/S0033-8338101i77001-4 [ Links ]
6. Cymerman JJ, Cymerman DH, O'Dwyer RS. Evaluation of odontogenic maxillary sinusitis using cone-beam computed tomography: three case reports. J Endod 2011; 37: 1465-1469. [ Links ]
7. Simuntis R, Kubilius R, Vaitkus S. Odontogenic maxillary sinusitis: a review. Stomatologija 2014; 16: 39-43. [ Links ]
8. Ferguson M. Rhinosinusitis in oral medicine and dentistry. Aust Dent J 2014; 59: 289-295. [ Links ]
9. Shanbhag S, Karnik P, Shirke P, Shanbhag V. Association between periapical lesions and maxillary sinus mucosal thickening: a retrospective cone-beam computed tomographic study. J Endod 2013; 39: 853-857. [ Links ]
10. Guerra-Pereira I, Vaz P, Faria-Almeida R, Braga AC, Felino A. CT maxillary sinus evaluation-A retrospective cohort study. Med Oral Patol Oral Cir Bucal 2015; 20: e419-26. [ Links ]
11. Khorramdel A, Shirmohammadi A, Sadighi A, et al. Association between demographic and radiographic characteristics of the schneiderian membrane and periapical and periodontal diseases using cone-beam computed tomography scanning: A retrospective study. J Dent Res Dent Clin Dent Prospects 2017; 11: 170-176. [ Links ]
12. Rak KM, Newell JD 2nd, Yakes WF, Damiano MA, Luethke JM. Paranasal sinuses on MR images of the brain: significance of mucosal thickening. AJR Am J Roentgenol 1991; 156: 381-384. [ Links ]
13. Arias-Irimia O, Barona-Dorado C, Santos-Marino JA, Martínez-Rodriguez N, Martínez-González JM. Metaanalysis of the etiology of odontogenic maxillary sinusitis. Med Oral Patol Oral Cir Bucal 2010; 15: e70-3. [ Links ]
14. García B, Martorell L, Martí E, Peñarrocha M. Periapical surgery of maxillary posterior teeth. A review of the literature. Med Oral Patol Oral Cir Bucal 2006; 11: E146-150. [ Links ]
15. Evwcombe R G., Merino Soto C. Intervalos de confianza para las estimaciones de proporciones y las diferencias entre ellas. Interdisciplinaria 2006; 23. URL:http://www.redalyc.org/articulo.oa?id=18023201 ISSN 0325-8203 [ Links ]
16. Abrahams JJ, Glassberg RM. Dental disease: a frequently unrecognized cause of maxillary sinus abnormalities? AJR Am J Roentgenol 1996; 166: 1219-1223. [ Links ]
17. Panico R, Fernandez Bodereau E, Sosa F. Dental implant migration to maxillary sinus. Treatment and complications: case report. Rev Asoc Odontol Argent. 2014; 102: 28-33. URL:https://www.aoa.org.ar/wp-content/uploads/2017/03/V101N2M2014.pdf [ Links ]
18. Adell R, Lekholm U, Rockler B, Brânemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg 1981; 1: 387-416. [ Links ]
19. García B, Martorell L, Martí E, Peñarrocha M. Periapical surgery of maxillary posterior teeth. A review of the literature. Med Oral Patol Oral Cir Bucal 2006; 11: E146-150. [ Links ]
20. Freedman A, Horowitz I. Complications after apicoectomy in maxillary premolar and molar teeth. Int J Oral Maxillofac Surg. 1999; 28: 192-194. [ Links ]














