INTRODUCTION
Composite materials are being increasingly used in dentistry. Over the years, their composition and properties have changed to meet esthetic and mechanical requirements1,2,3 . However, the greatest current challenge is still how to manage shrinkage stress, which depends on multiple factors such as polymerization shrinkage and the material's elastic modulus, which are directly related to the organic matrix and the quantity and type of filler; the speed of conversion and degree of conversion4,5 related to polymerization activation mode, and the type and quantity of initiators. These factors are directly affected by the composition of the material.6,7 Composites consist of an organic matrix, usually dimethyl acrylate, reinforced with ceramic fillers treated superficially with a vinyl-silane agent to adhere to the organic matrix and agents that promote the polymerization reaction. The base monomer, usually bis-GMA or some other diacrylate, has high molecular weight and, due to its high viscosity is mixed with other dimethyl acrylates of lower molecular weight (TEGDMA, UDMA) as diluents. It can be cured by chemical, physical or dual activation.8,9 The composite sets as a result of polymerization, when the monomer chains crosslink to produce a final thermoset structure. During this process, the intermolecular distance between monomers is reduced, causing shrinkage. Linear and volumetric shrinkage of restoration composites have ranges of 0.5% to 2.0% and 1.0% to 4.0%, respectively. Shrinkage stress is 0.5 MPa to 8 MPa, depending on variables such as inorganic filler, monomer characteristics, material insertion technique, photoactivation methods and design of the pre-paration10. During polymerization gel point, the composite's elastic modulus increases such that the dissipation or deformation capacity is reduced to compensate the shrinkage. The adhesion to the tooth wall and the shrinkage of a composite restoration generate shrinkage stress, which is transmitted to the adhesive interface or dental substrate, generating clinical problems such as marginal gap, tooth fissures and/or fractures, secondary caries, postoperative sensitivity, marginal pigmentation, etc.11-13 The activation mode, as well as the types and concentrations of initiators, regulate the degree of conversion and kinetics of the reaction14. The higher the degree of conversion, the greater the shrinkage and the elastic modulus, both of which contribute to producing greater stress. Faster polymerization rates mean that the monomers move faster than the critical conversion, causing rapid setting and at the same time reducing flowability. A higher speed of reaction is associated to faster growth in the module before and after the gel point, and translates into faster development of stress compared to what would be produced by using a slower curing regime.15,16 There are several techniques to reduce shrinkage stress, such as using fillers or liners with low elastic modulus, incremental placement of composite resins, low intensity during the initiation of photopolymerization and modification of the composition of the material. Placing a liner material with lower elastic modulus such as a flowable composite or hybrid glass ionomer enables the size of the preparation, as well as shrinkage, to be reduced. Since both these materials are more flexible, shrinkage stress transmitted to the adhesive interface and/or the tooth is reduced. However, the results of studies on flowable composite as a liner are controversial. The elastic modulus of flowable composites varies, and can sometimes be higher than that of the composites themselves. The flowable composites with lower elastic modulus reduce shrinkage stress and better results were achieved even in some resins without ceramic filler.
Several authors have shown that using a filler reduces microleakage and increases adhesion and resistance values. Aggarwal et al.17 studied marginal adaptation of composite resins with flowable composite and glass ionomer liners on third lower molars with different adhesive systems. Leevailoj et al. 18 evaluated marginal microleakage in class II restorations with high-viscosity composites (packable) with and without flowable composite liners in natural teeth. Montes et al. 19, evaluated bond strength of restorations with flowable composite with adhesives with or without ceramic fillers in bovine teeth. However, other studies report that using fillers has no beneficial effect on the margin of the material and the dentin due to the low content of filler and high polymerization shrinkage, e.g., the papers by Braga, Choi, Kwon and Caldenaro20-23.
There are many studies on glass ionomer related to reduction of shrinkage stress. Bryant et al.24 evaluated shrinkage of different types of glass ionomers and composite resins, finding that the shrinkage of glass ionomers is comparable to that of composites: about 2% to 3% in the long term without contact with moisture. Chutinan et al.25 evaluated glass ionomers under conditions of moisture, reporting that as from 56 days, glass ionomers undergo expansion. Feilzer et al.26 evaluated the influence of water sorption on shrinkage stress in resin-modified glass ionomer cements. Although the material initially shrinks after the setting reaction, subsequent hygroscopic expansion of the glass ionomer due to conditions of moisture and according to time positions it better compared to flowable composites, in agreement with the conclusions reported by Kemp-Scholte27 and Tolidis28. Competition between addition polymerization and the acid-base reaction of the resin-modified glass ionomers may affect the dimensional change of the material and its capacity to dissipate shrinkage stress, as suggested in the papers by Berzins, Kakaboura and Young29-31.
In order to contribute to knowledge on this topic, the aim of this study was to assess the effect of using a layer of flowable composite or hybrid glass ionomer on shrinkage stress of a composite for restoration.
MATERIALS AND METHODS
We used a nanofilled composite (FXT) (Filtek Z350 XT A2 from 3M), a resin-modified glass ionomer (VGI) (Vitrebond Light Cure Glass Ionomer from 3M) and a Flowable Composite (FFR) (Filtek Z350 XT Flowable Restorative A2 from 3M ESPE). The light-curing unit was a tungsten quartz lamp (XL-3000, 3M/ESPE).
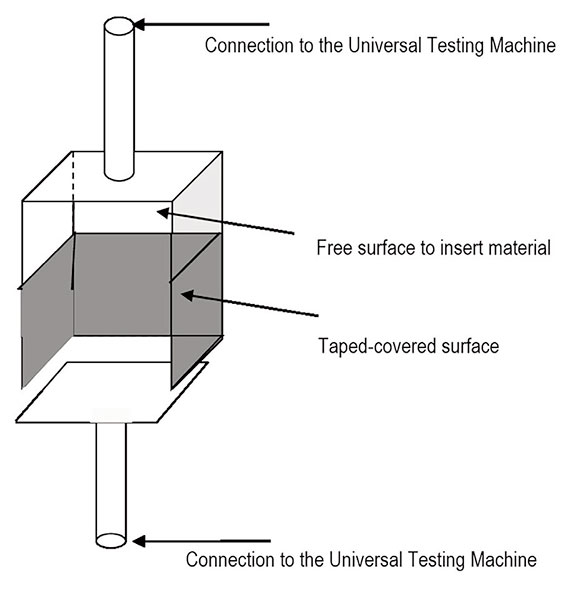
We made metal boxes in which 4 of the sides were attached to each other. The top side was welded to a metal rod 4 mm in diameter. The bottom side was not attached to the rest of the box, but welded to another metal rod 4 mm in diameter (see Figures 1 and 2). Its edges were polished to enable it to slide freely through the box. The back surface was divided into two areas: one of 9 mm2 on which to place the material, and the rest covered in paper tape. Composite was inserted through the open side. The opposite side was called floor, and its surface area was 20.25 mm 2. The metal rods were used to connect the pieces to a universal mechanical testing machine (INSTRON 1011, Instron Corporation, Japan). Before using the boxes, we sandblasted them with aluminum oxide 50 pm in diameter using a Bio-Art microblaster for 10 s from a distance of 2 cm with air pressure 7 bar (102.5 psi). Then we washed them with distilled water in a Teslab® tb02 ultrasonic cleaner for 1 min at a power of 80 W and a frequency of 40 kHz, and dried them with air from a triple syringe.
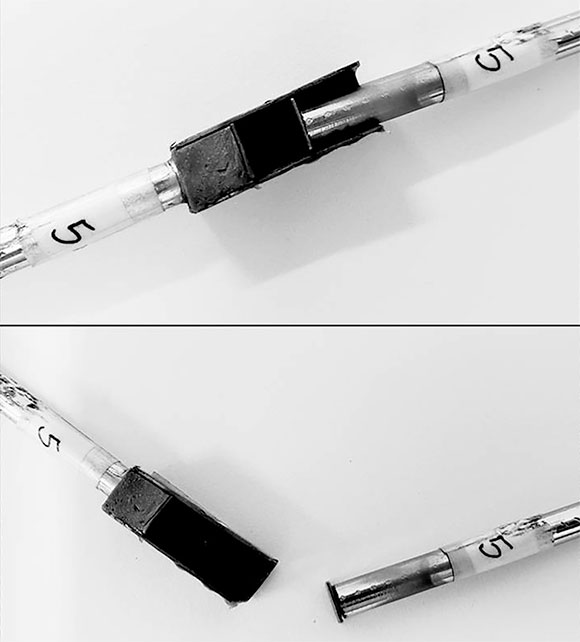
Fig. 2 Devices used to evaluate shrinkage stress; assembled (top) and disassembled (bottom). The two ends were connected to the universal mechanical testing machine.
We prepared three groups of 5 metal boxes: Group 1 (control group), filled with FXT; Group 2 (G.I.) lined with a resin-modified glass ionomer VGI and filled with FXT; and Group 3 (or Flowable) lined with FFR and filled with FXT.
For all three groups, each box was filled with 67.8 mg of composite, weighed with an OHAUS® Analytical Standard precision balance. The contact surface area was 56.25 mm2 in all three groups. In Group 2, the Centrix system was used to line the boxes with a layer 1 mm thick of VGI, which was cured according to the manufacturer's instructions. Immediately, the composite Filtek Z350 XT A2 (3M) was applied in a horizontal layer 2 mm thick, in contact with all five sides of the box, and cured for 40 s. The same was done for FFR. All assays were performed by a single operator.
The boxes were mounted on the testing machine such that the free-moving side was attached to the 0.5 kN load cell - adjusted in a 50N full scale - (the base of the free area was situated towards the floor of the box), while the rest of the box was attached to the base of the machine. The force values generated by polymerization were recorded every 10 s in newtons and converted to stress values (in kilopascals) according to contact surface area. Each procedure was recorded with a video camera and a digital chronometer from the beginning of composite activation with the lamp for 60 s (40 s photoactivation and 20 s post-curing).
The videos were used to record force values every 10 s for the fifteen tests performed. The results and the values converted to stress were analyzed statistically by ANOVA for repeated measurements and Tukey's test.
RESULTS
Table 1 shows mean and standard deviation (kPa) for the maximum stress values recorded for each group and evaluation time. Figure 3 shows mean stress values recorded for each group according to time. The ANOVA test, in linear and quadratic function, showed statistically significant differences (p<0.05) according to material. Comparison of means using Tukey's test showed statistically significant differences between the control group (restorative material only) and the other two groups (p<0.01), but there was no significant difference between glass ionomer and flowable composite (Groups 2 and 3). Analysis of confidence intervals established that there was no statistically significant difference at the first evaluation time (10 seconds), but in the Control Group, shrinkage stress increased significantly as from 20 s compared to the groups with flowable composite or glass ionomer liners, with no difference between the latter two. This behavior is clearly visible in Figure 3, which shows that Groups 2 and 3 behave similarly, while in the Control Group, the stress generated increases progressively.
DISCUSSION
This study evaluated stress from the time of polymerization until 20 s post-curing, for the composite and for composite with a liner. It did not evaluate the individual behavior of each base or liner material, although their elastic modulus and stress are known to increase hours and even days after they have completely set1.
It has been suggested that placing a liner with lower elastic modulus between the composite restoration and the substrate, used together with other precautions, may reduce the shrinkage stress18,19. Flowable composites and resin-modified glass ionomer are used as liners, but their use is still controversial according to results published to date. Because resin-modified glass ionomers (RMGIs) have fewer monomers that polymerize and therefore less shrinkage than composites, their use has long been suggested for reducing stress14,24-26. Kemp-Scholte & Davidson report that polymerization shrinkage stress was relieved by 20% to 50% as a result of the various flexible liner materials such as glass ionomer 27. Tolidis K et al. also report that RMGIs liners reduce shrinkage stress. RMGIs set more gradually and slowly than resins, up to 48 h later, with better stress dissipation28. Bryant & Mahler report that at 30 min, the volumetric shrinkage of both conventional and hybrid ionomers is very similar to that of composites 24. If shrinkage is similar, it may be deduced that stress would be similar, although our study found significant differences with and without liners, but no significant difference in stress relief for glass ionomer compared to flowable composite.
The competition between the acid-base reaction and addition polymerization can modify final structure and stress-dissipating ability. The two types of setting inhibit each other, i.e., if addition polymerization is activated, the rate and extent of the acid-base reaction is inhibited. Similarly, the polymerization reaction is affected by the polar nature of the ionomer medium, and as ionomer opacity increases as a result of acid-base neutralization, physical activation by light is attenuated29. It has been shown that the efficiency of curing decreases when it is applied after 20 min,30 even though this situation is clinically quite unlikely to occur. But if activation is delayed by 3 min and 15 s, there will only be 85% polymerization compared to immediate activation.
RMGIs are susceptible to water uptake and release 27. The movement of water may occur while the material sets under sealed conditions as a base or liner. Two chemical reactions have been reported. One is the intrinsic use of water during initial setting and the other is extrinsic water sorption by the acid-base reaction 31. In the model applied herein, where RMGIs are used as bases or liners in metal boxes, there is no extrinsic water effect, and therefore the material shrinks. This could explain why no difference was found between glass ionomer and flowable composite.
According to Braga RR, Ferracane JL & Hilton TJ20, flowable resins produce similar stress levels to composites. Most flowable composites do not produce significant stress reduction when used under composites 20 and there are even studies that report an increase in stress with flowable composite or RMGI liners21-23. Volumetric shrinkage and elastic modulus are inversely related and depend on the material's ceramic filler. Composites with high ceramic load have less organic matrix, and therefore less shrinkage due to the formation of crosslinked polymer chains, but in turn, they prevent elastic deformation for dissipating stress due to the high rigidity of the ceramic filler. A flowable composite follows these theories, but is a more fluid material due to the addition of monomers of smaller molecular size, and would theoretically have greater volumetric shrinkage. In turn, there are flowable composites with high ceramic loads which dissipate less stress due to their high elastic modulus. Thus, they do not dissipate stress due to the change in mechanical properties of the material. It would be helpful to know to what extent the final stress is caused by the quantity and size of organic molecules and the elastic modulus of the composite when it has set.
The current study used metal boxes in a moisture-free environment. The boxes were sandblasted to increase micromechanical adhesion of the materials by applying a model similar to the one used by Pires-de-Souza et al.32, with the difference that they used glass rods instead of metal boxes, mounted in the same way to the testing machine to record data. It should be noted that the substrate and adhesion are unlike the clinical situation. However, the design enables the behavior of materials and combinations to be evaluated, beyond the variables involved in the clinical situation. It would be interesting to ascertain the influence of the stress caused by each of them and the effect of the final resulting stress with the composite until the material hardens completely.