INTRODUCTION
Coronavirus disease (COVID-19) has emerged as the largest global pandemic and has already affected several countries, including Brazil 1 . Even though the disease sometimes appears as an asymptomatic or symptomatic clinical condition 2 , the diagnosis is most commonly associated with fever, dry cough, fatigue and difficulty in breathing 3 . COVID-19 can progress to other serious conditions with severe respiratory symptoms, including dyspnea and pneumonia, which can lead to death 4 , 5 .
Although the mortality associated with COVID-19 is low, it has high spreading potential6 and high levels of transmissibility 6-8 . It spreads mainly from person to person through contact transmission, including oral, nasal and eye membrane contact; or direct transmission, including sneezing, coughing and droplet inhalation 9 . Droplets containing the virus can settle on surfaces, where the virus can remain viable for days, causing significant concern among healthcare professionals and support services, including dental professionals 10 .
Dental care settings consistently involve the risk of COVID-19 infection due to the specificity of the procedures conducted in them. Dental professionals are constantly exposed to pathogenic microorganisms, including viruses and bacteria 11 . The exposure to saliva and blood, the use of sharp instruments, and the droplets and aerosols generated during dental treatment can contaminate instruments and environmental surfaces in dental practice, or infect the professional directly 12-14 .
The American Dental Association (ADA) recently issued guidance to prevent infection in the COVID-19 pandemic during emergency and nonemergency dental procedures 15 . Infection control in dental practice includes the use ofPersonal Protective Equipment (PPE), and cleaning and disinfecting the dental care environment as part of the clinical routine needed to prevent cross-infection 16 .
The available information on how dentists should work during the COVID-19 pandemic is very helpful in preventing infections. However, this information refers to urgent and emergency procedures or dental procedures in general, but does not provide more specific explanations on actions required for each specialty, e.g., endodontics. Thus, the aim of this study is to evaluate, through the application of a questionnaire, the impact of COVID-19 on endodontic treatment routine among Brazilian dentists, including possible changes in the technique and/or in preventive measures.
MATERIALS AND METHODS
The institutional Research Ethics Committee approvedthis study (CAAE: 31064820.6.0000.5052). Participants who accepted to take part in the survey signed an informed consent form (ICF) online.
This was a cross-sectional study using an online questionnaire with a convenience sample. The questionnaire design, pilot study and strategies for enrolling dentists were previously discussed, and it was decided that a convenience sample enrolled using social media would be valid to acquire a large number of respondents. The questionnaire was posted on the Google Forms platform, where it was available for one week, after which it was closed.
Respondents had to be dentists who regularly performed endodontic procedures in clinical practice (there was no need to be a specialist in endodontics). The submission was considered only when the ‘submit’ button was clicked at the end of the questionnaire.
This study was conducted from May 2 to May 6, 2020. The questionnaire was distributed by email as well as being posted on several social media platforms, such as Facebook and WhatsApp. It comprised 20 closed-ended questions designed to collect information about practical modifications established against the COVID-19 outbreak during endodontic treatment to protect professionals and patients (Fig. 1).
The questionnaire was divided into two sections. The first section recorded personal data such as age, sex, years’ experience in dental practice, area of residence, and professional setting (private or public) of dental practice. The second section included questions about dentists’ perception and behavior regarding endodontic treatment during the COVID-19 pandemic. For data analysis, we considered minimal PPE before COVID-19 pandemic to be the use of gloves, surgical masks, protective eyewear, surgical caps, gowns or lab coats. During the pandemic, minimal PPE includes gloves, N95 masks, protective eyewear, surgical caps, disposable gowns or lab coats, and shoe covers. After responding to the questionnaire, respondents were requested to provide their registration number in the Regional Council of Dentistry (RCD) to prevent duplication of data.
Data were collected and analysed by SPSS 25.0 for Windows (IBM corp., SPSS, Inc., Chicago, IL, USA). Descriptive statistics were performed, and chi-square and Fisher’s exact tests were used to test the significance of possible associations. The level of significance was 5% (p < 0.05).
RESULTS
A total 1105 questionnaires were answered from all of Brazil’s 25 states. Mean respondent age was 37.79±10.35 years. Female respondents accounted for 66.2% (732) and male 33.8% (373) of the total. Regarding time elapsed since graduation in dentistry, 44.2% (488) of respondents graduated in the last 10 years, 30% (332) graduated between 11 and 20 years ago, and 25.8% (285) graduated more than 20 years ago.
The percentage of respondents by regions of Brazil was 263 (23.8%) from the south, 335 (30.3%) from the south-east, 406 (36.7%) from the north-east, 54 (4.9%) from the mid-west and 47 (4.3%) from the north. Regarding clinical practice, most respondents worked only in private practice (72.5%), whilst 5.7% worked exclusively in public practice, and 21.8% worked in public and private practice (Table 1).
Ninety-seven respondents (8.8%) had already tested positive for COVID-19 or had been in direct contact with someone who tested positive. A total 1011 (91.5%) respondents identify the high risk of COVID-19 infection to dentists, while 1073 (97.1%) recognise the need to change some clinical practices in endodontic treatment due to the pandemic.
Most respondents (60.1%) are partially following social isolation. At the time the questionnaire was applied, 777 (70.3%) of respondents believed that Brazil would have a lower or similar number of COVID-19 infected people in comparison to the most affected countries, while 328 (29.7%) believed that Brazil would be one of the most severely affected countries in the world.
When asked if during the COVID-19 pandemic they would change the PPE used during dental appointments, 1073 (97.1%) answered affirmatively. Table 2 shows the use of minimal adequate PPE before and during the pandemic period, and how it differed according to respondent background characteristics.

Table 2 Association between the respondents’ demographic and professional characteristics and the use of adequate PPE before and during the COVID-19 pandemic.
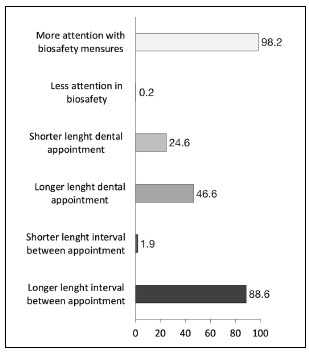
Fig. 2 illustrates the changes in endodontic cavity access during the pandemic. Most respondents (75.93%) agree that the use of a rubber dam before cavity access preparation diminishes the risk of virus dissemination. Most participants (56.83%) said that they would still use the high-speed handpiece during COVID-19 pandemic for cavity access preparation. Other changes in endodontic appointments were also considered in the survey, including greater attention to biosafety measures, duration of dental appointments, and duration of intervals between appointments (Fig. 3).

Fig. 2 Professional choices regarding cavity access preparation before and during the COVID-19 pandemic
DISCUSSION
Since the beginning of the pandemic, other studies have aimed at measuring the impact of the disease on dental professionals. However, ours is the first study to emphasize the need for changes in endodontic practice. Surveys using questionnaires are a popular method for determining the views of a sample of healthcare professionals or patients 17 .
Genetic and epidemiological research has found that the COVID-19 outbreak began with the transmission of the virus from animal to human, followed by the spread from human to human 18 , 19 . Further studies have demonstrated that not only is the virus transmitted by symptomatic patients, but also by asymptomatic persons or even those in the incubation phase 18 , 20 , 21 . This difficulty of identifying whether or not individuals have the virus makes the regulation of disease transmission extremely challenging. This has led to the constant recommendation for people to practice social isolation as much as possible during the pandemic period. However, in China, the demand for urgent dental treatment decreased by only 38% during the pandemic period 22 , reflecting the fact that urgent dental services will always be essential, making it difficult for dental care providers to practice social isolation. In addition, the interruption of dental care during this period puts pressure on the emergency departments at hospitals, which are already dealing with the pandemic 23 .
Although at this point Brazil is an epicenter of coronavirus infection, the present study was conducted from May 2 to May 6, 2020, when Brazil only had 90,000 cases of COVID-19 and 6,000 confirmed deaths. The information from the survey showed that most dentists were not in total social isolation, and were still performing different types of procedures, although the ADA (American Dental Association) had recommended that dentists should postpone elective treatments to avoid contact, focusing only on urgent and emergency care 24 .
It has been suggested that dental professionals are at higher risk for COVID-19 infection than any other professional 11 , requiring strategies to prevent infection, including pre-exposure and post-exposure prophylaxis. The results of the present study demonstrated that dental professionals are aware of this, with most respondents (91.5%) identifying the high risk of COVID-19 infection to dentists, and 97.1% saying they would change the PPE used during dental appointments during the pandemic. In fact, considering the severity of the COVID-19 pandemic, and in the light of the strong commitment of several dental associations, it is essential to provide simple, clear guidelines for managing dental patients and protecting dentists against risks 25 .
COVID-19 transmission can be expected via contact with droplets and aerosols generated during dental clinical procedures 26 . The guidelines recommended for dentists and dental staff by the Centers for Disease Control and Prevention (CDC), the ADA and the World Health Organization (WHO) to control the spread of COVID-19 include PPE, hand washing, detailed patient evaluation, rubber dam isolation, mouthwash before dental procedures, and disinfection of every exposed surface 27 .
Our results showed that before the pandemic, more than 80% of dental professionals used adequate PPE. The use of adequate PPE was more frequent among women, reiterating the concept that women tend to be more careful. This is somehow expected, since in general, women get less sick, suffer fewer accidents and die later because they are more careful and prevent more than men do. However, this association has not been demonstrated considering the pandemic period only, because it is still too recent.
Even though more than 97% of the respondents are aware of the need to change the PPE they use during the pandemic, at the time the survey was carried out, less than 30% of respondents said they used adequate PPE. Single respondents seem to be less worried than married respondents about using appropriate PPE during the pandemic, possibly because they usually live alone and worry less about other family members to whom they could transmit the disease if they became infected. We also found that the percentage of professionals using adequate PPE is higher in the southern and central-western Brazilian regions. It is interesting to note that at the moment, these areas present the lowest number of COVID-19 infected people.
It has already been recognized that the use of highvolume saliva ejectors could reduce the production of droplets and aerosols in dental procedures, thereby protecting dentists from infection. Furthermore, face shields and protective eyewear are essential whenever high- or low-speed drilling are used. The use of rubber dam isolation reduces the generation of droplets and aerosol mixed with patient saliva and/or blood in 1 m diameter of the surgical field by 70% 28 . Opportunely, the current study showed that 75.93% of respondents consider that rubber dam isolation before endodontic access cavity reduces the risk of virus transmission. In addition, the use of a highspeed handpiece with water-cooling to perform the access cavity was seen as a concern. Some of the respondents intend to change the technique during endodontic procedure, using low-speed handpiece or discarding the use of water-cooling. However, the use of high speed without water-cooling is not recommended, and in these cases, the damage to dental structure should also be considered.
Nearly all participants believe that biosafety in dental practice during the pandemic should receive more attention. This seems to be a consequence of extensive media coverage regarding the need to reinforce hygiene methods such as constant handwashing, use of a mask, coughing into a bent elbow, and keeping a distance, among others 29 . Almost half the respondents believe that longer dental appointments are one the changes that should be implemented in clinical practice during the COVID-19 pandemic. Even though there is no published data regarding the adequate length of dental appointments, it seems reasonable to believe that longer dental appointments may allow the dental professional to better complete the endodontic procedures, avoiding repeated contact with the patients on different days. Moreover, it has been recommended that the interval between dental appointments should last long enough for possible contagious droplets to stop floating in the air and settle on the surfaces for subsequent disinfection of the entire dental office and replacement of all PPE30. In the current study, almost 90% of respondents believe that the interval between dental appointments should be longer during the pandemic, which is in agreement with the recommendations.
The effects of COVID-19 are becoming worse day by day. As dentistry is at the top of professions at risk of contamination, many dentists are anxious and afraid to work. The general population, however, still demands emergency and non-emergency dental services. It is therefore essential that dentists should have appropriate guidelines for the protection of both parties. Several points can and should be analyzed regarding dental practice during the COVID-19 pandemic. Considering the high level of risk to which dentists are exposed, it is crucial that clearer and more detailed protocols should be developed so that professionals know how to act to prevent the virus from spreading. This risk can be reduced if dentists act appropriately in all specialties and when performing any type of procedure.
In conclusion, dentists who perform endodontic treatment still need to be able to identify the best arrangements for performing their procedures safely during COVID-19 pandemic. Specific guidelines require detailed information for each specialty and its procedures.