INTRODUCTION
Molar Incisor Hypomineralization (MIH) is defined as a qualitative enamel developmental defect, presumably multifactorial in origin, characterized by demarcated opacities in one to four first permanent molars (FPMs), with or without involvement of permanent incisors (PI). In weak and porous FPMs, enamel rapidly progresses to post-eruptive breakdown (PEB) and caries1-3. Reports have shown that second primary molars (SPMs), mineralized at a similar time as the FPMs, can also be affected, with the condition defined as Hypomineralized Second Primary Molar (HSPM)4.
The global prevalence of MIH has been estimated as 11.24% to 14.2%, despite the wide variability in prevalence studies that highlighted the need for standardized procedures and clinical assessment in order to reduce the heterogeneity. South America has been identified as the most affected region, with an estimated prevalence of 18%5,6. A systematic review and meta-regression analysis estimated MIH prevalent cases and incident cases in countries with no database. In Venezuela, prevalent cases were estimated at 4,120,887 in 2015, and incident cases were estimated at 86,782 in 2016 7. In 2019, an MIH index was tested, providing confidence as a reliable and valid instrument for use in population-based studies, and it was recommended to determine MIH prevalence in epidemiological research 8.
Only three studies have reported demarcated opacities in Venezuelan children (local school population and renal disease group) using DDE and mDDE Index from 2010 to 2018 9-11. To our knowledge, no research has been conducted following standardized procedures and using EAPD criteria to determine MIH prevalence in Venezuela’s pediatric population. The aim of this study was to determine the prevalence and distribution of MIH and HSPM in children who received dental care at two health services (one public and one private) in Caracas Metropolitan Area, Venezuela, and to compare the results with global epidemiological data.
MATERIAL AND METHODS
Study population
A cross-sectional prospective study was conducted on 6- to 12-year-old children who received care at the School of Dentistry at Universidad Central de Venezuela or at a private dental care center, from May 2019 to March 2020. The classification of health sectors was based on a previous report12. The study was designed according to the checklist described in a systematic review of MIH prevalence studies in order to ensure proper quality5. Sample size was calculated using the formula: sample size (n) = [Z2 × P (1-P)]/d2, where Z is the statistical level of confidence [95% confidence interval (CI) > Z = 1.96], and P is the expected prevalence and d the precision13, assuming 18% for expected prevalence and 7.5% as precision level. Twenty percent was added to the minimum sample to account for possible negative responses. The calculated sample size was 121 patients. All positive respondents were included in the total sample (n). A stratified randomized sample (n1) was calculated according to the size of each health sector group (positive respondents from the public and private sectors), using percentages and considering strong limitations in the previous randomized procedure, especially in the public sector. No official data is available about fluoride consumption level in salt or water.
The initial and final ethical approvals were secured from the Bioethics Committee, School of Dentistry, Universidad Central de Venezuela (CB-091-2019/ CB-133-2020). Parents or legal guardians signed informed consent before the clinical evaluation. Pursuant to national regulations, children also needed to assent to their participation in the study. Inclusion criteria were children seeking dental care (no general anesthesia or sedation required) with all first permanent molars fully erupted. Exclusion criteria were children using fixed orthodontic appliances, with special needs, disabilities, or contagious infectious diseases.
Clinical assessment
A valid and reliable instrument for MIH-index scoring was used for clinical evaluation8,14 (Table 1). Index teeth were FPMs, PI and SPMs.
All patients were examined while seated in a dental chair by a calibrated examiner, using a dental light source and a flat mirror number 5. The examiner adhered to standard infection control protocol, using single vision lenses +2.5. Subjects were positioned to receive maximum illumination. Before examination, all teeth were cleaned and dried with gauze. The evaluation of index teeth was initiated in the right maxillary region (Quadrant 1), followed by the left maxillary index teeth (Quadrant 2), then the mandibular arch, beginning with the most posterior index tooth in the left quadrant (Quadrant 3), and finally moved around to the last index tooth in the right mandibular quadrant (Quadrant 4). A sequential code registration was carried out in a written form. Severity was classified as mild (Codes 21 and 22) or severe (Codes 3, 4, 5 and 6).
Calibration exercise
A pediatric dentist was calibrated in EAPD diagnosis criteria for the MIH index, using clinical photographs collected from patients who had previously been examined for the presence/absence of tooth developmental defects of enamel and following the MIH training manual for clinical field surveys and practice14. Three calibration sessions for clinical status were held. Intra-examiner reliability Kappa value was 0.878 and Inter-examiner reliability Kappa value was 0.831.
Statistical analyses
Data were collected and tabulated using Microsoft Excel 2010 (Microsoft Corp., Washington, USA) and analyzed using Statistical Package for Social Sciences version 20 for Windows (SPSS Inc., Chicago, IL, USA) software. The MIH group included cases with codes 2, 3, 4, 5 or 6 in at least one FPM. The NOMIH group included cases without codes 2, 3, 4, 5 or 6 in at least one FPM. The prevalence of MIH/HSPM was calculated by frequencies, confidence interval (95%). Descriptive statistics were used to calculate frequency of affectation in index teeth. The chisquare test was used for association between MIH or HSPM and sex. The odds ratio (OR) was calculated to quantify the risk of presenting MIH according to presence of HSPM. The HSPM group included cases with codes 2, 3, 4, 5 or 6 in at least one SPM. The NO-HSPM group included cases without codes 2, 3, 4, 5 or 6 in at least one SPM. Adjusted SPM samples were made according to dental age (for total and randomized stratified sample), cases with no possible evaluation of all SPMs were excluded from the HSPM group. Cases in the MIH group with at least one affected SPM were included, although in some cases it was not possible to evaluate all SPMs. To calculate the number of MIH-affected teeth, affected SPMs were not considered, affected PIs were included. To calculate the number of HSPMaffected teeth, FPMs affected were not considered. The Mann Whitney U-test was used to evaluate the association between number of affected teeth and sex. Severity was calculated with respect to the total cases included in MIH and HSPM groups and to the total number of affected teeth in the MIH and HSPM groups, respectively. For this research, in case of a tooth with severe and mild presentation on different surfaces, the most severe form was considered and tabulated. Four dental groups were included in the analyses of the most affected tooth: FPM group (first permanent molars group), UPI group (upper permanent incisor group), LPI (lower permanent incisor group), SPM group (second primary molar group). Percentages were calculated with respect to the number of teeth evaluated in each group.
RESULTS
Sample distribution, MIH/HSPM prevalence and Odds Ratio.
One hundred and forty five 6- to 12-year-old children seeking dental care were invited and accepted to participate in this study. Three children were excluded according to selection criteria. The total sample (n=142) was distributed as follows: 80 children (56.33%) from a private center and 62 children (43.67%) from a public center. Of the total sample, 65 children (45.78%) were male and 77 (54.22%) female. Average age of the total sample was 8.85 ±1.63 years. A randomized stratified sample was calculated using SPSS® program according to health sector group size and the minimum sample size previously determined (n1=121). Of the randomized stratified sample, 56 children (46.28%) were male and 65 (53.72%) female. Average age of the randomized stratified sample was 8.83 ± 1.61. MIH prevalence was 25.35% (n=36) (CI 95%= 18.11%-32.59%) for the total sample, and 25.62% (n=31) (CI 95%=17.73%-33.51%) for randomized stratified sample. Regarding health sector groups, 68 (56%) children were examined in the private sector and 53 (44%) children in the public sector for the randomized stratified sample. MIH prevalence was 30.88% in the private sector (n=21) (CI 95%= 19.62%-42.15%) and 18.87% in the public sector (n=10) (CI 95%= 7.98%-29.76%), Chi square p-value= 0.133 for randomized stratified sample.
One hundred and ten children were included in the SPM total sample: 47 (42.73%) were male and 63 (57.27%) female. Average of age was 8.38±1.44 for the SPM total sample, and 8.35±1.41 for the SPM randomized stratified sample. Ninety-four children were included in the SPM randomized stratified sample: 42 (44.68%) were male and 52 (55.32%) were female. HSPM prevalence was 18% (n=20) (CI 95%= 11%-26%) for the SPM total sample and 20% (n=19) (CI 95%= 12%-28%) for the SPM randomized stratified sample. The co-occurrence of MIH and HSPM was 25.80% (n=8) in the stratified randomized sample. The Odds Ratio used to calculate the risk of presenting MIH according to presence of HSPM was 2.86 (CI 95% = 1.04-7.87) for the SPM total sample and 2.48 (CI 95%= 0.86- 7.15) for the SPM randomized stratified sample.
Distribution in the MIH group
The distribution of MIH prevalence according to sex was determined using the Chi square test with 5% significance level (Table 2). Severity was determined according to the total cases included in the MIH group and the total number of affected teeth in the MIH group (Table 3). Mild cases represented 78.2% of the cases in the stratified randomized sample and 77.5% in total sample. The number of affected teeth in each dental group for both MIH samples was calculated (Table 4). The upper left FPM, central right UPI and lateral right LPI were the most affected teeth. For the stratified randomized sample, average affected upper/lower teeth was 67.7%/58% for the FPM group. Average affected right/left teeth was 34.5%/27.6% for the UPI group and 26.4%/ 16% for the LPI group. Average affected teeth in the MIH group of the total sample was 4.19 ±2.17 and 4.16 ± 2.19 for stratified randomized sample. Girls had higher number of affected teeth than boys; U Mann Whitney p-value=0.947 for stratified randomized sample and p-value= 1.000 for total sample. Of the 31 children with MIH included in stratified randomized sample, 5 (16.1%) patients also presented hypomineralization defect (Code 14), 3 (9.6%) patients showed diffuse opacities (Code 11) and only 1 patient (3.2%) presented both (Codes 11 and 14).
Distribution in the HSPM group
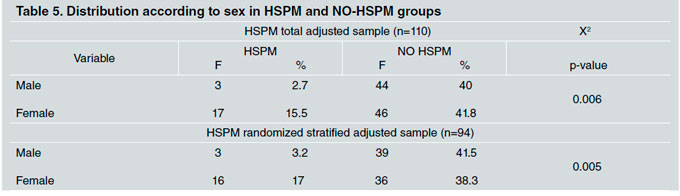
The distribution of HSPM prevalence according to sex was determined using Chi square test results with 5% significance (Table 5). Severity according to the total cases included in the HSPM group and to the total number of affected teeth in the HSPM group was determined (Table 6). Mild cases represented 69.8% of cases in the stratified randomized sample and 68.8% in the total sample. The number of affected teeth for both SPM samples was calculated. The upper right SPM was the most affected tooth (55.5%). For the HSPM randomized sample, average affected upper/lower teeth was 51.4%/45% for the HSPM group and 48.3%/42.4% for the HSPM total sample
Average affected teeth in the HSPM group of the SPM total sample was 1.65 ±0.74 and 1.68 ± 0.74 for the SPM randomized sample. Girls had a higher number of affected teeth than boys; U Mann Whitney test p-value=0.903 for stratified randomized sample and p-value=0.816 for the SPM total sample.
DISCUSSION
A prevalence of MIH of 25.62% was determined in a random sample of 6- to 12-year-old children who received dental care in Caracas Metropolitan Area. The number reported here is higher than the estimated prevalence for South America (18%)6. It is very difficult to make comparisons of epidemiological interest between studies on MIH prevalence. Reports vary widely depending on population age, instrument, index used (DDE, mDDE, EAPD criteria), researcher calibration, evaluation technique and the setting, severity classification, research objectives and associated studies with other variables such as systemic conditions, etiological factors or dental caries.
Considering studies in which subjects were examined in a dental chair, MIH prevalence of 17.8% was found in a group of Spanish children using transillumination technique for dental surface evaluation15. A study conducted in private dental offices and university hospitals (specialized in pediatric dentistry) in eight regions of Japan reported a global prevalence of 19.8% 16. In Latin America, a study conducted in a dental chair setting on Argentinean children determined MIH prevalence of 15.9% with significant differences according to health sector (private sector: 24.40% and public sector: 6.4%)17. Similar results were reported for Uruguayan children with MIH prevalence of 12.3% (private sector: 26.99% and public sector: 7.13%)18. These authors suggested that differences between health sectors could be attributed to local factors related to access to dental healthcare.
The prevalence reported in the current study is higher, but similar to previously reported prevalence for private sectors in Argentina and Uruguay. Also in this report, MIH prevalence in the private sector is higher than in public sector, but without significant difference. These findings suggest that comorbidities and complications associated to MIH lead parents to seek private services, considering that retreatments are often required, and the great demand for public services due to the economic crisis in Venezuela.
Clinical assessment conducted at schools may result in underestimation of positive cases because of limited viewing conditions, such as patient and operator position, or inappropriate light source. Some studies on Latin American schoolchildren have reported MIH prevalence of 40.4% in Mexico, 40.2%-18.4% in Brazil and 15.8% in Chile19-22.
Also, 12.3% MIH prevalence was reported in schoolchildren in Brazil, but only opacities greater than 2 mm were recorded (outdoor setting) so there may have been underestimation23. Recently, Colombian schoolchildren were evaluated using portable dental equipment, with artificial light, and MIH prevalence was determined to be 11.2%24. This wide variability in results and assessment highlights the need for standardized procedures, considering that opacities greater than 1 mm should be recorded14.
Regarding sex, significant difference in MIH prevalence has been found between Venezuelan girls and boys. Although systematic reviews had not determined this difference6,7, prevalence studies from Jordan and Iran have reported similar results25,26. In the current report, girls are more affected than boys, but the number of affected teeth does not differ significantly according to sex.
Clearly, MIH is more frequent in first permanent molars than in permanent incisors, with reports of molar involvement of 68.5%-58.9% in Argentina and 59.58% in a multicenter study in Argentina and Uruguay17,27. Those numbers are similar to our findings with an average of 67.7% for upper FPM and 56.45% for lower FPM. Small but significant differences have been previously reported between percentages of maxillary and mandibular affected teeth in Argentina28. Fortunately, the defect is mildly expressed in most cases, and severely affected teeth have been determined with values of 14.8% enamel breakdown and 9.1% atypical restorations in Brazilian schoolchildren23; 15% in Colombia (including cases of opacities with loss of structure, atypical restorations, and/or exodontia due to hypomineralization)24, and 21.8% of loss of enamel in affected teeth in Argentina17. Findings in the current study also suggest that MIH can be found simultaneously with demarcated opacities in premolars and canines, and/or diffuse opacities compatible with dental fluorosis. The co-occurrence of MIH and dental fluorosis has also been reported recently in schoolchildren in Brazil29.
In this study, a 20% prevalence of HSPM was determined in a random and adjusted (to dental age) sample of 6- to 12-year-old children who received dental care in Caracas Metropolitan Area, with significant difference between sexes, girls being more affected than boys. The prevalence of HSPM is highly variable worldwide and has been reported between 2.7% and 21.8% 30. The result found in the current study is within this range. The odds ratio determined in this study was 2.48, lower than previously reported between 4.6 and 4.44,31. However, it is still relevant for pediatric dentists, so that they can provide current information to parents or guardians and promote adequate follow-up.
Finally, the current study was conducted in dental chair setting, and prevalence observed in this setting could be higher than prevalence in the general population. MIH produces associated comorbidities such as dental hypersensitivity, caries lesions, frequent loss of restorations, aesthetic complaint and affectation of self-esteem and self-image, which are frequent reasons for consultation. Thus, these results must be properly interpreted and used as a reference for similar dental healthcare services.
Limitations
A recent publication has emphasized that the Venezuelan economic crisis has shattered the healthcare system and basic public services, threatening health in the country32. Strong limitations were faced during this investigation related to conditions in public service and general living conditions. Also, by national legislation, informed consent must be signed by a legal guardian and two witnesses, after the proper information has been provided by the researcher. It was therefore not considered feasible to perform a study in a school setting. Furthermore, the COVID-19 pandemic forced us to stop collecting data, though fortunately, the minimum sample size had been reached by March 2020 and the number of positive respondents enabled random selection.
CONCLUSIONS
The prevalence of MIH in 6- to 12-year-old Venezuelan children who received dental care in Caracas Metropolitan Area was higher than global prevalence and previously estimated prevalence for South America, with a predominance of mild affectation, and more frequent in upper molars. These results have major similarities with reports from Argentina, Uruguay and Brazil, and emphasize the significant number of children affected in Latin America.