INTRODUCTION
There has been great technological progress in implantology in recent years. The search for functional and aesthetic results has fostered the development of techniques and materials with high aesthetics and biodynamic performance 1 .
In this context, research on infrastructures using metal-free materials has increased significantly, concomitantly with the advancement of digital dentistry 1 2 . Digital systems for planning and clinical execution have become increasingly frequent in the dental routine 1-4 .
Among the digital systems, CAD/CAM (computer-aided design/computer-aided manufacturing) enables planning and execution with the aid of a computer, facilitating the introduction of zirconia (Zr)-based ceramics in implant dentistry 1-4 .
Zr is a material with aesthetic properties of high resistance and good health relationship with peri-implant tissues 2 3 . In addition, CAD/CAM enables automation and standardizaron of the manufacturing process of prosthetic infrastructures, thereby making it possible to manufacture prostheses with high-quality adaptation in a short time 1 . However, the high strength of a Zr-based infrastructure can generate wear when adapted directly to the prosthetic platform of osseointegrated implants 4-6 . It is therefore recommended to use a titanium base (TiBase) between the Zr and the implant 6 7 , especially when the implant is functional 6, 8-11 .
Thus, TiBases that fit the prosthetic platforms of the implants are made with a coronary portion suitable for receiving Zr infrastructures (Zr copings). After being made, the Zr copings are cemented to the TiBase abutment, and the set is fixed to the osseointegrated implant 6-8 . However, there are currently several types of dental cements with different indications and characteristics, raising questions about which cement is the most appropriate and has the best retention and stability 9 . Resin and ionomeric cements have been indicated as materials with high retention and resistance index in the aging process 7, 10-13 , and are therefore indicated for the cementation of Zr copings on the TiBase abutments due to their adhesion and mechanical resistance 7 14 . Although adhesion characteristics between TiBase abutments and various restorative materials have been reported 13-15 , it has not yet been well established which type of cement is the most suitable for cementing Zr copings on TiBase abutments, and especially their stability over time and the temperature changes that occur in the oral environment.
The aim of the present study was therefore to evaluate the tensile strength of Zr copings cemented on TiBase abutments with resin-modified glass ionomer cement and various resin cements after thermocycling. The following null hypotheses were tested: (1) there is no difference in tensile strength between the different cements tested, and (2) thermocycling did not influence the tensile strength values of the Zr copings cemented on the TiBase abutments.
MATERIALS AND METHODS
Experimental design
Forty-two samples were selected, composed of the set: Strong SW® Cone Morse implant (S.I.N, Sao Paulo SP, Brazil), TiBase abutment (Duotech® S.I.N, Sao Paulo SP, Brasil). The set was fixed on a steel base to receive the threads of the type of implant used.
For each TiBase abutment, a Zr coping was manufactured in a standardized manner using a CAD/CAM system, 6 mm in height and 6 mm in thickness. The coping was manufactured in a cylindrical shape, with an indentation of 4 mm in thickness and 2 mm in height towards the abutment, thus enabling adaptation of the traction device support in this region 14 15 .
The samples (n = 42) were randomly distributed according to the two study variables: 1) cementing agent: (resin-modified glass ionomer cement [RelyX Luting 2], self-adhesive resin cement [RelyX U200], and self-curing resin cement [Multilink N]); and 2) Thermocycling: without thermocycling (after 24 h of cementation), with thermocycling.
The abutments were digitalized using a bench scanner (inEos X5, Dentsply Sirona, Sao Paulo, SP, Brazil), and the coping project was designed (CAD software inLab, Dentsply Sirona) 15 .
The thickness of the cement film was designed to be 40 pm, except at the margins, which were designed to achieve total sealing to the abutment 1 16 .
Surface treatment and cementation
After milling, all Zr copings underwent a blasting process with 50 pm aluminum oxide (Al2O3) particles at a pressure of 1.0 bar for 10 s 17 . The coping was fixed and manually blasted at an angle of 45° and a distance of 3 cm from the jet firing point. Then the copings were washed ultrasonically with distilled water for 180 s, cleaned in 96% ethanol, and dried with an air jet.
After blasting, all copings were subjected to the surface treatment recommended by the cement manufacturer (Table 1). Subsequently, the cement was manipulated, inserted into the coping, and manually fixed to the TiBase. Initially, digital pressure was applied, and excess cement was removed. Then each sample was subjected to a constant pressure of 20 N in the center of the occlusal surface for 10 min 16-19 .
Photopolymerization followed the time recommended by the cement manufacturer (Table 1) and was carried out with a high-intensity LED light device at 1200 mW/cm 2 (VALO Cordless, Indaiatuba, SP, Brazil). A radiometer (Demetron L.E.D, Radiometer, Kerr Sybron Dental Specialties, Middleton, WI, USA) was used to check the light intensity for each of the five specimens.
The specimens were stored in distilled water at 37°C for 24 h. Half the specimens in each group (n = 7) were subjected to 5,000 cycles of thermocycling in water baths, at temperatures of 5°C, 37°C, and 55°C, with residence times of 30 s and rest times of15 s 14 .
Tensile test
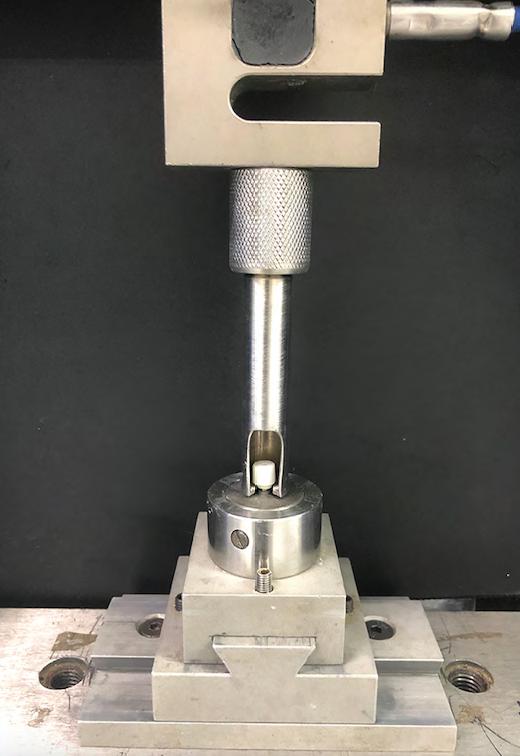
The tensile test was performed on a universal testing machine (EMIC DL 2000, Paraná, Brazil) at a speed of 1 mm/min until cementation failure or screw fracture occurred.
A load cell of 5000 N was used, in which a steel device was fixed for traction with a retention area for fitting the specimen (Fig. 1). The maximum force used at the time of the cementation failure (T) was recorded in newton (N) 14 15 .
After the test, the specimens were analyzed according to the location of the cement residue in each component 16 , using an optical microscope (SZH-131, Olympus Ltd., Tokyo, Japan) at a magnification of 10x.
The type of failure was classified as: adhesive failure between the Zr surface and the cement; mixed failure, when there was a failure in both interfaces (between the cement and the Zr and between the cement and the TiBase); or fracture of the screw (when the screw fractured before cement failure).
Statistical analysis
After verifying the normality of the data (Shapiro Wilk, p > 0.05), all data were analyzed using two-way analysis of variance (cementing agent and thermocycling). The Tukey post hoc test was used to compare between pairs in all analyses. The effect of size was calculated using eta squared (p2) for the independent variables.
Statistical analysis was performed using IBM SPSS Statistics for Windows v.26 (IBM., Armonk, NY, USA). Statistical tests were performed considering a 5% significance level.
RESULTS
Analysis of tensile bond strength
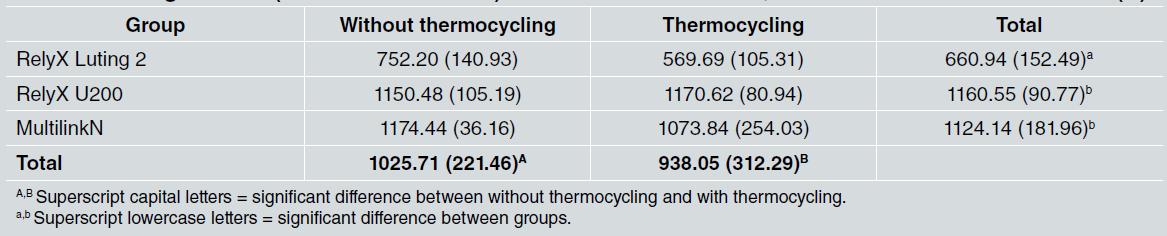
The mean values (standard deviation) demonstrated that the type of cement significantly influenced the recorded tensile load (p < 0.001) (Table 2). The glass ionomer (RelyX Luting 2) showed the lowest value of tensile load (p < 0.05), whereas the resin cements (RelyX U200 and MultilinkN) did not show a statistically significant difference (p > 0.05).
Influence of temperature change on tensile bond strength of cement
The interaction between the cements and thermocycling was significant (p = 0.163). When subjected to temperature changes (thermocycling), a reduction in the mean values of cement tensile strength (95% confidence interval) was observed (p = 0.047). The effect size was 0.760 for the cement type, and 0.105 for the thermocycling variable, i.e., thermocycling was responsible for approximately 10% of the bond strength variation, and the cement type was responsible for 76% (Fig. 2).
Failure analysis after the tensile test
When cementation was performed with RelyX Luting 2, the failures were predominantly adhesive, between the Zr coping and the cement (85.7%). RelyX U200 presented failures predominantly due to screw fracture (85.7%), with a minimum number of adhesive failures between the Zr coping and cement (14.3%). In MultilinkN, all samples that were not thermocycled showed failures due to screw fracture (100%), while in the group that underwent thermocycling 28.5% were adhesive failures between the Zr coping and cement (Fig. 3).
DISCUSSION
The results of tensile strength and longevity of the Zr coping cementation on the TiBase abutment found in this study are important to guide clinicians in choosing the type of cementation material. The results showed that the glass ionomer cement promoted lower tensile strength values than the resin cements, leading to the rejection of the first proposed nuil hypothesis. Another result was the significant decrease in tensile strength after thermocycling for the cements used, leading us to reject the second null hypothesis.
Resin cements are known to promote higher values of tensile strength than glass ionomer cements 19 . Resin cements have high shear strength to resist the internal forces that can cause the structure of the material to slide against itself. At the same time, they can withstand tensile forces, enabling the hydrophobic matrix of a composite cement to adhere to hydrophilic substrates 20 . Thus, better behavior of resin cement is also observed when Zr copings are cemented on TiBase abutments 8 , reaching higher levels of retention force.
Comparison of the tensile bond strength values of resin cements showed averages of 1160.55 and 1124.14 N respectively for the RelyX U200 and MultilinkN cements, and 660.94 N for the ionomer (RelyX Luting 2). Resin cements are composed of resinous monomers that provide adequate chemical adhesion as well as micromechanical adhesion to dental and metallic structures when compared to resin-modified glass ionomer cement 19 . Moreover, there is consensus in the literature that treating the Zr surface with ceramic primers can promote better adhesion of the organic particles of the cement with
the inorganic particles of Zr 13-22 . This may explain the higher values of the retention forces for the resin cements tested in relation to the glass ionomer cement modified by resin.
Another aspect is the surface treatment of Zr. Hansen et al. 21 evaluated the importance of preparing Zr with jets of AL2O3 before cementation. Different authors have concluded that the use of Zr surface treatment significantly increases the quality of retention after cementation 7 8 23 24 . However, other studies have shown that abrasive air particles with AL2O3 can cause damage to the surface of Zr, causing flaws and microcracks, compromising the mechanical strength of Zr 25 26 .
The literature also reports that a lack of application of adhesive systems between Zr structures and resin cements could decrease the bond strength of Zr structures on implants 8 10 12 . However, the increase in adhesion can only be improved by using surface treatments such as blasting, silanization, and use of adhesives next to resin cements containing phosphate groups 26 . The resin cements used in this study include phosphate groups in their composition, which together with the surface treatment could explain the better performance ofboth resin cements. The high holding force could also be the result of using a titanium abutment with retentive areas. The pillar used in this study had areas of roughness, which possibly guaranteed greater mechanical interlocking with cement. In fact, Güngor et al. 14 used smooth abutments for cementing Zr structures and concluded that thermocycling added to the mechanical cyclic load and resulted in a significant decrease in tensile strength
Another aspect studied was the effect of aging by thermocycling. Thermocycling is well accepted as a form of aging, since in addition to hydrolytic degradation promoted by water, temperature changes, repeated expansion/contraction, and other stresses within a sample have a significant impact on tensile strength 27 .
In this study, the average retention for the tested cements was 1025.71 N for the groups without thermocycling and 938.05 N for the thermocycled groups, showing a significant decrease. In the individual analysis, the effect of thermocycling was found to be less on resin cements than on the resin-modified glass ionomer cement . Saleh et al. 26 also used thermocycling for aging and found that resin cements are more resistant than other types of cements to its effects and maintain the integrity of the cement line.
Among the causes of this decrease are increased sorption and solubility, and less interaction with organic components. The absence of a resinous monomer in this type of cement can aggravate the low resistance to aging processes, fostering a weak connection between the cement and the Zr structure. This could also have promoted an increase in adhesive-type failures in this group . However, in resin cement, although thermocycling decreased the values of tensile strength, this did not promote a significant difference. This may be due to the use of adhesive systems that, in addition to the surface alteration of Zr with AL2O3 blasting, made the adhesion more stable even after an aging process, as shown in Figure 2 in the confidence interval line 15 28 . In the analysis of the type of failure, it was found that for the resin cements, the failures were predominantly of the screw fracture type (82.1%), while with the use of glass ionomer cement, 28.5% of the failures were of the adhesive type between the Zr coping and cement. The increase in retentive strength in the groups where resin cements were used caused the predominance of failures due to screw fractures. The region most susceptible to fracture of the pillar screw is located at the junction between the threads and the neck 29 , and it was in this region where all fractures occurred in this experiment. Studies report that this type of fracture can be minimized by using thicker screws and with an apical indexer that helps in the stabilization of the prosthetic component 30 .
Another feature that could have caused an increase in such failures is the thickness of the cement film. In the present work, it was standardized at 40 gm for all samples. According to the literature, when thicknesses of up to a maximum of 60 gm are used, better results are obtained in tensile strength tests 8 10 . This thickness of cement film, added with a retentive titanium pillar, probably caused the high retentive force.
Malthazan et al 8 tested two resinous cementing agents, finding the best retention rates with preconditioning of the coping and application of a ceramic primer. The maximum average observed in one of the groups in their study was 598.6 N, using a smooth titanium pillar 7.8 mm high and 3.4 mm wide and a 30 gm cementation space.
Although studies have evaluated different materials for cementing Zr structures on TiBase abutments 7 11 12 14 21 , the cementation step is important to ensure the stability and longevity of the implant-supported prosthesis system, and the lack of a predictable protocol for cementation of Zr copings on TiBase abutments is still a limitation in this area. The results in this study will help the appropriate choice of cement for zirconia restorations on zirconia or TiBase abutments.
The methodology used in this study endeavored to simulate what is performed clinically in a standardized way, but the clinical condition of each patient can influence the final outcome and longevity of the restorations. It is known that in vitro studies provide limited information regarding the clinical performance of Zr copings on TiBase abutments; therefore, randomized clinical trials that show real clinical situations of the behavior of these cements in the oral cavity have yet to be conducted.
In conclusion, resin cement has better adhesive stability when cementing the Zr coping to the TiBase abutment. Thermocycling decreases the retentive strength of resin-modified ionomer cement.