INTRODUCTION
Early detection of furcation involvement (FI) favors treatment success, preventing the progression of alveolar bone loss and loosening ofteeth 1 , 2 . Periodontal diagnosis of furcation involvement is based on clinical, radiographic and intra-surgical probing of the furcation entrance. Although intra-surgical measurement is invasive, it has been considered the gold standard for classifying the extent of furcation involvement, especially in upper molars 3 . Despite its accuracy for FI diagnosis, intra-surgical measurement should only be used in specific cases, while the conservative approach (clinical and radiographic examinations) can be routinely performed 4 .
Periapical, interproximal and panoramic radiographs have been widely used as complementary examinations for periodontal disease diagnosis, primarily due to their easy acquisition, low cost and satisfactory resolution 5 , 6 . Even though intraoral radiographs are still the most frequently used technique for diagnosing FI 7 , they are often not precise, because two-dimensional radiographs may show overlapping roots, making it challenging to evaluate furcation lesions correctly 8 , 9 .
Due to the limitations of conventional radiographs, cone-beam computed tomography (CBCT) has been indicated for the diagnosis of FI, since it provides detailed information about periodontal tissue support and interradicular bone, which are fundamental components for treatment planning 10 , 11 . It is worth using CBCT in FI diagnosis in upper molars when surgical treatment is indicated 2 . CBCT is highly accurate for detecting furcation involvement, and has been extensively used for challenging diagnoses, such as Degree I or II 12 , 13 .
In vivo studies 3 , 5 10 14 15 have shown the potential of 3D images compared to intra-surgical assessments for diagnosing FI in maxillary molars, but results are controversial regarding CBCT accuracy for this purpose. The aim of this study was therefore to compare CBCT images with clinical and intra-surgical analyses to diagnose maxillary molar furcation involvement.
MATERIALS AND METHODS
This was a prospective cross-sectional study, performed in full accordance with the World Medical Association Declaration of Helsinki and approved by the Institutional Review Board of Federal University of Goiás, Brazil (#67419517.4.0000.5083) and University Center of Anápolis (#2.126.098). It was also registered by ReBEC (Brazillian Register for Clinical Trials - #RBR-33mj49). This study followed the CONSORT guidelines for clinical trials.
To calculate the sample size, 83% mean agreement was considered, as previously reported 3 , 5 , performed at a significance level of 95%, for a test power of 80%, two-tailed. A number of 41 sites per analyzed group was determined. The following inclusion criteria were established: patients older than 18 years, with periodontitis in the upper molar indicated for surgical treatment. Exclusion criteria were teeth with caries, cervical resorption, fused roots, metallic crowns, amalgam restorations close to the alveolar bone crest and endodontic treatment; pregnant and/ or lactating women. The study group was comprised of 12 patients (8 men and 4 women), aged 40 to 55 years and diagnosed with periodontitis. A total 40 teeth, 120 sites, with or without FI, were included. Patients received prior periodontal therapy, including oral hygiene instructions, scaling and root planing, and occlusal adjustment when necessary. The same periodontist performed examination and treatment for all patients.
Clinical measurements
The sites were classified according to the presence or absence of FI, and horizontal and vertical bone loss were measured. Horizontal bone loss was assessed with Nabers probe (PQ2N, Hu-Friedy, Chicago, IL, USA) on the distal, buccal and mesial sites, according to the classification system of Hamp et al. (1975) 16 . Vertical bone loss was evaluated with the North Carolina probe (PCPUNC-15, Hu-Friedy, Chicago, IL, USA), measuring the distance from cementoenamel junction (CEJ) and the bottom of the periodontal pocket at the center of the buccal surface 17 . The examiner had no access to the CBCT images.
Intra-surgical measurements
Intra-surgical evaluation (ISE) was considered the gold standard and was performed using the same parameters described previously ( Fig. 1 ). During ISE, the periodontist had no access to the previous clinical measurements or the CBCT images.
Image acquisition and analysis
All CBCT images were acquired with an i-CAT Cone Beam 3D Imaging System-Next Generation (Imaging Sciences International, PA, USA) device using the same parameters: voxel size 0.125 mm3, tube setting 120 kV (voltage) and 5 mA (current), acquisition time 26.9s, and an 8 x 8 cm field of view (FOV). InVivo Dental Application software (Anatomage 5.3.2, USA) was used for CBCT image analysis.
Three previously calibrated radiologists performed the tomographic measurements. All the images were independently analyzed twice by each observer, with an interval of 2 weeks between the analyses.
The observers had no access to the clinical and intra-surgical evaluations. Horizontal and vertical bone loss were measured in the slice that showed the greatest extension of FI ( Fig. 2 ). Vertical measurements were performed in the sagittal plane by positioning the cursor at the beginning of the FI and extending it to the defect’s maximum point (Fig 2D).
Statistical analysis
Cohen’s Kappa test (k) was used to establish presence or absence of FI and horizontal bone loss. An Intraclass Correlation Coefficient (ICC) was used to analyze the intra- and inter-observer agreement in the tomographic measurements for vertical bone loss. For the Kappa test, the fohowing interpretation was considered: k < 0.20, poor; k = 0.21-0.40, fair; k = 0.41-0.60, moderate; k = 0.61 - 0.80, good and k = 0.81 - 1.00, very good 18 . For the ICC interpretation, Bland and Altman’s reference19was used: ICC < 0.4, small; 0.4 < ICC < 0.75, moderate and ICC > 0.75, excellent.
Clinical and CBCT measurements (horizontal and vertical) were compared using the Wilcoxon test, which was also used to compare them to the gold standard (intra-surgical measurements). McNemar’s test was used to compare the groups regarding the presence or absence of furcation involvement. Accuracy, sensitivity, specificity, positive and negative predictive values were calculated for the detection of furcation lesions.
evaluated sites, according to different methods of assessment
RESULTS
Distribution of FI
The horizontal FI recorded in the clinical, CBCT and intra-surgical evaluations are shown in Table 1. The intra-surgical findings revealed Degree I (21 sites), II (15 sites) and III (15 sites), while 69 sites showed no FI (57.5%). The clinical findings presented 28 Degree I, 25 Degree II, and 8 Degree III lesions and 59 sites without FI (49.2%). The CBCT findings showed 6 Degree I, 16 Degree II, and 12 Degree III lesions and 86 sites showed no FI (71.7%).
Diagnostic tests for clinical and CBCT assessment
Diagnostic tests for the detection of FI are shown in Table 2. Accuracy for clinical detection was 75%, while for CBCT evaluation it ranged from 72.5% to 77.5%, considering the 3 observers.

Table 2 Accuracy, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) for the identification of furcation lesion
Sensitivity was higher for CBCT (92.7%) than for clinical evaluation (72%), while specificity was lower for CBCT (45.1-56.9%) than for clinical detection of FI (78.8%).
Intra- and inter-observer agreement on CBCT images
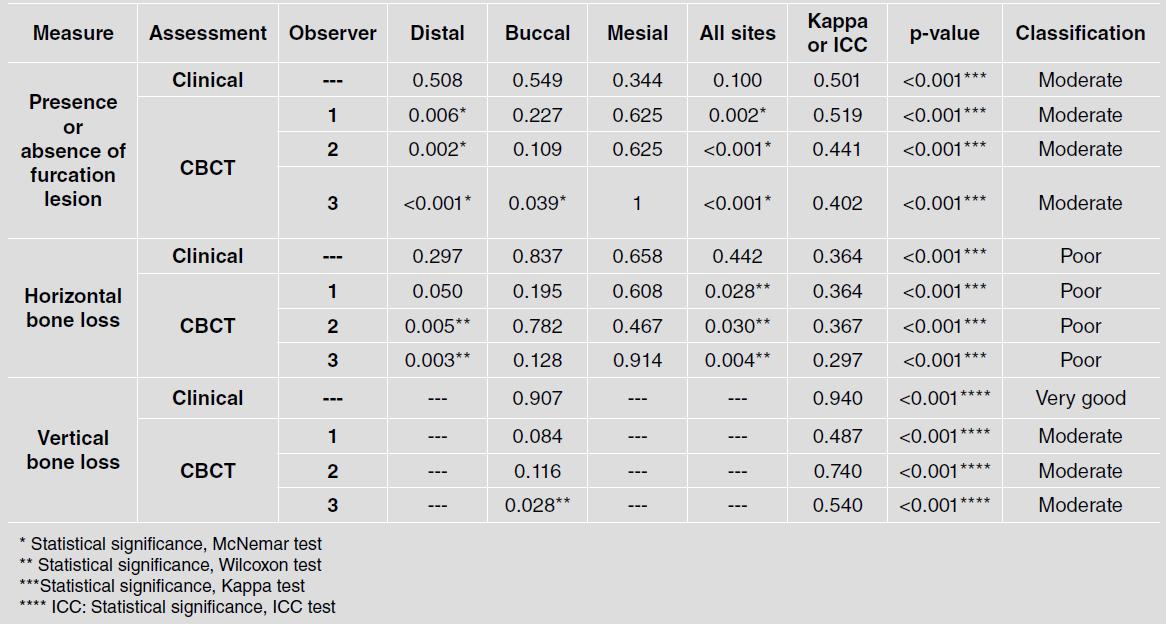
Intra- and inter-observer agreement for the presence or absence of FI and horizontal bone loss are shown in Table 3 and those for the vertical bone loss in Table 4.

Table 3 Intra- and interobserver agreement for the presence or absence of furcation lesion and horizontal bone loss
For vertical bone loss, both intra-observer agreement (ICC=0.916) and inter-observer (ICC=0.965) agreement were considered excellent. Regarding the presence or absence of FI, intra-observer agreement was very good (k=1.000) and inter-observer agreement was good (k=0.773). Horizontal bone loss showed moderate (k=0.485) to very good (k=1.000) intra-observer agreement and moderate (k=0.549) to good (k=0.625) inter-observer agreement.
Comparison and agreement of clinical, CBCT and Intra-surgical assessment
Table 5 shows statistically significant results for the comparison and agreement tests between the clinical and CBCT data measurements and intra-surgical evaluations for all variables: presence or absence of FI and horizontal and vertical bone loss.
Comparing clinical and ISE, there was a significant difference between presence and absence of FI with moderate (k=0.501) and poor (k=0.442) agreement, respectively, for horizontal bone loss and very good (k=0.940) agreement for vertical bone loss (p<0.05). Comparing CBCT to ISE, there was a significant difference for the presence or absence of FI on CBCT to distal sites with moderate agreement for all assessments (p<0.05). Horizontal bone loss showed poor agreement with CBCT assessment (p<0.05).
DISCUSSION
Our results showed that neither clinical evaluation nor CBCT presented high agreement with the gold standard (intra surgical evaluation - ISE). Accuracy values for FI detection were below 80%, which indicates that caution is required when prescribing and interpreting CBCT exams for this purpose. Other studies have reported high precision for CBCT for detection of FI 2 , 20 . Our study’s accuracy results may be related to a sample of incipient furcation lesions, which are difficult to diagnose, even in imaging exams. In a previous study, Yusof et al. 14 found no difference between clinical and intra-surgical evaluation; however, they evaluated molars (both upper and lower) with extensive bone losses. In another study 15 , CBCT measurements showed high agreement with ISE in evaluating incipient furcation defects, as in the present study, but assessment was made by a single observer, and a larger FOV was employed. It is essential to mention that these variations in the agreement (greater or lesser) between CBCT and ISE in these studies may occur due to changes in the parameters of the CBCT devices (such as FOV, voxel size, voltage), as has been shown in a recent study by Rinne et al. 21 .
In the present study, the descriptive analysis concerning presence of FI showed a 14.2% underestimation by CBCT. Similar results were found in other clinical studies 3 , 5 10 . Clinical assessment overestimated presence of FI in 11.96% of the cases, showing superior results compared to CBCT. Our results differed from Darby et al. 1 , who found in clinical assessments an overestimation of 58% of FI and an underestimation of 20% of FI compared to CBCT.
The findings of the intra-observer agreement for the presence and absence of FI and horizontal bone loss were considered very good. These results were better than those reported in a previous in vitro study by Kolsuz et al. 22 , who found good agreement. It is important to emphasize that in vivo studies present difficulties related to soft tissue and anatomical variations 7 . This makes our results surprisingly better than those of in vitro studies in which these limitations are not present 8 , 23 .
For horizontal bone loss, the good and moderate interobserver agreement supports the notion that observers have difficulty in classifying FI compared to detecting presence or absence of the defect. Other clinical studies 2 , 20 24 did not report the results of the interobserver agreement on CBCT, so we could not compare our findings.
There was no statistically significant difference regarding intra-observer agreement for vertical bone loss; however, inter-observer agreement was excellent. These results show the validity and reproducibility of CBCT in monitoring the height of the bone defect at the buccal surface of teeth with vertical bone loss.
As observed in this study, the distal site was diagnosed better (p<0.05) than the buccal and mesial sites. These results corroborate Walter et al. 2 , who found a greater diagnostic precision at the distal site. Similar results were also described by Qiao et al. 20 , who reported significant agreement in the diagnosis of FI by ISE. Moreover, the study by Zhang et al. 25 , CBCT showed more significant agreement in the detection of distal sites by clinical evaluation, while in the recent study by Komsic, et al. 15 , the buccal site was better diagnosed than the distal and mesial sites.
In the present study, the general agreement of CBCT with intra-surgical assessment for the FI involvement was moderate (k: 0.519) and poor (k: 0.367) for horizontal bone loss. These results show that for the classification of bone loss, the statistical error of the method could have been relatively high. On the other hand, better results were found in the clinical studies by Qiao et al. 20 and Walter et al. 2 , with very good agreement between CBCT and intra-surgical assessment, while Yusof et al. 14 reported excellent agreement. Remarkably, these studies had samples with extensive FI, especially Degrees II and III, while in the present study, much of the sample consisted of incipient defects. In the early stages of FI, the cavities are small and have irregular borders, making them difficult to diagnose by CBCT 26 . Moderate agreement was found upon comparing CBCT and ISE for vertical bone loss for all observers (p <0.05). Qiao et al. 20 reported only the difference of 0.36 mm between the measurements, but not the agreement result. Padmanabhan et al.8evaluated 25 furcation defects in lower molars, using a pachymeter for the evaluation of vertical bone loss, and found a difference of only 0.12 mm by CBCT compared to ISE. The differences found in those studies are small compared to the present study, and both showed statistically significant differences 8 , 20 . However, Yusof et al. 14 did not find statistically significant differences between CBCT and ISE measurements for vertical bone loss.
In our study, accuracy results for FI identification were similar for clinical assessment and CBCT evaluation by all three observers. Interestingly, despite the similar results, a statistical difference was found upon comparing clinical assessment and CBCT by McNemar’s test. This can be clearly understood by the sensitivity and specificity findings individually. In the clinical evaluation, all diagnostic test results presented a balanced ratio between sensitivity (72%) and specificity (78.8%), which resulted in a 75% accuracy value. Contrarily, CBCT accuracy for all observers was defined by high sensitivity compensation combined with low specificity. This implies that CBCT showed a high performance in detecting the presence of FI (92.7% sensitivity) but was not as useful to exclude false positive cases. These findings should be taken into consideration when indicating and interpreting a CBCT exam for this purpose.
According to the meta-analysis published by Haas et al. 27 , although there is moderate scientific evidence supporting the use of CBCT to assess furcation lesions and FI, it should not be considered the first choice. Other systematic reviews 28 , 29 corroborate this analysis, stating that CBCT should be indicated for selected cases, considering a risk-benefit balance. These researchers agree with Yang et al. 30 on that, depending on the types of periodontal bone defects, CBCT is not necessary since clinical assessment is sufficient for detecting and classifying these lesions. Another critical issue to be highlighted is that different CBCT settings and devices may influence image accuracy for FI detection 21 , 31 32 , and a small field of view should be preferred 28 .
In summary, clinical, CBCT and intra-surgical measurements showed similar results in assessing maxillary molar furcation involvement. Regarding horizontal and vertical bone loss analyses, CBCT was not found to be an accurate method for incipient lesions. For the diagnosis of incipient furcation lesions, clinical evaluation remains fundamental. The indication of CBCT should be made considering the radiation dose evaluation and the real benefits for diagnosis of the furcation involvement.