INTRODUCTION
Surgical procedure to remove impacted or embedded third molars can limit masticatory function and cause, albeit temporarily, severe pain and discomfort 1, 2 . Specific therapeutic altematives have been studied as adjuvants of drugs in controlling pain, swelling and other undesirable postoperative complications. Low-level laser therapy (LLLT) has proven to be effective in reducing postoperative discomfort because of its analgesic, anti-inflammatory and tissue biomodulation effects 2-4 .
Three biological effects produced by LLLT have been described: primary effects, classified as biochemical, bioelectric and bioenergetic, which stimulate the production of cellular ATP, causing mitotic acceleration; secondary or indirect effects, with increased blood flow and lymphatic drainage, which interfere with the body’s inflammatory response; and general therapeutic effects, such as activation of the immune system 1-5 .
There is extensive literature on the benefits of LLLT, including several controlled, randomized studies that evaluate the efficacy of a low-level laser compared to a placebo for the reduction of pain, swelling, and trismus after the removal of lower third molars 1-4 . On the other hand, certain studies that evaluated pain, swelling and trismus after removing lower third molars found no statistically significant difference between the use of LLLT and conventional drug therapy 6, 7 .
There are different protocols for using LLLT and various study designs for evaluation, and there is still no consensus on the best application method 1-4 . The aim of this study was to test the efficacy of two low-level laser protocols by evaluating pain control, swelling and trismus in the postoperative period of lower third molar surgeries.
MATERIALS AND METHODS
The study project was approved by the Ethical Review Board of Federal University of Goias (#68615217.0.0000.5083). The Declaration of Helsinki on medical protocol and ethics was followed. Patients were only included in the research after signing the institution-approved Free and Informed Consent Form as a means of guaranteeing confidentiality and presenting the risks and benefits of their participation in the research, and having been informed about the entire procedure they would follow.
A randomized, crossover, double-blind clinical trial was performed among patients who received care at the oral surgery service of the School of Dentistry at the Federal University of Goiás (FO-UFG). The inclusion criteria were good general and oral health, and bilaterally impacted lower third molars indicated for extraction with the same classification according to the Pell and Gregory (1933) classification in terms of impaction, and to Winter’s (1926) classification in terms of angulation. Exclusion criteria were systemic diseases; using drugs that could interfere with the inflammatory process, pain and healing; infection or pathologies involving the regions of teeth 38 and 48; being allergic to standardized medication; smokers and alcoholics; pregnant or lactating women, and patients who did not follow postoperative recommendations or needed therapeutic supplementation in the postoperative period beyond that recommended for the study. Out of 28 patients selected, seven were excluded, 2 for not consenting to participate and 5 for not following the established guidelines. The final study sample consisted of 21 patients and 42 study sites.
A different protocol was applied on each side of the mouth of each patient:
PROTOCOL A - The LLLT was applied at three different times: immediately after the surgical procedure, and 24 and 48 hours after the surgery. There were four intraoral application points: one on the alveolus, and one each on the buccal, distal and lingual surfaces of the alveolus, 1 cm away from the surgical wound (Fig. 1A). There were 8 points on the face: one pre-auricular point, four points on the Masseter muscle, two submandibular points on lymph nodes and one retromandibular point (Fig. 1B).

Fig. 1 A- points of application of intraoral laser therapy; B- points of application of extraoral LLLT.
PROTOCOL B - When performed on the opposite side, the LLLT was applied in the same way but in one session only immediately after the surgical procedure. Device modulation was identical for both intraoral and extraoral applications. To maintain the reliability of the study, the 24- and 48-hour sessions were performed in the same way, including sound emission, but without laser activation (placebo). Patients were allocated by simple randomization according to order of arrival in a chart randomly numbered from 0 to 9, with each number appearing in the same quantity. Patients numbered from 0 to 4 were first allocated to Protocol A, while patients numbered frorn 5 to 9 first received Protocol B. The patient’s right side was always treated first, and the left side received the other protocol. Initial information, such as patient identification, classification of the radiographic positioning of the tooth, facial measurements and mouth opening range were recorded on a specific chart (T0).
To determine swelling and trismus, initial face measurements and mouth opening were collected before (T0) and after surgery. All measurements were taken using a pachymeter (Mitutoyo®, Mitutoyo, Suzano, Brazil). Swelling was measured by means of a simple average of three facial measurements: from the medial canthal ligament to the angle of the mandible, from the tragus to the labial commissure and from the tragus to the menton point (Fig. 2). The range of mouth opening was determined by measuring the mesio-incisal angle of the upper and lower incisors as reference points, measured in millimeters.
The extractions were performed by the same surgeon, thereby standardizing the surgical technique, as well as the anesthetic solution and technique. All patients received a postoperative prescription of Nimesulide 100 mg every 12 hours and Paracetamol 750 mg every 6 hours for two days. They were instructed that the analgesic medication could be taken at a longer time interval if they experienced no pain or mild discomfort. Conversely, if the pain was very intense, this time interval could be safely reduced, and the analgesic could be taken every 4 hours. The quantity and periodicity of analgesic pills taken each day were noted when each patient returned. The surgical procedures on the right and left sides were performed at different times, with a 15-day interval, so that there was no bias in the evaluations, particularly in terms of the range of mouth opening. For the laser therapy protocol, a gallium-aluminum-arsenide laser device (Thera Laser, DMC Brasil®, continuous wave, 0.4 mm sized point) was used, with the tip of the device positioned on a surface of intact skin, cleaned by using dry air before application. The applications were performed by an oral and maxillofacial surgeon qualified to perform the procedure, who applied Protocol A on one side of the patient’s face and Protocol B on the other. The locations of laser exposure and device modulation were the same for both protocols. For intraoral application, the following technical parameters were used: 660 nm (red), 5 J/cm 2 dose, t 10 s, P 20 mW, E 1.2 J per point. For the extraoral application, device modulation was 780 nm (infra-red), 30 J/cm 2 dose, t 20 s/point, P 60 mW, E 1.2 J per point. Postoperative evaluations were performed by an evaluator blinded to the type of protocol used, and undertaken immediately after the surgical procedure (T1), 24 hours after (T2), 48 hours afterward (T3) and on the seventh day (T4) after the surgical procedure, for both sides. The chart used for each assessment contained the same information as the initial chart (T0), plus information on the need for analgesic medication and how frequently it was taken. The Visual Analogue Scale (VAS), validated by Katz and Melzack 8 , was used to assess postoperative pain.
The data were treated by SPSS Statistics Version 24 (SPSS Inc., Chicago, USA). The following tests were used: the Shapiro Wilk test to assess the normality of the data, the Levene test for homogeneity of variance, and the ANOVA repeated measures to assess trismus and swelling. The data for postoperative pain and quantity of analgesics used were non-parametric with non-normal distribution, so the Wilcoxon test was used. A significance level of 5% was adopted for all tests.
RESULTS
Table 1 shows the distribution of the patients by sex and the characteristics of the positioning of the 3rd molars.

Table 1 Descriptive data of the sample in terms of sex and positioning of teeth 38 and 48 (n= 42 third molars)
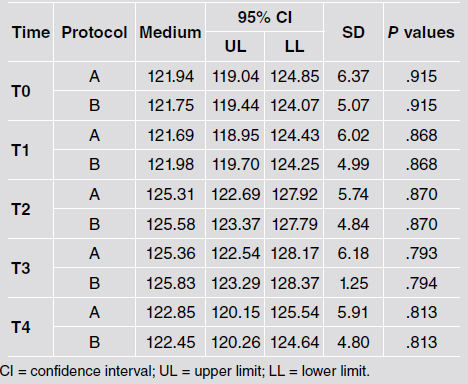
Regarding pain and use of analgesics, patients reported no pain episodes at T1 and T4. Therefore, only the data obtained at T2 and T3 were included in the statistical tests. There was no difference between protocols A and B for pain evaluation (p = .909). In the evaluation of the amount of analgesic medication used, there was a lower consumption of analgesics at T2 when Protocol A (p= .022) was used (Table 2). Protocols A and B were compared, and no statistically significant difference was found between groups (p=.837). There was a difference between the times for both protocols tested in an inter-group evaluation, with T0 and T4 presenting some difference (p=.01). A more significant difference was found when T2 and T3 were compared to T0, T1 and T4 (p<.001) (Fig. 3). Table 3 shows descriptive statistics and p values for protocol A and B comparisons over time. When protocols A and B were compared, there was no statistical difference (p=.958) for post-surgical swelling. In an intra-group evaluation, the difference in the means of facial measurements between the times was significant, with the greatest difference found when T1 was compared to T2 and T3 (p<.001). The values at T0 and T1 were very close, as there had not been enough time for a significant swelling to form. In the evaluation of the 7-day postoperative evolution, the swelling had reduced to almost initial measurements (Fig. 4). Table 4 shows descriptive statistics and P values for protocols A and B comparisons over time.

Fig. 3 Graphic representation of the variation in range of mouth opening (mm) during the postoperative period of impacted lower third molar surgeries (at times T0, T1, T2, T3 and T4), using two LLLT protocols.
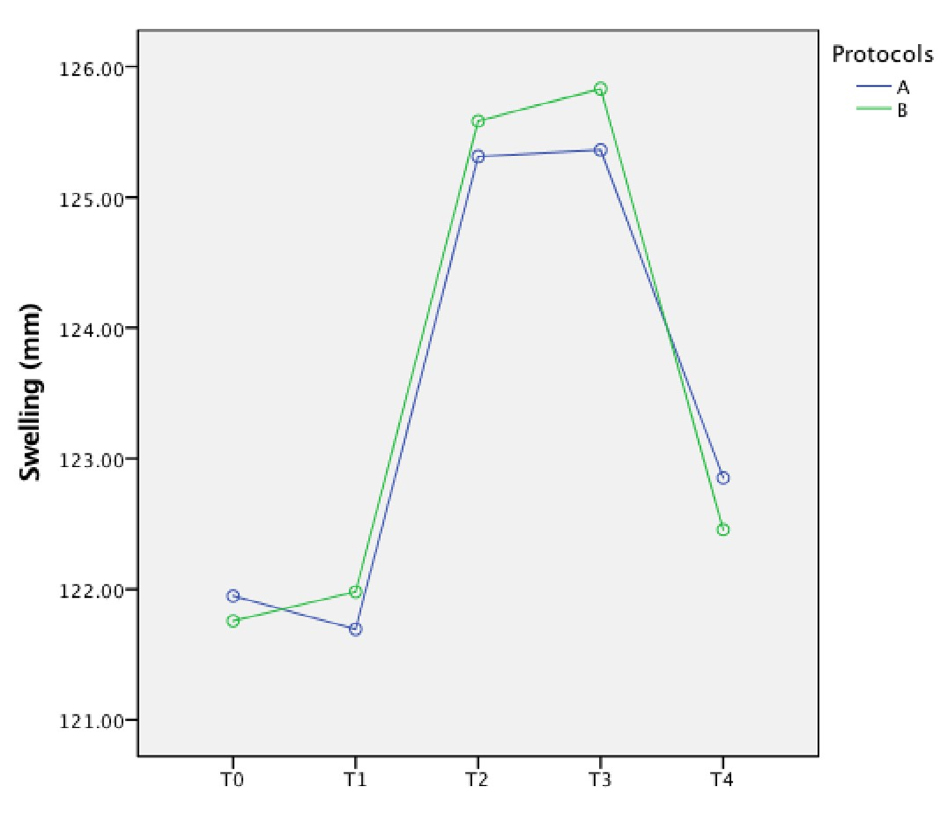
Fig. 4 Graphic representation of the variation in facial swelling (mm) in postopertive surgery of impacted lower third molars, at times T0, T1, T2, T3 and T4, using two LLLT protocols.

Table 2 Evaluation of the amount of analgesic medication used in the postoperative period of impacted lower third molars

Table 3 Evaluation of trismus measured in the range of mouth opening in mm during the postoperative period of impacted lower third molar surgeries, using two LLLT protocols
DISCUSSION
This study shows no critical difference between LLLT applied in one or three times. Although protocol A leads to less use of analgesics, it was not relevant for swelling and trismus.
Concerning methodology, panoramic radiography of the jaws was used to evaluate and classify the third molar positions and surgical planning. According to Guerrero et al. 9 , other imaging tests are not needed for this type of surgery. Careful radiological planning followed by an adequate surgical approach is essential for a good resolution of cases, irrespective of whether 2D or 3D preoperative images are used 10 . Postoperative swelling is mainly influenced by the surgical protocol used, and the length of time and degree of difficulty involved in the surgery 11 . In addition, the surgical technique used to remove impacted third molars affects the quality of the postoperative period, with some studies showing the importance of the care that must be taken with each step of the procedure 12, 13 . To reduce bias in our study, a Split-Mouth design trial with a standardized surgical protocol was performed by a dental surgery specialist. The surgeries were conducted in the most atraumatic manner possible and resulted in lower levels of swelling and pain associated with laser therapy treatment. Similar measures of care have also been adopted in various comparable studies 14, 15 . There is consensus on the prescription of preemptive or therapeutic antibiotics in cases where the patient has a systemic or local condition leading to an infection that might develop or worsen with third molar surgery 15, 16 . However, studies show that if a good surgical technique is used and the aseptic chain is maintained, there is no need to use antibiotics in third molar surgeries 12 . Based on that evidence, antibiotics were not used in this study, as the patients presented neither local nor systemic conditions which would have justified such use.
Postoperative care is crucial in reducing the discomfort caused by the surgical procedure. Pain, trismus and swelling are complications resulting from the inflammatory processes which occur after third molar surgery. Drugs are recommended to minimize the inflammatory response 1,2,13, 17 . However, although medication is satisfactory in relieving pain, it also has adverse effects 16 . Adjuvant therapies, such as laser therapy, have been used to enhance postoperative comfort while at the same time reducing drug consumption 1-4,7, 14 .
The analgesic medication of choice used by patients who underwent surgery was Paracetamol 750mg due to its low rate of adverse reactions and its efficacy in controlling postoperative pain, even though it does not have a high degree of analgesic potential 13 . Other therapies to control inflammatory reactions were not adopted in this study so that more precise answers regarding the effects of LLLT could be obtained. The placebo was used specifically to evalúate the role of single or three LLLT applications.
Regarding pain, it was found that the consumption of analgesics was lower at T2 for protocol A compared to the quantity of analgesics used at T2 when protocol B was applied. This agrees with the results reported by Kazancioglu et al} 1 , who also found a lower consumption of analgesics by patients who received LLLT in the postoperative period. Our results indicate that, in general, there was little difference between the protocols used.
Despite the decrease in analgesic consumption at T2 for protocol A, the difference was not statistically significant by VAS assessment. Other authors 7, 18 also found no statistically significant difference in the pain presented by patients when using LLLT. Other studies found a difference in the pain profile of patients who used LLLT in the postoperative period of impacted third molar surgeries compared to the control group 1,2, 19-22 .
Variations in the medication protocols could explain these differences. In the studies by Fernando et al. 1 , Landucci et al 23 , Eshghpour et al} 4 , and Sierra et al. 24 , the protocol used for postoperative medication includedAmoxicillin 500mg for seven days, Ibuprofen 600mg for three days and Chlorhexidine 0.12% mouthwash. Markovic & Todrivic 1, 2 and Amarillas-Escobar et al. 20 administered Dexamethasone in different doses for each group. There was also a difference in the laser therapy protocol. In our study, Paracetamol was prescribed at standard intervals (every six hours for two days). However, the patients were instructed that the medication could be taken at longer intervals if they felt less discomfort or no postoperative pain, and that the interval could be safely reduced in case of more severe pain. Well-established results of pain reduction found in studies on mucositis and other mucosal ulcerations could be related to the superficiality of the lesion 25 . The use of laser in bone alterations, such as postoperative surgery for third molars, demands further research to evaluate the in-depth effect of LLLT 26 .
The trismus evaluation showed no statistical difference in the postoperative period between protocols A and B. Similar results were found in the literature 17,18,20, 21 , which also showed no difference in the trismus evaluation between a single dose of LLLT in the immediate postoperative period compared to applying it in 3 (three) sessions, as occurred in our study. However, different medication protocols and LLLT doses were used. Studies evaluating trismus when LLLT was used in the postoperative period of impacted third molar surgeries, which included groups that did not receive the laser treatment 5, 27-29 , showed positive results with lower trismus in the group where LLLT was applied. This shows that, even though our study found no statistical difference between protocols A and B, the use of LLLT in the postoperative period of impacted third molar surgeries can be beneficial, providing greater post-surgical comfort. The evaluation showed that there was no clinical difference between the protocols when swelling was compared. Of the factors analyzed, swelling seems to respond least to LLLT, a finding also reported in other studies 10,17, 20 .
The difficulty in comparing results published in studies is mainly due to the lack of standardization in the use of LLLT 17, 18 . There are great variations between the technical parameters, time and place of application, and type of laser used. Some apparent benefit has been found, especially in relation to a reduction in trismus and pain, as noted in several studies 4, 27-29 . Further research could contribute to clarify a better cost-benefit ratio of using only one LLLT session in the immediate postoperative period or adding other LLLT sessions to reduce pain.
In conclusion, this study found no difference between applying LLLT in 3 sessions (immediately, 24 and 48 hours after surgery) and applying it only in the immediate postoperative period. We consider that protocol A could be more challenging due to the need to apply it 24 and 48 hours after surgery. Therefore, for practical reasons, a single laser application in the immediate postoperative period could be effective to manage postoperative discomfort in lower third molar surgery.