INTRODUCTION
Third molar extraction surgery is a frequent procedure in dentistry, and the prophylactic removal of third molars still lacks consensus regarding risks and benefits 1-7 . However, this procedure may prevent intraoral morbidities such as caries, periodontitis, root absorption of adjacent teeth, pericoronitis, and other oral pathologies 5 . It is also cost-effective considering the treatments that would have been required had the lesions not been prevented 4 . Third molar extraction surgery may cause known complications such as mandibular fracture 1 , paresthesia 3 , postoperative pain, edema, and trismus related to inflammatory responses after surgery 2, 6 .
Temporomandibular disorder (TMD) is a collective term for several clinical problems involving masticatory muscles, temporomandibular joints, and associated structures 8 , which affects about 10% of the adult population 9 . TMD patients usually have chronic orofacial pain, and their masticatory muscles may be more sensitive to mechanical stimuli than in normal patients 10 . Furthermore, parafunctional habits may be associated with more pain experiences after dental extractions due to the pressure applied to tooth and bone structures during surgery 11 .
Although the influence of oral mucosa flap designs on postoperative symptoms is controversial 12, 13 , envelope flaps are usually faster to perform and more often associated with lower oral symptomatology in the extraction surgery of third molars classified as Position A and B according to Pell & Gregory, even though triangle flaps cause fewer alveolar osteitis complications 13 .
Like patients in other chronic pain groups, patients with bruxism often appear to have lower thresholds and tolerance for various types of pain compared to healthy controls 14 . The aim of this study was to analyze postoperative pain in patients with and without bruxism subjected to third molar extraction surgery.
MATERIALS AND METHOD
An observational study was conducted based on the CONSORT statement, with four groups and an allocation ratio of 1:1:1:1., following ethical approval (No. 3.324.037) from the Research Ethics Committee of the Dental Research Center of the Sao Leopoldo Mandic Dental School;Campinas, SP, Brazil. Written informed consent was obtained from all participants before conducting the research.
This study included healthy patients (ASA I -following the classification of the American Society of Anesthesiologists) with absolute or relative need to remove lower third molars, non-smokers, without periodontal disease or history of periodontal disease treatment, and without pulp necrosis or pulpitis in the tooth requiring extraction. Exclusion criteria were postoperative infections, alveolitis, wound healing defects, cases of postoperative hemorrhage that required reintervention or resuture, and patients with incomplete files or who did not understand the Portuguese language well enough to complete the pain questionnaires applied. Bruxism was self-reported by each participant based on signs and symptoms reported in the questionnaire, and confirmed by an expert clinician who considered known bruxism-related clinical features such as tooth wear, temporomandibular joint pain, and masticatory muscle hypertrophy, pain or fatigue.
The research was conducted at the Community Health Center of the State University of Campinas (CECOM-UNICAMP, Campinas, Sao Paulo, Brazil) from January 2017 to November 2019. This is a public health care center that provides a multidisciplinary approach and emergency dental care. Therefore, all patients received treatment for their oral health-related needs, regardless of eligibility criteria.
The four groups included patients 1) without bruxism subjected to third molar surgery only with forceps and levers, 2) with bruxism subjected to third molar surgery only with forceps and levers, 3) without bruxism subjected to third molar surgery with osteotomy and odontosection, and 4) with bruxism subjected to third molar surgery with osteotomy and odontosection. All teeth on both sides should present the same surgical difficulty level evaluated by panoramic radiographs. The use of only forceps and levers or execution of osteotomy and odontosection was based on the prediction of the difficulty of extraction by the oral and maxillofacial surgeon (OABN), who has more than 10 years’ experience.
The same surgeon (OABN) performed the same access technique at the surgical sites of all participants. First, a specific form for this procedure was completed with data related to the surgery, such as the degree of difficulty of the tooth requiring extraction and technique details. Second, all patients received the same technique and surgical sequence.
Intraoral and extraoral antisepsis followed the aseptic chain and basic principles of surgical techniques, and sterile fields were placed on the face of each patient and the surface of the surgical table. Inferior alveolar nerve block and infiltrative anesthesia with local anesthetic of 2% lidocaine with epinephrine (1:100,000) (DFL, Rio de Janeiro, RJ, Brazil) were performed. The mucosa flap was selected. Osteotomies were performed with a high-speed handpiece with #6 spherical drills (Prima Dental by Angelus, Londrina, PR, Brazil) and long-stemmed Zekrya burs (Prima Dental by Angelus, Londrina, PR, Brazil).
Surgery time was measured from the start of the incision to the end of suturing and gauze hemostasis. Irrigation was performed with 100 mL of 0.9% saline solution, suture with simple 4.0 silk thread, and hemostasis with gauze for 30 minutes. All patients received postoperative instructions and were discharged with instructions to schedule a return visit on the seventh postoperative day for reassessment and suture removal.
The oral drug regimen prescribed was 8 mg dexamethasone and 500 mg dipyrone one hour before the procedure, and 4 mg dexamethasone every eight hours for two days and 500 mg dipyrone every six hours for three days in the postoperative follow-up. Mouthwash with 0.12% chlorhexidine digluconate was prescribed, from 24 hours after the end of the procedure until the third postoperative day.
The primary outcome of this study was postoperative pain after third molar extraction surgery in two groups of patients: with and without bruxism. The secondary outcomes consisted of postoperative pain in the two groups with added variables based on the surgical technique used, namely forceps and levers only (ST1) and osteotomy and odontosection (ST2), and variables based on whether an oral mucosa flap had been performed during surgery.
After surgery, primary and secondary outcomes were measured by providing each patient with a questionnaire with seven Visual Analog Scales (VAS), one for each postoperative day until suture removal on the seventh day. The VAS consisted of a 100-mm scale, with zero (left end) meaning “no pain” and 100 mm (right end) meaning “maximum possible pain” 15 . After returning the questionnaire, the filled-out scales were measured with a digital caliper to obtain postoperative pain results in millimeters. Age, sex, treated tooth and surgery time were recorded for all participants.
After applying the eligibility criteria to 340 patients, only 136 were eligible to participate in this study. Each of the four groups was a convenience sample (n=34). Some participants in groups 1 and 2 (n=34) and all participants in groups 3 and 4 (n=68) received an oral mucosa flap. There was a test power of at least 0.80 for the effects of bruxism, type of surgical technique, surgery time, and the interaction between those effects, at a 5% significance level and mean effect size f=0.25 16 . Calculations were performed with the GPower software.
First, the four groups were compared for age and surgery time (Kruskal-Wallis and Dunn test), treated teeth (Fisher’s exact test), and sex (chi-square test). Then, a descriptive and exploratory analysis of pain scores was performed. The non-parametric Mann-Whitney test compared the two techniques and the groups with and without self-reported bruxism. Friedman and Nemenyi non-parametric tests were used for time comparisons. The analyses were performed with the R software at a 5% significance level.
RESULTS
There was no significant difference between the four groups regarding age (p>0.05). Surgery time was significantly longer for the groups subjected to the extraction technique with osteotomy and odontosection (groups 3 and 4), p<0.0001. Fig. 1 presents the surgery time according to technique and the presence of temporomandibular disorder.

Fig. 1 Boxplot of surgery time according to technique and the presence of temporomandibular disorder. ST1: third molar surgery only with forceps and levers; ST2: third molar surgery with osteotomy and odontosection; TMD: temporomandibular disorder.
Regarding pain scores, among patients subjected to the ST1 technique (forceps and levers only), except for the fifth day, the pain score was significantly higher for those with than without parafunction (p<0.05). Among patients subjected to the ST2 technique (osteotomy and odontosection), from the third day onwards, a higher pain score was reported by participants with parafunction (p<0.05). There was only a significant difference between the two techniques for patients with parafunction on the seventh day when the pain score was significantly higher for patients in whom the ST2 technique had been used (p<0.05). Table 1 and Fig. 2 show the pain score according to technique, presence of bruxism, and postoperative day.
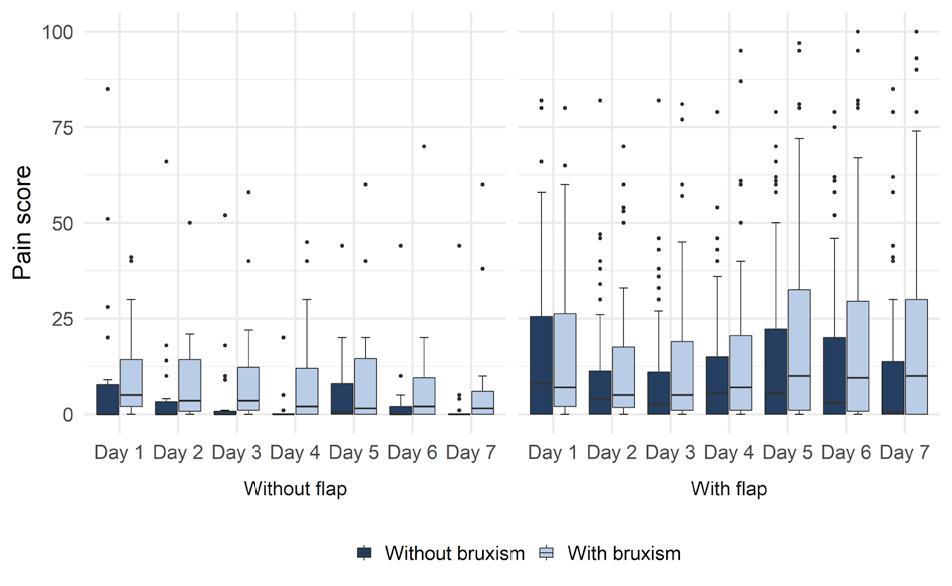
Pain scores were compared between the groups that did or did not receive the flap, among patients subjected to the ST1 technique. For patients without bruxism, the group with the flap had significantly more pain on the fourth day (p<0.05) than the group without the flap. For patients with bruxism, those who received the flap also reported higher pain scores, but in this case, on the fourth, fifth, and sixth days (p<0.05). In the group that did not receive the flap, patients with bruxism had a higher pain score than those without bruxism on the first four days (p<0.05). For the groups that received the flap, there was no significant difference between patients with and without bruxism (p>0.05). Table 2 and Figure 3 show the pain score according to flap performance and the presence of bruxism for the group that received the ST1 technique.
Table 1 Mean (standard deviation) and median (mínimum and máximum valúes) pain score valúes according to technique (with or without ostectomy and odontosection) and the presence or absence of bruxism.
| Bruxism | Day | Group | p-value | |||
| ST1 | ST2 | |||||
| Mean (standard deviation) | Median (minimum and maximum value) | Mean (standard deviation) | Median (minimum and maximum value) | |||
| Without | 1 | 10.3 (17.9) | 3.0 (0.0-85.0) Aa | 16.6 (19.4) | 11.0 (0.0-82.0) Aa | 0.0753 |
| 2 | 6.06 (12.5) | 0.0 (0.0-66.0) Aa | 10.5 (18.0) | 2.5 (0.0-82.0) Aab | 0.2670 | |
| 3 | 6.8 (12.7) | 0.0 (0.0-52.0) Aa | 8.3 (15.2) | 2.0 (0.0-82.0) Aab | 0.3418 | |
| 4 | 5.06 (10.1) | 0.0 (0.0-43.0) Aa | 9.6 (16.9) | 3.0 (0.0-79.0) Aab | 0.1427 | |
| 5 | 7.8 (12.2) | 0.5 (0.0-44.0) Aa | 14.4 (20.9) | 5.5 (0.0-79.0) Aab | 0.2617 | |
| 6 | 6.6 (12.7) | 0.0 (0.0-52.0) Aa | 11.9 (19.0) | 4.0 (0.0-79.0) Aab | 0.1256 | |
| 7 | 6.4 (16.7) | 0.0 (0.0-85.0) Aa | 10.5 (19.0) | 0.0 (0.0-79.0) Ab | 0.2040 | |
| p-value | 0.3656 | 0.0379 | ||||
| With | 1 | 14.4 (16.6) | *5.5 (0.0-53.0) Aa | 16.8 (22.0) | 7.0 (0.0-80.0) Aa | 0.7083 |
| 2 | 10.9 (14.0) | *4.5 (0.0-53.0) Aa | 14.2 (20.3) | 5.0 (0.0-70.0) Aa | 0.7221 | |
| 3 | 11.8 (18.0) | *4.0 (0.0-77.0) Aa | 14.5 (19.1) | *6.5 (0.0-60.0) Aa | 0.5196 | |
| 4 | 12.1 (17.1) | *3.5 (0.0-61.0) Aa | 16.1 (22.0) | *7.0 (0.0-95.0) Aa | 0.4077 | |
| 5 | 14.0 (21.5) | 2.0 (0.0-80.0) Aa | 23.7 (27.1) | *10.0 (0.0-97.0) Aa | 0.0695 | |
| 6 | 13.3 (21.9) | *3.5 (0.0-81.0) Aa | 23.1 (27.4) | *11.0 (0.0-95.0) Aa | 0.1208 | |
| 7 | 10.0 (19.2) | *2.0 (0.0-90.0) Ba | 22.4 (26.4) | *11.5 (0.0-93.0) Aa | 0.0208 | |
| p-value | 0.0646 | 0.5814 | ||||

Fig. 2 Boxplot of pain scores according to technique, the presence of temporomandibular disorder, and postoperative day. ST1: third molar surgery only with forceps and levers; ST2: third molar surgery with osteotomy and odontosection; bruxism.
Table 2 Mean (standard deviation) and median (mínimum and máximum valúes) of pain score valúes according to use of a flap and the presence or absence of bruxism for the group that received the ST1 technique.
| Bruxism | Day | Flap | p-value | |||
| Without | With | |||||
| Mean (standard deviation) | Median (minimum and maximum value) | Mean (standard deviation) | Median (minimum and maximum value) | |||
| Without | 1 | 11.0 (22.9) | 0.0 (0.0-85.0) Aa | 9.4 (10.6) | 6.0 (0.0-33.0) Aa | 0.1425 |
| 2 | 6.3 (15.9) | 0.0 (0.0-66.0) Aa | 5.8 (7.7) | 3.5 (0.0-26.0) Aa | 0.2079 | |
| 3 | 5.0 (12.7) | 0.0 (0.0-52.0) Aa | 8.9 (12.8) | 3.0 (0.0-43.0) Aa | 0.0845 | |
| 4 | 1.4 (4.8) | 0.0 (0.0-20.0) Aa | 9.1 (12.8) | 3.0 (0.0-43.0) Aa | 0.0577 | |
| 5 | 6.3 (11.3) | 0.5 (0.0-44.0) Aa | 9.5 (13.3) | 1.0 (0.0-43.0) Aa | 0.6538 | |
| 6 | 3.8 (10.4) | 0.0 (0.0-44.0) Aa | 9.7 (14.6) | 0.0 (0.0-52.0) Aa | 0.4794 | |
| 7 | 3.0 (10.3) | 0.0 (0.0-44.0) Aa | 10.2 (21.6) | 0.0 (0.0-85.0) Aa | 0.3170 | |
| p-value | 0.3303 | 0.9392 | ||||
| With | 1 | 11.2 (12.7) | *5.0 (0.0-41.0) Aa | 18.8 (20.6) | 9.5 (0.0-53.0) Aa | 0.5756 |
| 2 | 9.2 (12.2) | *3.5 (0.0-50.0) Aab | 13.4 (16.4) | 5.5 (0.0-53.0) Aa | 0.5174 | |
| 3 | 10.7 (15.2) | *3.5 (0.0-58.0) Aab | 13.4 (22.1) | 4.0 (0.0-77.0) Aa | 0.9164 | |
| 4 | 10.4 (16.2) | *2.0 (0.0-45.0) Aab | 14.4 (18.8) | 6.5 (0.0-61.0) Aa | 0.1564 | |
| 5 | 9.4 (16.0) | 1.5 (0.0-60.0) Aab | 20.6 (26.9) | 8.5 (0.0-80.0) Aa | 0.1370 | |
| 6 | 8.4 (16.0) | 2.0 (0.0-70.0) Aab | 20.3 (27.4) | 11.0 (0.0-81.0) Aa | 0.0965 | |
| 7 | 7.2 (15.1) | *1.5 (0.0-60.0) Ab | 14.0 (23.9) | 6.0 (0.0-90.0) Aa | 0.2858 | |
| p-value | 0.0498 | 0.6012 | ||||
DISCUSSION
Some limitations of this study must be acknowledged, such as the fact that bruxism diagnosis and severity, and chronic orofacial pain were self-reported. Nevertheless, bruxism was confirmed based on related clinical features. Additionally, the third molar position classification was not recorded, and postoperative instructions, drug regimen, and pain questionnaire responses were highly patient-dependent and without professional supervision. Therefore, sample standardization and data collection were biased.
One of the main steps to approach patients in this study was anamnesis, by collecting sufficient data to establish a proper diagnosis and treatment plan. The surgical techniques selected were based on patient characteristics and radiological aspects of third molars. This perioperative protocol may help predict the steps to manage each case appropriately 17 . The pain questionnaires included the VAS, which is a reliable, valid tool for assessing postoperative pain in oral procedures 15 .
Postoperative pain levels after lower third molar surgery were higher in patients with than without bruxism for both surgical techniques (p<0.05). Considering the higher sensitivity in cases with parafunction 10 , patients with bruxism should be managed carefully with a proper drug regimen and postoperative instructions to reduce symptomatology.
The comparison between surgical techniques showed significantly higher pain levels only on the seventh day for the osteotomy and odontosection groups (p<0.05). Therefore, both techniques are viable, and the benefits of performing osteotomy and odontosection may exceed the postoperative effects when correctly selected for a treatment plan based on previous criteria 17 .
Moreover, persistence and pain levels were not significantly higher in patients subjected to oral mucosa flap incisions (p>0.05). This means that professionals may perform flaps if needed 13 , improving visibility during surgery and tissue mobility for suturing. Bruxism, osteotomy, and odontosection may increase postoperative pain levels, whereas performing an oral mucosa flap did not show significant differences in symptomatology. However, these preliminary data should be interpreted carefully. Randomized controlled trials on postoperative pain in patients with bruxism subjected to third molar extraction surgery are required to reinforce the findings of this study.