INTRODUCTION
The dental pulp and periodontium have different communication routes, including, e.g., apical foramen, accessory canals (which are more prevalent in the apical third) and dentin tubules 1 . Scaling, planing and root surface treatment with an EDTA-based conditioner are used in minimally invasive regenerative periodontal procedures. Such treatment may generate pathological communication between the two structures due to interruption of the vascular pedicle or migration of bacteria and/or inflammatory byproducts from deep periodontal pockets, which may generate pulp pathology 2 .
In 2013, De Sanctis conducted a retrospective study to evalúate the influence of regenerative periodontal surgery on pulp vitality status in teeth with defects involving the apical third, concluding that periodontal surgery did not imply risk of pulp necrosis and that it was not necessary to perform a preventive endodontic treatment unless the periodontal lesion surpassed the apical foramen such that the vascular pedicle would be interrupted during instrumentation 3 .
This study agrees with the results published in 2011 by Cortellini and Tonetti following evaluation of 208 teeth (167 vital and 41 non-vital) associated to infraosseous defects treated by guided tissue regeneration (GTR) procedures. Long-term follow-up (5.4 ± 2.8 years) showed that 165 of the 167 teeth were still vital, so it was concluded that despite the high prevalence of lateral canals in the middle and apical thirds, instrumentation of these areas during GTR procedures did not cause pathological changes in pulp vitality status 4 .
In multi-rooted teeth, the presence of deep pockets and loss of attachment are likely to expose lateral canals located at the level of the furcation area 5 . In 2020, Cortellini performed a study to evaluate the outcomes of minimally invasive regenerative periodontal surgery in molars with infraosseous defects combined with furcation lesions, demonstrating that it was possible to achieve clinical improvements at the furcation area level both vertically and horizontally 6 .
To date, there is no published study evaluating the effect of minimally invasive (MIST) regenerative periodontal procedures on pulp vitality. Therefore, the aim of this study was to evaluate the influence of MIST procedures on pulp vitality status in single-rooted and multi-rooted teeth associated to infraosseous defects extending to the middle and apical thirds.
MATERIALS AND METHOD
This retrospective study analyzed the clinical records of patients who received care between August 2018 and August 2019 at the postgraduate program, Department of Periodontics School of Dentistry, University of Buenos Aires (FOUBA). The study was approved by the FOUBA Ethics Committee by resolution No. 938 (CUDAP: EXP-UBA:0088295). Thirty single-rooted and multi-rooted teeth from 14 patients were included in the study. Patients were 10 women and 4 men, average age 41 ±17 years, who met the following inclusion criteria: a) systemically healthy patients without contraindications, with at least one tooth treated by regenerative periodontal surgery, b) surgical procedures included Minimally Invasive Surgical Technique (MIST) described by Cortellini and Tonetti in 20 07 7 and Modified Minimally Invasive Surgical Technique (M-MIST) described by the same authors in 2009 8 and c) teeth were required to have a diagnosis of clinically normal pulp9..
Exclusion criteria: smokers, diabetics, pregnant women, presence of grade III furcation lesions and tooth mobility.
Clinical parameters recorded at 180 days post-surgery:
Probing depth (PD) and clinical attachment level (CAL) were recorded using a North Carolina probe (UNC-15, Hu-Friedy, Chicago, IL, USA) at a pressure of 0.3N. Furcation grade was established according to horizontal Hamp classification 10 using a Nabers probe (Q-2N Nabers, Hu-Friedy, Chicago, IL, USA), degree of tooth mobility was classified using the Miller scale 11 , plaque index per mouth was expressed using the O’Leary index 12 , and bleeding on probing (BOP) was assessed dichotomously (presence-absence) following Cortellini et al. 1993a 13 .
Pulp sensitivity to cold was tested using a dichlorodifluoromethane coolant spray (Endo Icea, Klepp, Argentina), and perirradicular tissue response was tested by percussion and palpation. Radiographic diagnosis: Periapical X-ray was used to evaluate the chamber (anatomical extension of the chamber, presence of pulp calcifications, caries,
existing restorations, and any sign of previous pulp treatment), degree of root apex development, canal (canal anatomy, presence of calcifications and resorptions), and perirradicular tissues (periodontal space and integrity of alveolar cortical plate).
RESULTS
Thirty teeth (21 single-rooted and 9 multi-rooted) were included, of which 14 had defects extending to the middle third and 16 had defects extending to the apical third. Twenty-five teeth were treated with MIST technique and 5 with M-MIST technique.
Baseline pulp diagnosis:
Clinical evaluation and x-rays of all 30 teeth were compatible with clinically normal pulp.
Clinical evaluation: Asymptomatic pulp; response to sensitivity test slight and transitory, absence of response to heat, percussion and palpation. Radiographic evaluation: Chamber, canal and periradicular tissue appearance normal.
Pulp diagnosis 30 days post-surgery:
One tooth presented clinical and radiographic evaluation compatible with acute irreversible pulpitis (Table 1).
Table 1 Case Processing Summary
| N | Percent | ||
|---|---|---|---|
| Cases available for analysis | Event a | 2 | 6.7% |
| Censored | 0 | 0.0% | |
| Total | 2 | 6.7% | |
| Cases dropped | Cases with missing values | 0 | 0.0% |
| Cases with negative time | 0 | 0.0% | |
| Censored cases before the earliest event in a stratum | 28 | 93.3% | |
| Total | 28 | 93.3% | |
| Total | 30 | 100.0% | |
Clinical evaluation: Spontaneous, persistent pain of severe intensity in response to temperature changes (cold), and sensitivity to percussion.
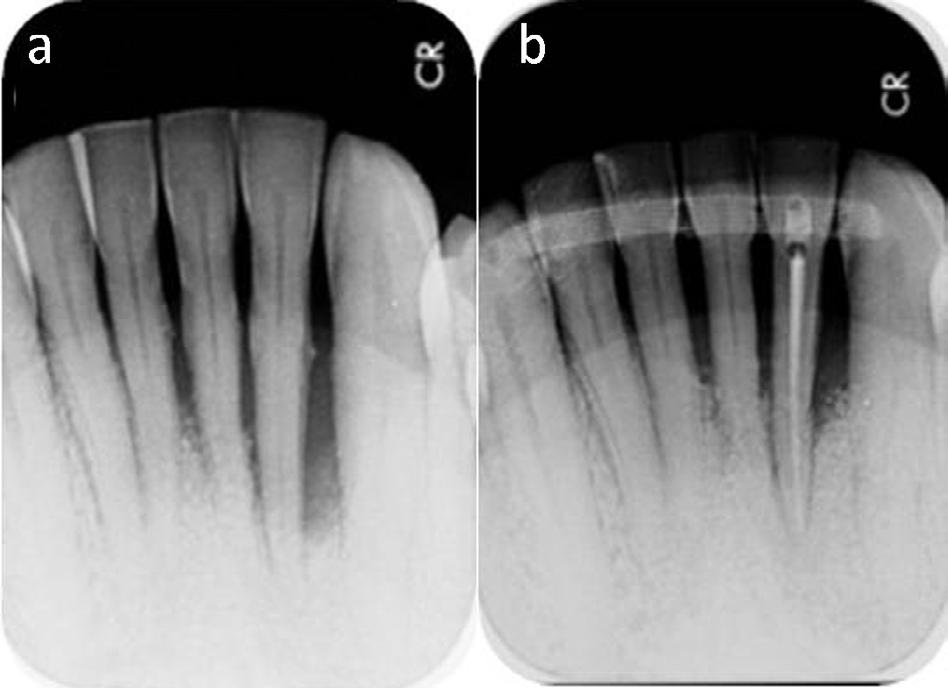
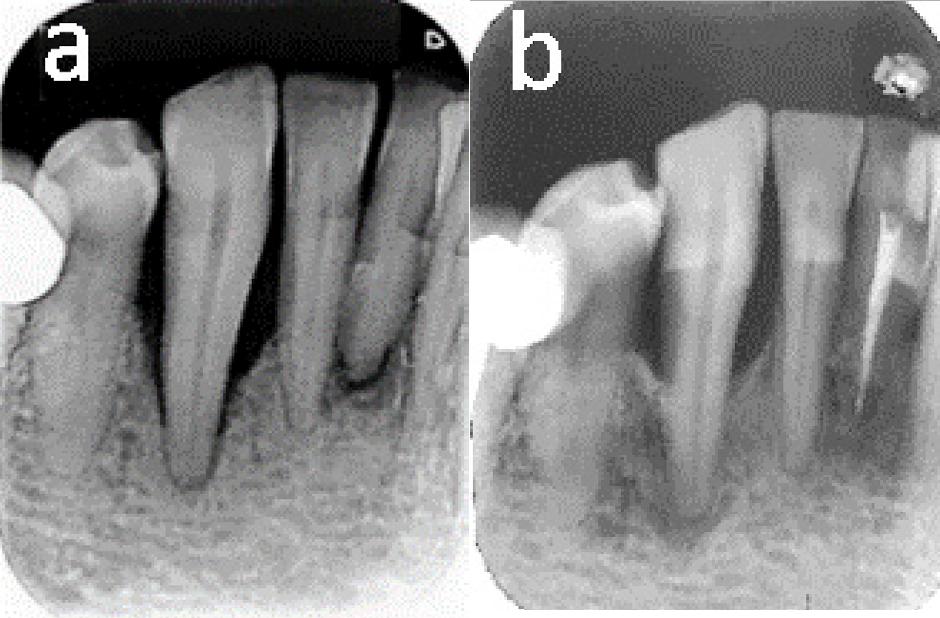
Radiographic evaluation: Chamber and canal appearance normal. Enlargement of periodontal space (Fig. 1a- 1b).
Pulp diagnosis 180 days post-surgery:
One tooth presented clinical and radiological evaluation compatible with pulp necrosis (Table 1). Clinical evaluation: Pulp presents no response to sensitivity test.
Radiographic evaluation: radiolucent image circumscribed at the level of the root apex (Fig. 2a-2b).
Survival analysis:
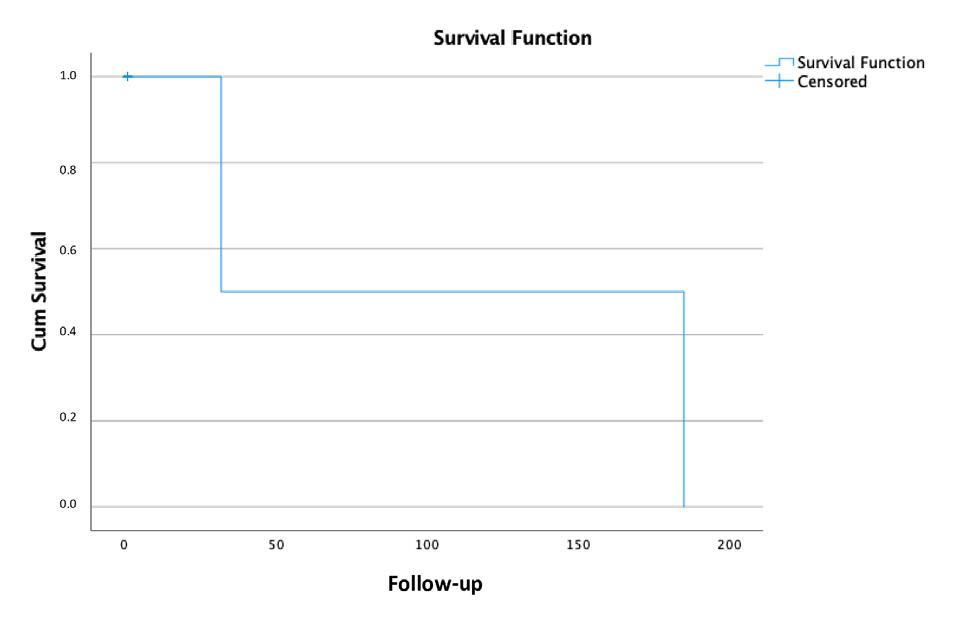
The probability of the teeth treated with minimally invasive regenerative periodontal procedures (MIST, M-MIST) to continue having clinically normal pulp at 180 days post-surgery was 93.3%. For teeth with defects extending to the level of the apical third of the root it was 85.7%, and for teeth with defects extending to the middle third, including presence of furcation lesions, it was 100% (Fig. 3). With a confidence level of 95%, we can say that the mean survival of a tooth treated by minimally invasive regenerative procedures was 105 days with a minimum time of 0 and a maximum time of 252 days.
DISCUSSION
This study evaluated pulp vitality at 180 days post-surgery in 30 teeth treated with MIST. Pulp vitality was determined clinically and radiographically. Pulp sensitivity to cold was tested using a dichlorodifluoromethane coolant spray (Endo Ice), and response of periradicular tissues was tested by percussion and palpation. Pulp sensitivity to cold was used because it is highly precise method for diagnosing necrotic pulps, and more sensitive than the electricity test 14 used in other studies.
Only two out of the 30 teeth presented changes in pulp status following regenerative periodontal procedure. They were both single-rooted and presented bone defects of two walls extending to the apical third, and were treated using MIST. One of them (lower incisor) presented irreversible pulpitis at 30 days, while the other (lower canine) presented necrosis at 180 days post-surgery. The risk rate for changes in pulp vitality was 6.7% (Table 1).
None of the 9 multi-rooted teeth with grade I and II furcation lesions presented changes in pulp status. Indeed, eight of them presented improvement in their horizontal component (Table 2, Fig. 4a-4b).
Table 2 Furcation lesions
| FURCATION LESIONS | ||
|---|---|---|
| LOCATION | BASELINE | 6 MONTHS |
| UPPER JAW (0/I/II) | (0/1/2) | (1/2/0) |
| LOWER JAW (0/I/II) | (O/1/5) | (4/2/0) |
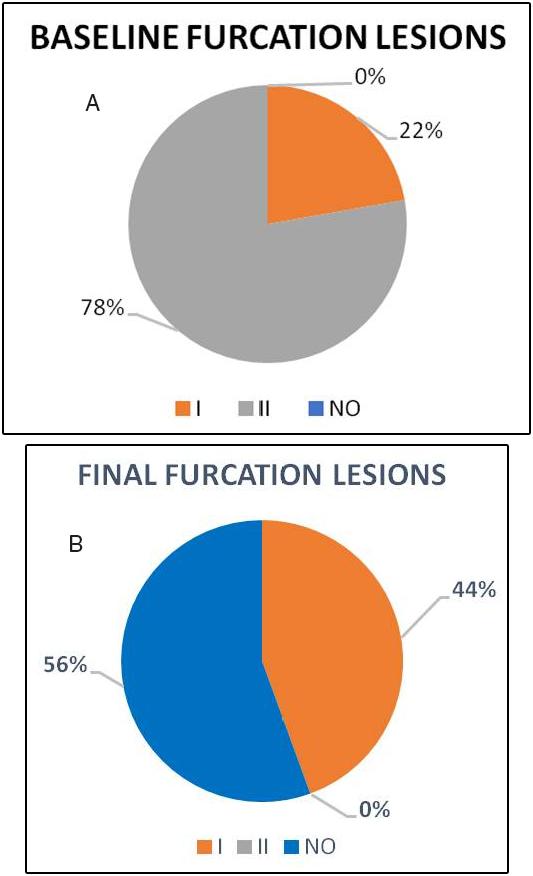
Fig. 4 a) Baseline furcation lesions according to Hamp’s classification. 78% had grade II furcation lesions (7 teeth), and the remaining 22% (2 teeth) had grade I furcation lesions. b) Final furcation lesions according to Hamp’s classification. 56% present no furcation lesion (5 teeth), and the remaining 44% had grade I furcation lesions (4 teeth).
These results agree with the retrospective study published by De Sanctis 3 in 2013. Said study evaluated pulp vitality in 137 patients with teeth with defects extending to the apical third, finding no statistically significant association between the number of teeth that lost vitality and the surgical procedures performed. It concluded that preventive endodontic treatment is not necessary in compromised teeth that will undergo regenerative surgery.
CONCLUSIONS
Although the number of cases analyzed in this study is small, we can conclude that the probability of single-rooted and multi-rooted teeth treated by minimally invasive regenerative periodontal procedures (MIST, M-MIST) continuing to have clinically normal pulp at 180 days post-surgery was 93.3%. For teeth with defects extending to the level of the apical third of the root it was 85.7%, and for teeth with defects extending to the middle third, including furcation lesions was 100% (Fig. 3).