Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista argentina de cirugía
versión On-line ISSN 2250-639X
Rev. argent. cir. vol.112 no.4 Cap. Fed. dic. 2020
http://dx.doi.org/10.25132/raac.v112.n4.1456.ei
Articles
Bile duct injury after cholecystectomy: the experience of Hospital José Ramón Vidal de Corrientes
1 Servicio de Cirugía General, Hospital José Ramón Vidal, Corrientes Argentina
Introduction
Bile duct injury is nowadays a serious health problem. Most lesions occur during laparoscopic surgery which is a common tool among surgeons in current practice1.
The first cholecystectomy was performed by Langebuch in 1882. In 1891, Sprengel described the first side-to-side choledochoduodenostomy after bile duct injury. One year later, Doyen described the end-to-end anastomosis of the bile duct to repair a totally sectioned common bile duct. In 1905, Kerh repaired two cases of bile duct injuries using end-to-end anastomosis without drainage of the duct2.
Although not statistically significant, the incidence of bile duct injuries during laparoscopic cholecystectomy is twice more common than during an open procedure (0.6% vs. 0.3%)
The two most frequent scenarios are bile leak and bile duct obstruction. Most of bile duct injuries after laparoscopic cholecystectomy are recognized in the immediate postoperative period3. Many patients with this complication may require long and complex surgeries4.
The aim of this study is to report our experience in repairing bile duct injuries, and how we manage this complication. As our institution is a referral center in the province, our surgical volume is mostly represented by biliary surgery (65% of the total surgeries per year). We also analyzed morbidity and mortality related with the procedure, and the incidence of this condition in our institution.
Material and methods
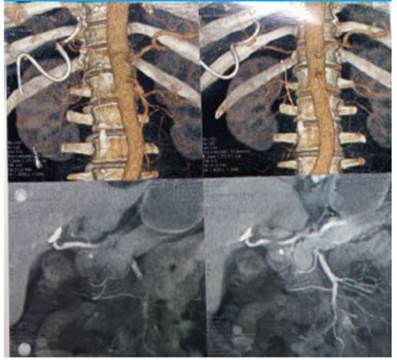
We conducted a retrospective and descriptive study. The information was retrieved form the medical records of 19 patients 9 patients with bile duct injury hospitalized at the Hospital José Ramón Vidal in Corrientes, Argentina, between January 2011 and July 2019. The cohort was made up of seven men and 12 women (Figure 1) between 18 and 72 years. Bile duct injuries occurred during open surgery in 9 patients (47.36%) and during video-assisted laparoscopic procedures in 10 patients (52.63%) (Figure 2). All the cholecystectomies were scheduled procedures. No vascular lesions were reported. In five cases the injury occurred in our institution: three were identified during surgery and two of these were repaired within the same procedure. The remaining case required stent placement and endoscopic dilation. Two injuries were identified in the postoperative period: one was resolved by endoscopic retrograde cholangiopancreatography (ERCP) and the other patient required reconstructive surgery (hepaticojejunostomy). The other patients were transferred from other institutions of our province which lack surgeons with expertise in laparoscopic surgery. A previous repair was not attempted in any of these patients. The anatomy of the injury was evaluated with percutaneous transhepatic cholangiography (PTC) (Figure 3), magnetic resonance cholangiopancreatography (MRCP) and computed tomography angiography (CTA) (Figure 4) with vascular reconstruction of the hepatic hilum (Figure 5). The lesions were classified using the Strasberg classification (Figure 6).

Figure 3 Cholangiography performed through the percutaneous drain. See the absence of filling of the distal bile duct

Figure 4 Colangioresonancia, Nótese sección total de la vía biliar distal. Colec tor de sector posterior derecho seccionado.

Figure 6 Clasificación de Strasberg. Arriba de izquierda a derecha. Strasberg A: Fuga de conducto cístico o pequeño conducto biliar del lecho hepático. Strasberg B: oclusión de un conducto hepático derecho aberrante. Strasberg C: Sección sin ligadura de conducto hepático derecho aberrante. Strasberg D: Lesión lateral de vía biliar principal. Abajo:Strasberg E1: Sección total distal a la confluencia >2cm. Strasberg E2: Sección total distal a la confluencia <2cm. Starsberg E3: Lesión hiliar con preservación de la confluencia. Strasberg E4: Lesión hiliar con afectación de la confluencia y pérdida de comunicación entre hepático derecho e izquierdo. Strasberg E5: Lesión de conducto hepático derecho sectorial aberrante solo o asociado a estenosis del conducto hepático principal.
Results
The results are summarized in Table 1. A Roux-en-Y hepaticojejunostomy (RYHJ) was performed in 12 patients, double hepaticojejunostomy in two patients, and two patients were treated with end-to-end ductal anastomosis with suture over a T tube (Figure 7). The anastomoses were performed intraoperatively in two cases of injuries that occurred in our institution. In the remaining patients, the procedures were performed between 6 and 8 weeks after the injury, using absorbable monofilament suture (polyglycolic acid 4-0). A transanastomotic drain was placed in three patients who underwent RYHJ through an orifice created at the antimesenteric side of the Roux-limb (Figure 8). All the reconstructions were made by open surgery via a right subcostal incision. Three of the patients undergoing surgery developed stenosis of the anastomosis, which was resolved by percutaneous balloon dilation in three sessions; one patient presented bleeding after the initial percutaneous drainage. Complications occurred in 26.3% of the patients and there were no deaths. The patients were referred to our institution between 10 and 60 days after cholecystectomy (mean 19.5 days). Eighteen patients (94.7%) developed jaundice. All the patients with percutaneous drainage or transanastomotic drainage underwent control cholangiography. The trasanastomotic drain was removed three months after surgery. All the patients were discharged with ursodeoxycholic acid (600 mg/day) and were followed-up and monitored with cholangiography and laboratory tests. Three patients underwent ERCP with stent placement and dilation. Stitches were removed 10 days after discharge. Follow-up visits were scheduled at 30 and 90 days, 6 months and once a year with laboratory tests and imaging tests, as applicable.
Discussion
Bile duct injury represents a serious health problem for patients and surgeons. Despite the experience gained with laparoscopic cholecystectomy, the incidence is 0.03-0,6% in most experienced centers5, and 0.08% in our institution6.
Anatomic anomalies, local pathology, and poor surgical techniques are the main causes7.
Anatomic factors include cystic duct anomalies (high or low insertion, short duct or parallel course of cystic duct with the common bile duct) sectoral duct anomalies (in 20% of the cases one of the sectoral duct join the common hepatic duct), intrahepatic gallbladder and vascular anomalies (accessory right hepatic artery). Local pathology includes acute cholecystitis, scleroatrophic cholecystitis, Mirizzi syndrome, chronic cholecystitis and frozen Calot’s triangle. Difficult in terms of technique includes casual attitude towards a “simple gallbladder”, improper placement of trocars, bulky and hanging falciform ligament, bulky quadrate lobe, exaggerated or inadequate use of clips to control bleeding, injudicious use of electro cautery in Calot’s triangle, surgeons’ experience and the learning curve effect8.
Hepaticojejunostomy is the preferred procedure for most bile duct injuries9.
We believe surgeons should be trained in minimally invasive surgical procedures before performing a new laparoscopic technique10.
There are several classification systems of bile duct injury11.The Strasberg classification seems to be the most adequate and easiest to understand despite it does not describe additional vascular involvement. Classification of the injury is done with imaging tests as MRCP, PTC or ERCP3.
The management of a bile duct injury after cholecystectomy costs between 4.5 and 26 times the cost of an uncomplicated laparoscopic cholecystectomy, with significant impact on hospital costs12,16,17.
Imaging tests are essential to establish the diagnosis, define the extent of the injury and plan an appropriate intervention. These tests include ultrasound (US), computed tomography (CT) scan, MRCP, ERCP, and PTC13.
The consequences of an iatrogenic lesion can be serious14.15.
Several methods have been recommended to prevent bile duct injury after surgery: avoid the use of energy device to prevent heat dissection near the main bile duct, knowledge of bile duct anatomy, use of the infundibular technique, critical view of safety described by Strasberg and intraoperative cholangiography, among others18.
If the responsible surgeon is not qualified to repair the injury, he or she must place an external drain into the bile duct making the smallest dissection possible of the hepatic hilum. If the bile duct cannot be drained, several drains should be placed in the Morrison’s space and in the right parietocolic gutter and then the patient should be transferred19,20.
In the United States, most bile duct injuries are repaired in the same institution and by the same surgeon21.
The surgical technique consists of resecting the fibrous tissue scars and inflammatory tissue around the common bile duct immediately after the stricture until reaching the normal mucosa of the duct, trying not to mobilize the ducts too much so as not to generate ischemia that will produce a new stenosis22.
The lack of experience of surgeons, inadequate equipment, patient’s body constitution, aberrant anatomy and inflammation are considered the main risk factors.
In conclusion, bile duct injury may be a common complication after conventional or laparoscopic cholecystectomy. There are many ways to prevent this complication. There are no reliable statistical data on the condition in our country. Among the several classification systems of bile duct injury, we believe that the Strasberg classification is the most useful.
Our institution has a training center in laparoscopic surgery for residents and continuous training for staff surgeons. Our residents’ training is progressive, and they perform increasingly complex procedures.
The main goal of cholecystectomy should be to avoid bile duct injury. Partial cholecystectomy and cholecystostomy should be considered as options in case of frozen or complex gallbladder hilum.
Our prevalence is similar to the one reported by the international literature; nevertheless, we are still working to reduce it. Our morbidity and mortality rate after bile duct repair is adequate.
In case of bile duct injury after cholecystectomy, the recommendation is to place a drain tube and then transfer the patient to a center with surgeons experienced in repairing this complication.
Referencias bibliográficas /References
1. Jabłońska B, Lampe P. Recontructive Biliary Surgery in the Treatment of Iatrogenic Bile Duct Injuries, New Advances in the Basic and Clinical Gastroenterology, Prof. Tomasz Brzozowski (2012) (Ed.), ISBN: 978-953-51-0521-3, InTech, Available from: http://www.intechopen.com/books/new-advances-in-the-basicand-clinical-gastroenterology/reconstructive-biliary-surgery-in-the-treatment-of-iatrogenic-bile-duct-injuries [ Links ]
2. Wilks A, Berri A. Relato oficial. Lesiones quirúrgicas de la vía biliar. Rev Argent Cirug. 1978;Número extraordinario. [ Links ]
3. Mercado MA, Domínguez I. Classification and management of bile duct injuries. World J Gastrointest Surg. 2011; 3(4):43-8. [ Links ]
4. Mercado MA, Chan C, Tielve M, Contreras A, Gálvez-Treviño R, Ramos-Gallardo G, Orozco H. Lesión iatrogénica de la vía biliar. Experiencia en la reconstrucción en 180 pacientes. Rev Gastroenterol Mex. 2002;. 67(4). [ Links ]
5. Kwangsik C. Recent classifications of the common bile duct injury. Korean J Hepatobiliary Pancreat Surg. 2014;18:69-72. [ Links ]
6. Segovia JR y cols. Colecistectomía realizada por residentes en el Servicio de Cirugía del Hospital José Ramón Vidal de Corrientes, Argentina. Rev Argent Cirug . 2018;110(4):191-4 . [ Links ]
7. Zhenfeng G, Fangzhang C, Dingyong T. The Clinical Analysis of Bile Duct Injury during Laparoscopic Cholecystectomy. International Journal of Clinical Medicine, 2015; 6: 825-30. [ Links ]
8. Sankar S, Subramanian M. Laparoscopic bile duct injuries-controversies and consensus. Sri Ramachandra Journal of Medicine. 2007; 1 (Issue 2). [ Links ]
9. Conzo G, Napolitano S, Candela G, Palazzo A, Stanzione F, Mauriello C, Santini L. Iatrogenic Bile Duct Injuries Following Laparoscopic Cholecystectomy: Myth or Reality? A Recent Literature Review from 2006 to 2011, Cholestasis, Dr Valeria Tripodi (Ed.), ISBN: (2012). 978- 953-51-0043-0, InTech, Available from: http://www.intechopen.com/books/cholestasis/iatrogenic-bile-ductinjuries-following-laparoscopic-cholecystectomy-myth-or-reality-literature-revi [ Links ]
10. Blanco Benavides P, Fonseca Alvarado JA, Mora Leandro M, Moya Conejo X, Navarro González J, Paniagua González M, Quirós- Montero JF. Colecistectomía laparoscópica y la importancia de un laboratorio de entrenamiento en cirugía mínimamente invasiva, a propósito de su reciente creación en la universidad de costa rica. Medicina Legal de Costa Rica. 2013; 30 (1). ISSN 1409-0015. [ Links ]
11. Kwangsik Chun. Recent classifications of the common bile duct injury Korean J Hepatobiliary Pancreat Surg . 2014;18:69-72. [ Links ]
12. Sampaio JA, Kruse CK, Passarin TL, Waetcher FL, Nectoux M, Ott Fontes PR, Pereira Lima L. Benign biliary strictures: repair and outcome with the use of silastic transhepatic transanastomotic stents. ABCD Arq Bras Cir Dig. 2010; 23(4):259-65. [ Links ]
13. Thompson CM, Saad Ne, Quiazi RR, Darcy MD, Picus DD, Menias O. Management of Iatrogenic Bile Duct Injuries: Role of the Interventional Radiologist. RG 2013; 33 (1). [ Links ]
14. Barbier L, Souche R, Slim K, Ah-Soune P. Long-term consequences of bile duct injury after cholecystectomy. J Visc Surg. 2014; 151: 269-79. [ Links ]
15. Corbelle JL, Ferrero JO, Rosales CD, Amor HH, More M, Rijana R. Lesiones quirúrgicas de la vía biliar, incidencia, tratamiento y resultados alejados de la reparación. Relato Oficial Rev Argent Cirug . 1996;71:217-23. [ Links ]
16. Hofmeyr S, Krige JEJ, Bronman PC, Beningfield SJ. A cost analysis of operative repair of major laparoscopic bile duct injuries. SAMJ 2015; 105(6). [ Links ]
17. Savader SJ, Lillemoe KD, Prescott CA, Winick AB, Venbrux AC, Lund GB, et al. Laparoscopic Cholecystectomy Related Bile Duct Injuries. A Health and Financial Disaster. Ann Surg. 225 ( 3). [ Links ]
18. Claros N, Laguna R, Pinilla R. Estrategias intraoperatorias para evitar la lesión de vía biliar durante la realización de una colecistectomía laparoscópica Rev Med La Paz. 2011; 17(1):5- 15. [ Links ]
19. De Santibañes E, Sivori J, Pekolj J, Ciardullo M, Sendin R, Mazza O, et al. Lesiones de la vía biliar secundarias a colecistectomía laparoscópica. Rev Argent Cirug .1996;70:208-19. [ Links ]
20. Facciuto E, Ruiz P, Verduna G, Facciuto M. Lesiones quirúrgicas de las vías biliares. A propósito de la actual era de la colecistectomía videolaparoscópica. Rev Argent Cirug .1993;64:116-21. [ Links ]
21. Fischer CP, Fahy BN, Aloia TA, Bass BL, Gaber AO, Ghobrial RM. Timing of referral impacts surgical outcomes in patients undergoing repair of bile duct injuries. HPB. 2009; 11:32-7. [ Links ]
22. Gramatica L, Montenegro R, Lada PE, Gramatica L (h), Martinessi V, Badra R, Mercado LA. Las estenosis benignas altas de la via biliar principal. Rev Argent 2000;78:70-6. [ Links ]
23. Bustos S. Relato Oficial: Prevención de la lesión quirúrgica de la via bilar. Rev Arg Res Cir. 2014; Relato Oficial. sección 1-4. [ Links ]
Received: April 16, 2020; Accepted: August 27, 2020











 texto en
texto en